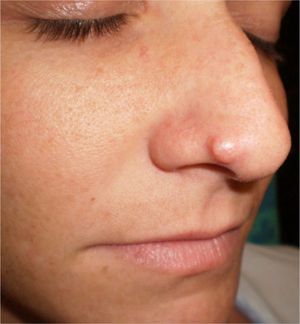
We report the case of an otherwise healthy 27-year-old woman who was seen for an asymptomatic lesion on the right nasal ala that had developed several years earlier. The lesion had begun to grow rapidly over the previous few months.
Physical ExaminationOn physical examination there was a well-defined, firm, skin-colored papular lesion measuring 0.4cm in diameter on the right nasal ala. Several months later, the lesion had increased in size and become a more exophytic, indurated nodule with occasional superficial telangiectasias (Fig. 1).
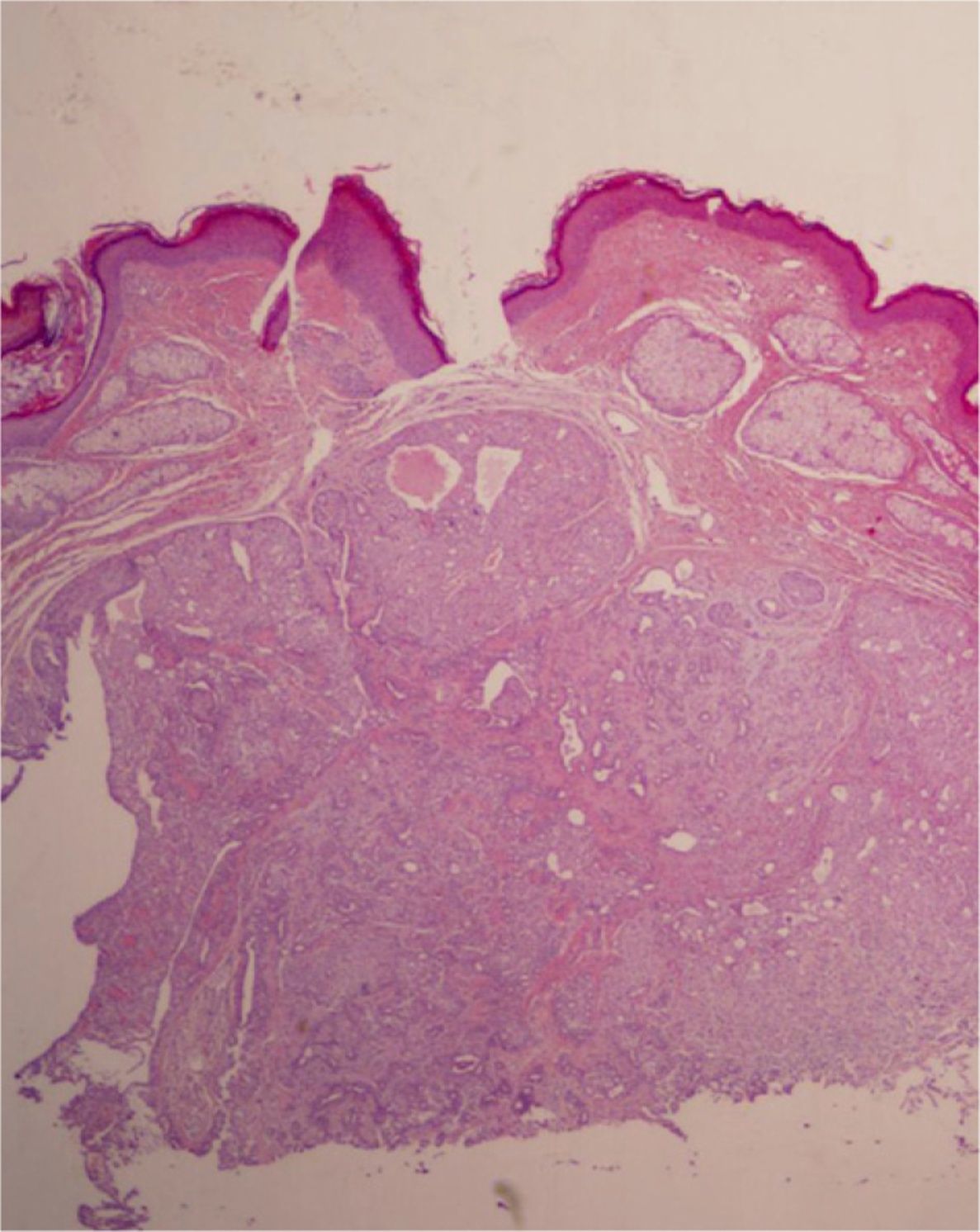
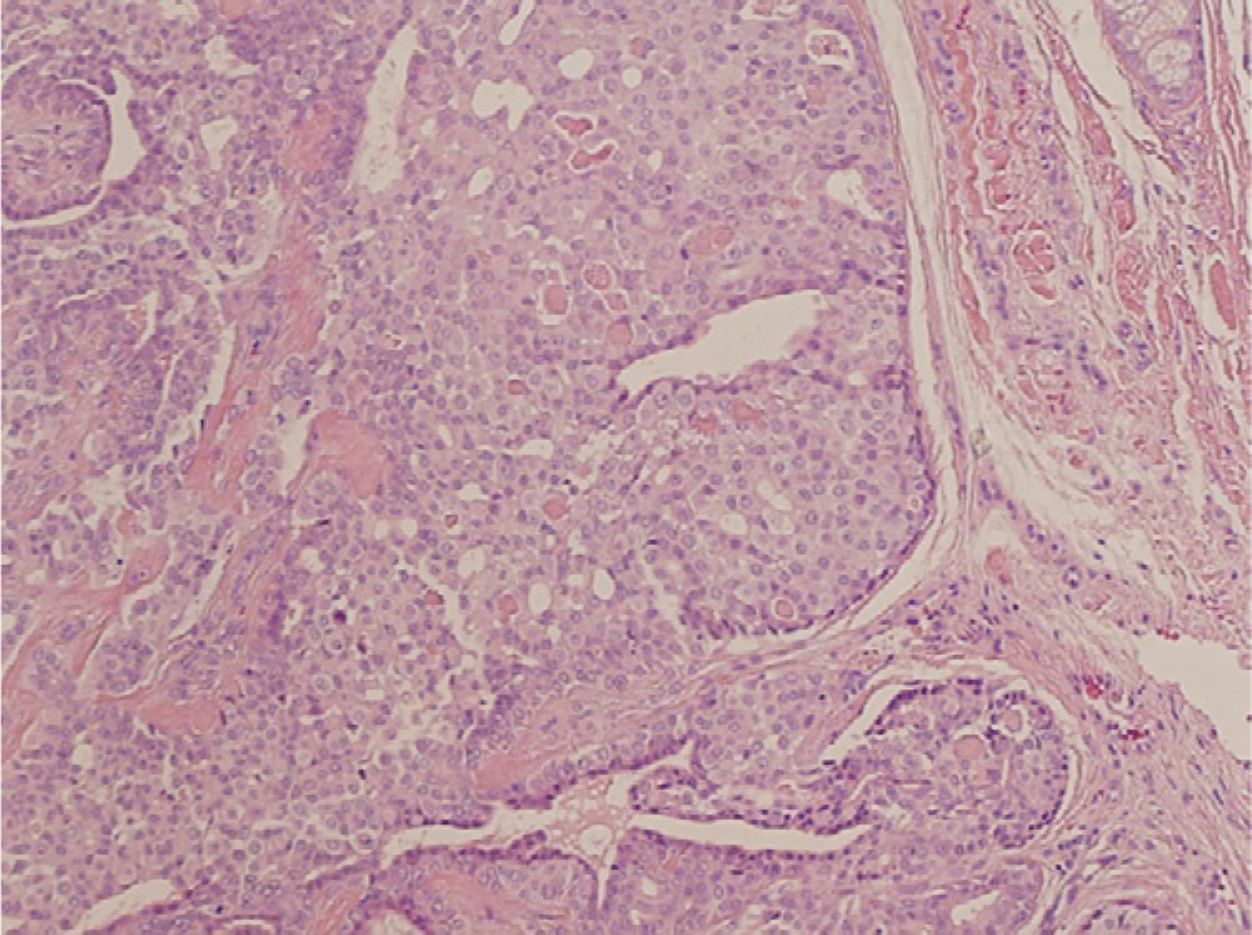
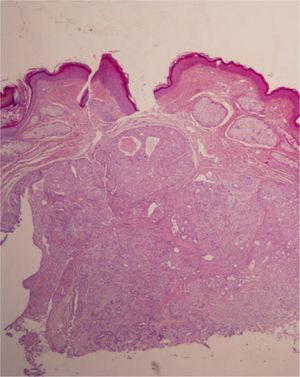
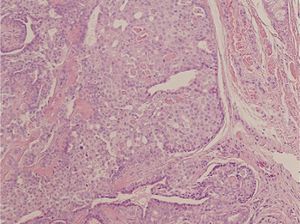
HistopathologyHistopathology revealed a nodular lesion with an expansive growth pattern and well-defined borders (Fig. 2). The lesion consisted of nests of cuboidal epithelial cells without atypia that formed occasional glandular lumina associated with a stroma that was myxoid in some areas (Fig. 3).
What Is Your Diagnosis?
DiagnosisChondroid syringoma (mixed tumor of the skin).
Clinical CourseComplete resolution of the tumor was achieved by excision under local anesthetic.
CommentChondroid syringoma is a rare cutaneous or subcutaneous tumor that presents as a painless, slow-growing lesion that most often arises on the head and neck and typically affects adult men. The size of these lesions ranges between 0.5cm and 3cm in diameter, although they can occasionally be larger.1 They are also known as mixed tumors of the skin because of the histologic similarities with pleomorphic adenoma or mixed salivary gland tumors.1
The term chondroid syringoma was coined by Hirsch and Helwig in 1961, though the tumor was first described by Billroth in 1859 as a nosologic entity with the same histopathological properties as salivary gland tumors. Headington later classified chondroid syringomas as eccrine or apocrine according to their histologic appearance.2
These tumors are generally benign and have an incidence of 0.01% to 0.098% of excised skin tumors.3 No relationship between chondroid syringoma and sun exposure has been reported in the literature despite the predominance of these tumors on sun-exposed areas.1
A rare malignant form of chondroid syringoma has been described in the literature. In contrast to the benign form, malignant chondroid syringoma occurs mainly in women (mean age at onset, 54 years; range, 13-89),4 predominantly on the limbs. Lymphatic and visceral metastases are common, occurring in 42% and 40% of patients, respectively.4 When these types of metastasis develop, they present adenocarcinoma-type characteristics and lose the ability to form chondroid stroma.
Dermoscopy shows no specific features.1
Histology reveals well-defined nests of polygonal cells containing tubulo-alveolar and glandular structures within a fibroadipose, chondroid, myxoid, or hyaline stroma. Periodic acid-Schiff and Alcian blue staining is positive.3,5 The eccrine type presents only 1 layer of cuboidal cells with small lumina, while the apocrine type involves tubular, cystic, ramified lumina lined by 2 layers of cells. Staining is usually positive for cytokeratin, S-100, epithelial membrane antigen, vimentin, actin, glial fibrillary acidic protein, and p63.5 The benign form of chondroid syringoma does not present atypia, mitoses, or pleomorphism and does not recur. However, the malignant form, which does not arise from a previously benign lesion,5 is characterized by cytologic atypia, mitoses, poorly defined borders, satellitosis, and necrosis.3–5 Some authors also refer to an atypical form when the data on malignancy are not conclusive.6
The definitive treatment for these tumors is surgery.1,5 Fine-needle aspiration biopsy can be used for diagnosis before the operation, but excision biopsy is the most useful technique.5 As these lesions are lobular, it is important to include a margin of normal skin to ensure complete excision and avoid recurrence.5 When treating the malignant form, surgery may be combined with adjuvant radiotherapy and chemotherapy, although the efficacy of these therapies has not been demonstrated.4
Please cite this article as: Arango-Duque LC, et al. Lesión asintomática en ala nasal. Actas Dermosifiliogr. 2012;103:827-8.