Erythema annulare centrifugum (EAC) is a rare inflammatory condition. It is one of the figurate erythemas, and is characterized by annular, arciform, or polycyclic erythematous plaques, with or without scales, that enlarge centrifugally with central clearing. It is associated with a variety of diseases and other causes, such as infections, drugs, hormonal or immune alterations, tumors, and stress.1 Some authors believe that EAC is a reactive clinical pattern rather than a clinical-pathologic entity in its own right.2
Annually recurring EAC (AR-EAC) is a very rare clinical form of EAC. While its clinical and histopathologic characteristics are indistinguishable from those of classic superficial EAC, it has a very distinctive clinical course, with lesions appearing on the extremities and recurring annually and seasonally (in the spring and summer). There are no known triggers, and the lesions regress spontaneously after several weeks or months.3
Bernie et al.4 recently described the case of a woman with a large, recurrent, erythematous plaque on her abdomen. As AR-EAC was the main entity in the differential diagnosis, we thought it opportune to report a new case and review the literature.
A 66-year-old man with a history of hypertension presented with slightly pruritic lesions that had appeared on his buttocks and thighs 2 months earlier. There was no fever and his general health was good. He mentioned that this was the fifth summer the lesions had appeared and was unaware of any clear triggers. The lesions resolved spontaneously in autumn, approximately 4 months after onset.
Skin examination showed a series of red-brown annular and arciform plaques on the proximal area of the posterior surface of the thighs and buttocks. The plaques had an erythematous border and collarette scaling at the inner margin (Fig. 1). There were no lesions on the face, hands, feet, trunk, or mucosal surfaces.
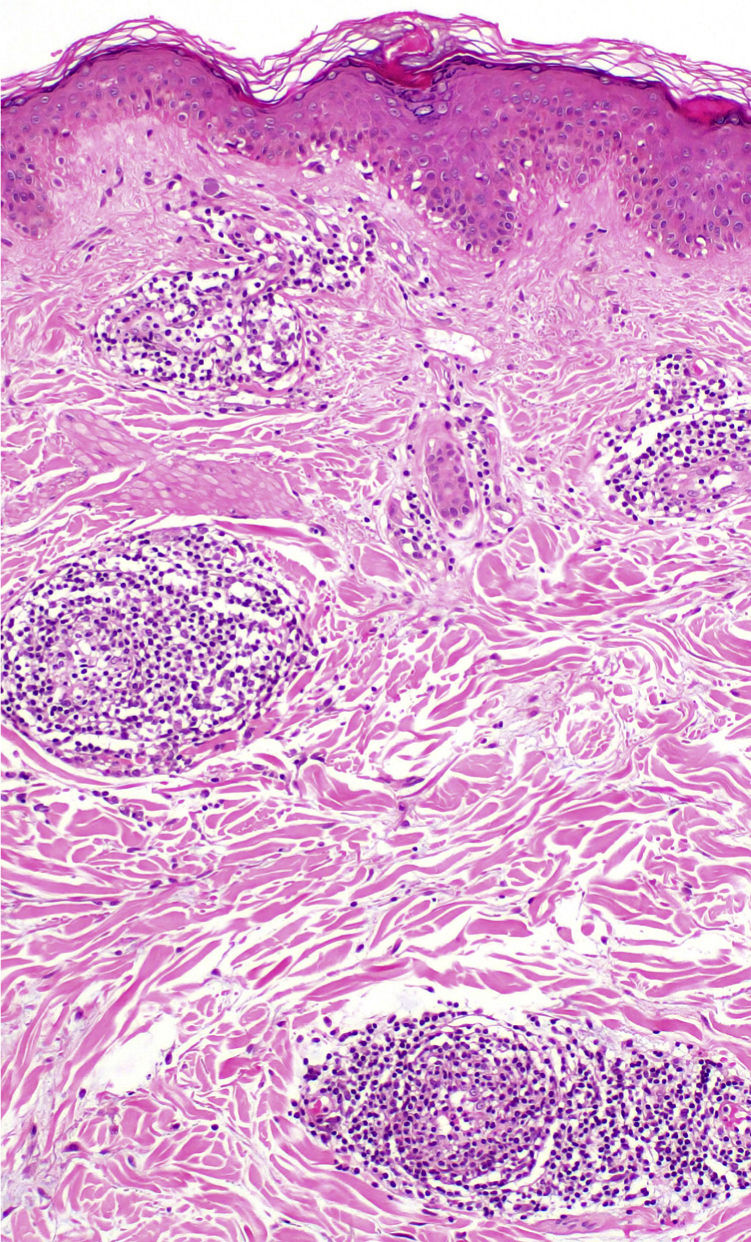
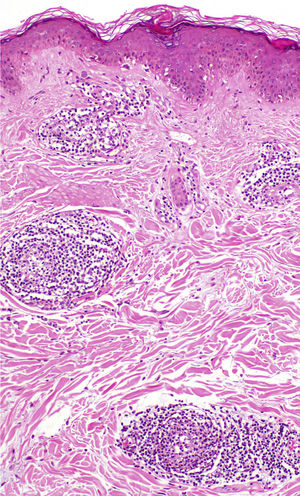
Histopathologic examination of a biopsy specimen taken from a plaque on the posterior surface of the patient's left thigh showed minimal epidermal spongiosis with focal parakeratosis. A discrete, cuff-like, predominantly lymphohistiocytic, perivascular inflammatory infiltrate not affecting the vascular walls was observed in the superficial dermis (Fig. 2). Periodic acid-Schiff staining revealed no fungal elements, and direct immunofluorescence was negative.
Laboratory tests, which included complete blood count, biochemistry, immune tests, and serology for Borrelia burgdorferi and hepatitis B and C viruses, were normal or negative. Based on the clinical and histopathologic findings, the patient was diagnosed with superficial AR-EAC. The lesions regressed after 2 months with no treatment.
AR-EAC is an uncommon form of EAC. Just 10 cases, including ours, have been described in 6 articles (Table 1).3,5–8 They involved 7 women and 3 men with a median age of 55 years (range, 36–83 years). The lesions were located on the extremities, and in some cases, the trunk or buttocks. The face, feet, and hands were spared in all cases. The lesions recurred annually, and in 1 case, this had happened for 23 years. They appeared in spring or summer, lasted for between 15 days and 5 months, and spontaneously regressed in summer or autumn. As mentioned, the clinical and histopathologic manifestations of AR-EAC are identical to those of classic EAC, and in particular the superficial classic form.
Cases of Annually Recurring Erythema Annulare Centrifugum in the Literature.
| Case no. | Author/y | Sex/age, y | No. of episodes, y | Season | Areas affected | Spontaneous resolution |
|---|---|---|---|---|---|---|
| 1 | Piñol Aguadé et al./19665 | F/60 | 7 | Spring-summer | Upper and lower limbs | In 15 d |
| 2 | Piñol Aguadé et al./19665 | F/43 | 17 | Summer | Upper and lower limbs | In 20 d |
| 3 | Janss et al./19926 | F/36 | 2 | Not reported | Trunk and upper limbs | In 6 wk |
| 4 | García Muret et al./20063 | F/76 | 8 | Summer | Trunk, upper and lower limbs | In autumn |
| 5 | García Muret et al./20063 | M/83 | 23 | Summer | Upper and lower limbs | In autumn |
| 6 | García Muret et al./20063 | M/55 | 13 | Summer | Upper and lower limbs | In 15 d |
| 7 | García Muret et al./20063 | F/55 | 15 | Spring | Upper and lower limbs | In 4–5 mo |
| 8 | Ruiz Villaverde et al./20107 | F/38 | 4 | Spring | Upper limbs | In 2 mo |
| 9 | Mandel et al./20158 | F/46 | 12 | Summer | Upper and lower limbs | In 4 mo |
| 10 | Present case | M/66 | 5 | Summer | Buttocks and lower limbs | In 4 mo |
Abbreviations: F, female; M, male.
The cause of AR-EAC is unknown, and no triggers have been identified. The constant, periodic course of this condition could be linked to temperature or reactions to certain seasonal plants or fungi. It is not associated with sun exposure, as it typically affects covered areas, with sparing of the face.3 There are no effective treatments.1
What is particularly noteworthy about AR-EAC, apart from the importance of recognizing it, is its broad differential diagnosis, which includes recurring skin conditions that present with annular lesions or lesions that mainly appear in summer months. It is first necessary to rule out recurring forms of nonidiopathic EAC with a clear trigger, such as tonsillitis or stress.9 Erythema papulosa semicircularis recidivans (EPSR) is a recently described entity characterized by semicircular erythematous plaques that can also recur annually and seasonally. Unlike AR-EAC, EPSR tends to have larger and fewer lesions, with nonscaling papular borders, that appear on the trunk.4,10 As reported by Bernia et al.,4 even though EPSR and AR-EAC have distinct clinical and histopathologic features, some authors prefer to include both within the spectrum of recurring figurate erythemas. Recurring erythematous scaling lesions with similar features have also been described in association with hereditary lactate dehydrogenase M-subunit deficiency. Other conditions that should be ruled out include fixed drug eruption, urticaria, autoimmune progesterone dermatitis, erythema marginatum rheumaticum, erythema chronicum migrans, dermatophytosis, granuloma annulare, pityriasis rosea, parapsoriasis, annular psoriasis, subacute cutaneous lupus erythematosus, and polymorphic light eruption reactions.3,6,7