A 48-year-old man with skin phototype II and no past history of interest consulted for a lesion in the submandibular region that had appeared 6 months earlier. The lesion was accompanied by occasional pruritus that, interestingly, disappeared after shaving. Physical examination revealed no other skin or mucous lesions and the patient reported no other associated symptoms. The lesions persisted despite treatment with topical antifungal drugs prescribed by his primary-care physician.
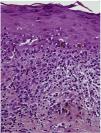
Physical ExaminationThe submandibular region revealed a brownish-violaceous, well-demarcated plaque with raised polylobulated edges, depressed areas of atrophic appearance, and an area of 5×2cm (Fig. 1A). The patient had no palpable local or regional lymph nodes.
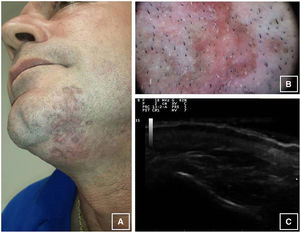
HistopathologyA histologic study of the lesion revealed predominantly lymphocytic lichenoid dermatitis with hyperkeratosis and wedge-shaped hypergranulosis, Civatte bodies, and pigmentary incontinence (Fig. 2).
Other TestsLaboratory tests were normal and serology was negative. Dermatoscopy (Fig. 1B) revealed whiteish-red areas, arciform distribution of uniform brown pigmented structures, and diffuse punctate vessels. No criteria for melanocytic lesions were observed. Skin ultrasound (Esaote® 18Mhz) (Fig. 1C) revealed a thickened hyperechoic epidermal line, a uniform hypoechoic subepidermal band, and echogenicity and normal structure of the subcutaneous cell tissue. Doppler ultrasound was negative.
What Is Your Diagnosis?
DiagnosisAnnular pigmented lichen planus.
Clinical Course and TreatmentThe lesion remained stable despite prior treatment with topical high-potency corticosteroids and daily photoprotection. Slight improvement was observed after 2 months of topical treatment with 0.1% tacrolimus ointment.
CommentLichen planus pigmentosus (LPP) is a rare variant of lichen planus, described by Bhutani et al. in 1974,1 which appears in middle-aged patients, predominantly in women and in patients with dark skin. Although the etiology is unknown, sunlight has been suggested as the main causal agent, given the predominant involvement of photoexposed areas.2 It has been linked to hepatitis C virus and photosensitization to mustard oil or allyl thiocyanate, which is present in fragrances and cosmetics (hair dyes, etc.). The disease initially manifests as small, brown, occasionally pruriginous oval macules that evolve insidiously into diffuse, reticular, patchy, or perifollicular grayish-brown plaques. It is located in photoexposed areas, particularly on the face and neck, although it may also affect the torso and upper limbs. It rarely affects the mucosa or intertriginous regions such as the axillas and inframammary folds.3 Histology reveals vacuolar degeneration of the basement membrane with apoptotic keratinocytes, lymphocytic/histiocytic lichenoid infiltration in bands, and pigmentary incontinence with melanophages in the superficial dermis.3 Cases have been reported of LPP associated with frontal fibrosing alopecia, acrokeratosis paraneoplastica, HVC infection, and nephrotic syndrome. The principal differential diagnosis to consider is erythema dyschromicum perstans (EDP). Presentation of the lesions in areas other than those exposed to sunlight and melanin deposits in the deep dermis allow differentiation between EDP and LPP. Other diseases to include in the differential diagnosis are drug-induced erythema fixum, macular amyloidosis, urticaria pigmentosa, Berloque dermatitis, Riehl melanosis (pigmented cosmetic dermatitis), idiopathic eruptive macular pigmentation, and heavy metal hyperpigmentation. Dermatoscopy is a useful tool for diagnosing LPP.4 Pigmentation in the form of points and grayish-brown globules is observed. Vázquez et al.5 described 3 types of dermatoscopic patterns: punctate, diffuse, and mixed. According to those authors, patients with a greater amount of pigmented granules present a longer course compared to the diffuse pattern, as with our patient. Wickham striae are rare in LPP but not in lichen planus.3 Treatment essentially consists of photoprotection in association with high-potency topical corticosteroids. Treatment with 0.1% tacrolimus ointment produces clinical improvement in half of cases.6 Other less thoroughly documented therapeutic options with a good response include neodymium laser, dapsone, and acitretin. The course is benign, with variable duration and therapeutic response.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Navarro-Triviño FJ, Naranjo-Díaz MJ, Ruiz-Villaverde R. Placa anular pigmentada submentoniana. Actas Dermosifiliogr. 2018;109:911–912.