In recent years, there has been a trend towards conservative management of breast cancer, which involves the use of adjuvant radiotherapy. This approach carries a risk of radiation-induced secondary malignancy.
We present the case of a 70-year-old woman who underwent quadrantectomy combined with adjuvant radiotherapy to treat invasive ductal carcinoma in her right breast in 2007. She was referred to our center 3 years later with a 1-month history of skin lesions. Examination revealed several red-violaceous nodules and papules, with multifocal involvement of the treated breast (Fig. 1).
Histopathology of 1 of the nodules revealed a poorly defined dermal tumor infiltrating the subcutaneous layer, which was formed by a proliferation of vascular structures alternating with undifferentiated solid areas (Fig. 2). The vascular structures were covered by endothelial cells with atypia, whereas the solid areas contained highly proliferative pleomorphic epithelioid cells (6 mitoses per 10 high-power fields) and interstitial hemorrhaging. The tumor cells proved to be immunoreactive to vascular markers (CD31 and CD34) and negative to epithelial markers (epithelial membrane antigen and pancytokeratin). Immunostaining for herpes simplex virus type 8 was negative.
A, Cell proliferation affecting the entire dermis, in which interstitial hemorrhage and vascular lumens are visible (hematoxylin-eosin [H&E], original magnification ×40). B, Vascular channels lined by endothelial cells with atypia infiltrating the collagen bundles (H&E, original magnification ×200). C, Pleomorphic epithelioid cells, between which several atypical mitoses are visible (H&E, original magnification ×400). D, Immunohistochemical staining with anti-CD31 antibody was positive for proliferating cells (H&E, original magnification ×200).
These findings confirmed the diagnosis of angiosarcoma, and the patient underwent simple mastectomy. Pathological examination of the surgical specimen showed the presence of several dermal nodules (the largest measuring 4×3cm) and foci in the breast parenchyma (2-5mm). Histopathology confirmed the diagnosis of high-grade angiosarcoma, with disease-free margins. The results of the staging study (computed tomography of the thorax, abdomen, and pelvis and positron emission tomography) were negative. After a 9-month follow-up period, the patient remains disease-free.
Angiosarcoma is a very uncommon endothelial cell tumor.1 It accounts for less than 1% of cases of sarcoma and most frequently affects the skin.2,3 Cutaneous angiosarcoma can be divided into 3 main types: the classic or idiopathic type, the chronic lymphedema–associated type, and the radiation-induced type. Classic idiopathic angiosarcoma affects the skin of the head and neck in elderly patients3,4 and is the most frequent variety (50%-60%).5 Chronic lymphedema–associated angiosarcoma appears after a period ranging from 4 to 27 years4 and almost always (>90% of cases) develops in a limb with chronic lymphedema following radical mastectomy with axillary lymph node dissection (Stewart-Treves syndrome). Radiation-induced angiosarcoma appears in an irradiated field after a latency period.2 In previous decades, this variety mostly affected the abdomen after radiotherapy for abdominopelvic tumors.2,3 Today, however, angiosarcoma is detected mainly on the skin of the breast in women aged more than 60 years who have undergone adjuvant radiotherapy after conservative surgery for breast cancer. The latency period is 3 to 5 years in most cases.2 In any case, angiosarcoma remains a very uncommon complication (0.05%-0.16% of patients2,3,6).
Clinically, angiosarcoma is characterized by the onset of erythematous-violaceous nodules or plaques that are typically multifocal. Histopathology findings correspond to those reported in our case. Growth is explosive in high-grade tumors and more insidious in low-grade tumors.1,2 Its appearance may be similar to that of cutaneous metastases and of erysipelatoid carcinoma (cutaneous metastasis whose symptoms are similar to those of erysipelas). The differential diagnosis should include atypical vascular lesions (AVLs), which are cutaneous vascular proliferations that appear after radiotherapy for breast cancer with a latency period of 3 to 6 years.7 Unlike angiosarcoma, AVLs are not characterized by multiple layers of endothelial cells, prominent nucleoli, mitosis, atypia, destruction of skin appendages, areas of solid growth, invasion of the subcutis, or hemorrhage. Furthermore, AVLs are circumscribed lesions with frequent chronic inflammation and stromal projections in the lumen, which are not found in angiosarcoma.1,7 Radiation-induced angiosarcoma was recently shown to involve an amplification of the v-myc myelocytomatosis viral oncogene homolog (avian) gene (MYC), which is not found in AVLs. The presence of this gene could be used to confirm a diagnosis in complex cases or when the available tissue is limited.8 It is therefore important to remember that sufficient sample material must be obtained, since punch biopsy findings can lead to an erroneous diagnosis.1
Treatment involves aggressive surgical excision.3 Hyperfractionated accelerated adjuvant radiotherapy has been reported to achieve better control of the disease.9 Prognosis is poor, with high recurrence rates and a strong tendency to metastasize.2 Overall survival at 5 years is 12% to 20%, and mean survival is 18 to 28 months.5 Some data suggest that radiation-induced angiosarcoma could have a poorer prognosis than sporadic angiosarcoma.10
In conclusion, we present a case of multifocal angiosarcoma of the skin of the breast. This condition is a very uncommon yet very aggressive complication of radiotherapy that should be suspected in patients with erythematous-violaceous nodules on a previously irradiated breast. Given the recent trend towards conservative management of breast cancer, we should be on the alert for possible increases in the incidence of this tumor.
Please cite this article as: M. Armengot-Carbó, M.J. Roca-Estellés, E. Quecedo-Estébanez, E. Gimeno-Carpio. Angiosarcoma cutáneo tras radioterapia por cáncer de mama. Actas Dermosifiliogr. 2012;103:557-9.


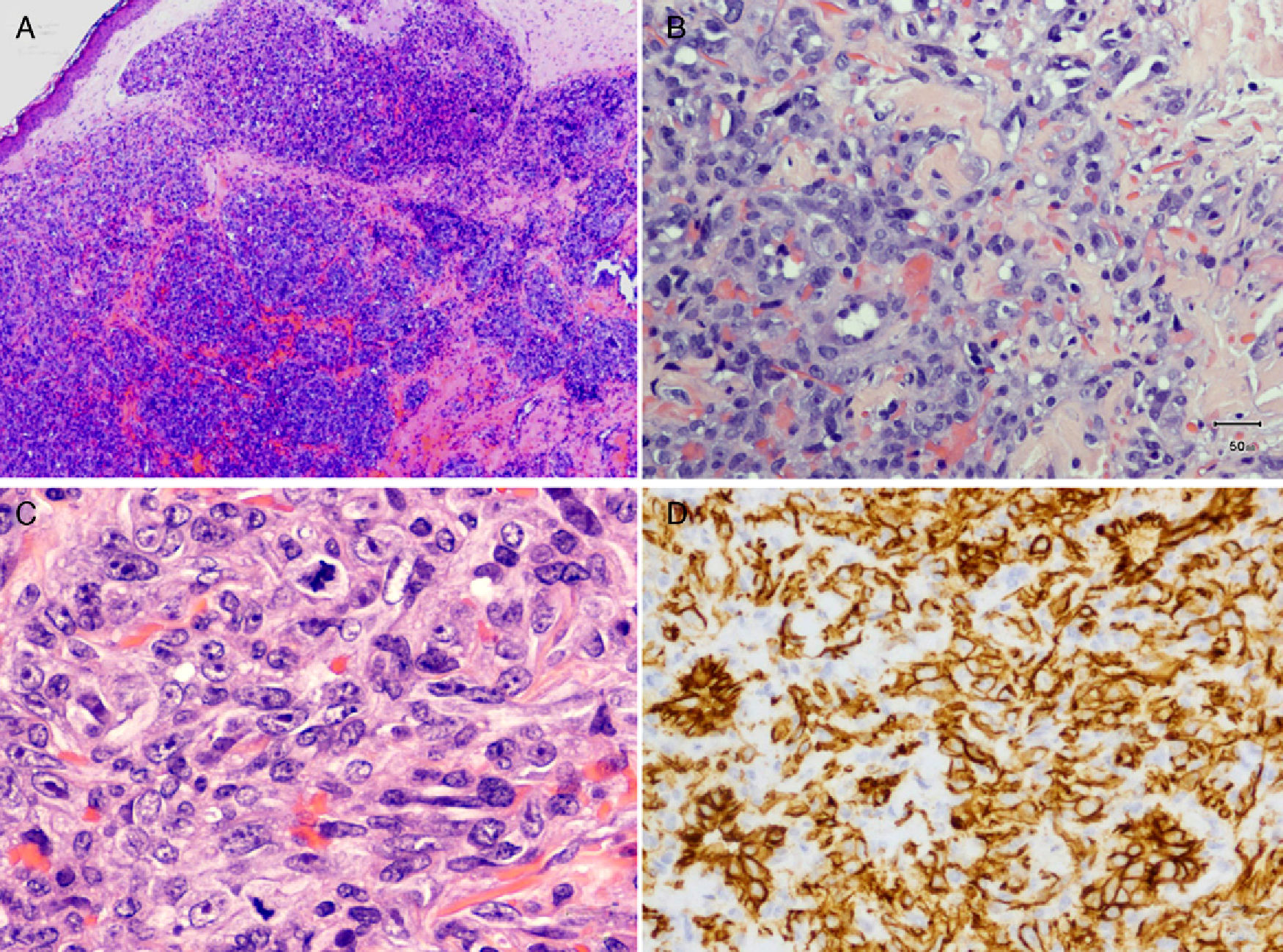

![A, Cell proliferation affecting the entire dermis, in which interstitial hemorrhage and vascular lumens are visible (hematoxylin-eosin [H&E], original magnification ×40). B, Vascular channels lined by endothelial cells with atypia infiltrating the collagen bundles (H&E, original magnification ×200). C, Pleomorphic epithelioid cells, between which several atypical mitoses are visible (H&E, original magnification ×400). D, Immunohistochemical staining with anti-CD31 antibody was positive for proliferating cells (H&E, original magnification ×200). A, Cell proliferation affecting the entire dermis, in which interstitial hemorrhage and vascular lumens are visible (hematoxylin-eosin [H&E], original magnification ×40). B, Vascular channels lined by endothelial cells with atypia infiltrating the collagen bundles (H&E, original magnification ×200). C, Pleomorphic epithelioid cells, between which several atypical mitoses are visible (H&E, original magnification ×400). D, Immunohistochemical staining with anti-CD31 antibody was positive for proliferating cells (H&E, original magnification ×200).](https://static.elsevier.es/multimedia/15782190/0000010300000006/v1_201304241313/S1578219012002107/v1_201304241313/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



