A 54-year-old man with a history of hypertension on treatment with enalapril and simvastatin consulted for the appearance of an asymptomatic lesion that had appeared on the right frontal region 4 months earlier and that had increased progressively in size. He reported no local trauma or use of topical treatments.
Physical ExaminationAn irregular plaque of normal skin color, measuring 1 x 0.8cm and with a slightly depressed centre was observed; it was formed of small papules following a serpiginous path in the periphery of the lesion. No other lesions of interest were observed on other areas of the body (Fig. 1).
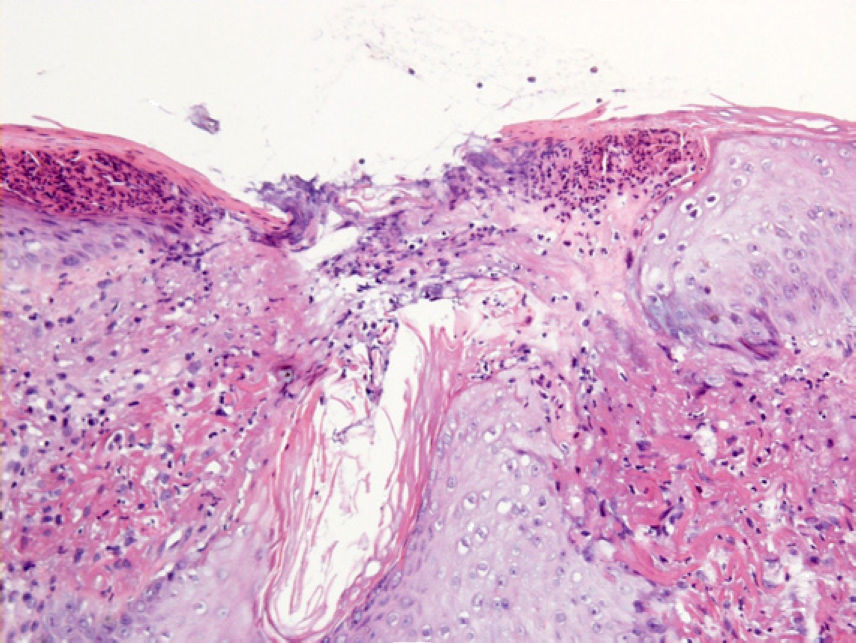
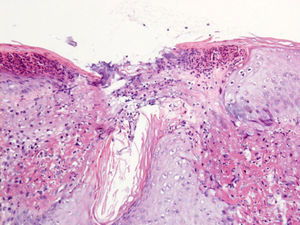
HistopathologyA biopsy taken from the border of the lesion revealed an accumulation of acellular eosinophilic material associated with thick hypereosinophilic elastic fibers in the superficial papillary dermis. There was a moderate inflammatory infiltrate of lymphocytes and plasma cells in the adjacent dermis, with frequent multinucleated giant cells. One area of the overlying epidermis presented a perforation and there was transepidermal elimination of the acellular eosinophilic material associated with small clusters of neutrophils (Fig. 2).
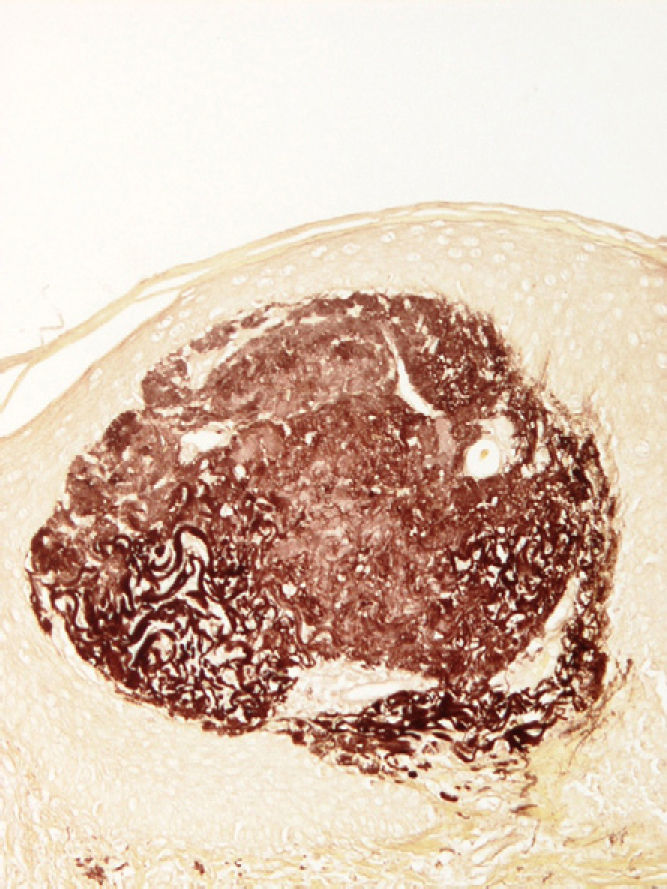
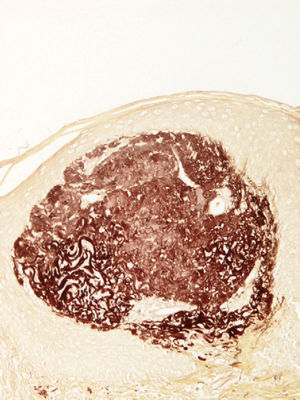
Orcein stain was positive only in the areas with abnormal elastic fibers, including some within the stratum corneum. Orcein stain also revealed altered elastic fibers (Fig. 3).
What Is Your Diagnosis?
DiagnosisElastosis perforans serpiginosa.
Clinical Course and TreatmentTwo sessions of cryotherapy were administered at an interval of 6 weeks. Three months after the second session, the skin on the treated area was slightly atrophied and hypopigmented. At 9 months of follow-up there was no recurrence and no new lesions had appeared.
CommentElastosis perforans serpiginosa is a rare dermatosis caused by the transepidermal elimination of thickened elastic fibers. It has traditionally been classified into 3 types: idiopathic; secondary to treatment with D-penicillamine; and associated with other disorders such as Down syndrome, Marfan syndrome, osteogenesis imperfecta, Ehlers-Danlos syndrome, acrogeria, morphea, Rothmund-Thomson syndrome, and pseudoxanthoma elasticum.1,2 Some familial cases have also been described, with variable inheritance patterns.
The lesions typically appear in early adulthood, with a male to female ratio of 4 to 1.3 Clinically, elastosis perforans serpiginosa consists of the appearance of asymptomatic or slightly pruritic, skin colored or erythematous papules with a central keratin plug; bleeding occurs if the plug is removed. The papules tend to occur in a curvilinear or serpiginous distribution, preferentially on the face, neck, or extremities. The lesions sometimes resolve spontaneously after months or even years, leaving hypopigmented atrophic scars.
Histological features include the presence of abnormal, thickened elastic fibers that are eliminated via transepidermal channels that form grooves in an acanthotic epidermis. A keratin plug can sometimes be observed on the surface, and there many be multinucleated giant cells and a pericanalicular inflammatory infiltrate.4 Specific stains for elastic fibers (Verhoeff-Van Gieson or orcein) show the abnormal morphology of these elastic fibers. In penicillamine-induced cases, slight differences can be seen on optical and electron microscopy.
The etiology and pathogenesis of EPS are unknown. It is thought that the abnormal fibers may be identified as foreign bodies, provoking a granulomatous reaction that results in their elimination. The granulomatous reaction around the elastic fibers may play an important role in the pathophysiology of elastosis perforans serpiginosa, as may the keratinocytes that surround the elastotic material and express the elastin receptor (67-kDa). This receptor could be implicated in the interaction of the keratinocytes with the elastin and its subsequent elimination.5
The clinical differential diagnosis principally includes granuloma annulare, prurigo nodularis, tinea, annular sarcoidosis, cutaneous calcinosis, and porokeratosis of Mibelli. Histopathologically, EPS must be distinguished from congenital reactive perforating collagenosis—a rare genodermatosis usually of autosomal dominant inheritance that typically occurs in association with renal dysfunction or diabetes mellitus—and the acquired forms (Kyrle disease and perforating folliculitis).
Most forms of treatment are unsatisfactory although good cosmetic results have been achieved with cryotherapy,6 electrocoagulation, tazarotene, imiquimod, subcutaneous hydrocortisone, cellophane tape stripping, bichloroacetic acid, carbon-dioxide laser, and oral isotretinoin.
The interesting feature in this case of elastosis perforans serpiginosa is the unusually late onset and presentation in the form of a single lesion. We believe that further lesions may appear in the future despite the good initial response to cryotherapy.
Please cite this article as: Fuentelsaz-del Barrio V, et al. Lesión asintomática en la región frontal. Actas Dermosifiliogr.2011;102:733-734.