To evaluate the results of an outpatient program for major dermatological surgery in patients with a range of skin conditions.
MethodsWe undertook a retrospective, observational study of patients who underwent scheduled dermatological surgery as outpatients in a public hospital between 2004 and 2007. The most common procedures were excision of basal cell or squamous cell carcinoma with or without graft reconstruction. The rates of substitution (of inpatient procedures), cancellation, hospital admission, and readmission were analyzed along with service utilization and systemic complications arising within the first 72h of surgery. Variables were analyzed as relative frequencies. The occurrence of complications during the study period was analyzed by chi square test.
ResultsA total of 2789 patients underwent surgery during the study period, and of those, 2757 procedures were performed on an outpatient basis (overall substitution rate, 17.99%). The service utilization was 74.36%. Fourteen patients were admitted to hospital following surgery (2.62%), and of those 12 were admitted immediately (85.71%). Nine patients had serious complications (cardiovascular, neurological, metabolic, or infectious), representing a proportional risk of 1:59. Less serious complications (hypertension, nausea, vomiting, and vasovagal syncope) requiring hospital admission occurred in 25 patients.
ConclusionsMajor surgery undertaken on an outpatient basis is an excellent multidisciplinary surgical care model that allows well-selected patients to be treated effectively, safely, and efficiently. A small percentage of postoperative complications of varying severity can still occur despite patients’ meeting optimal criteria for success. Fortunately, however, the rate of mortality is practically zero.
Evaluar los resultados de un programa de cirugía mayor ambulatoria en pacientes intervenidos quirúrgicamente de diversas patologías dermatológicas en nuestro hospital.
MétodosEstudio observacional retrospectivo que incluye los pacientes intervenidos de forma programada en el periodo 2004-2007 en un hospital público realizándose diferentes procedimientos quirúrgicos de forma ambulatoria, siendo la cirugía de exéresis de carcinomas basocelulares y espinocelulares, con y sin injerto, la operación mayoritaria. Se han analizado diversos índices (sustitución, suspensión, ingresos, reingresos), así como el rendimiento quirúrgico y las complicaciones sistémicas que surgieron dentro de las primeras 72 horas tras la cirugía. La medición de las variables se realizó mediante frecuencias relativas. El análisis utilizado para la evolución de las complicaciones en el periodo de estudio fue la Chi cuadrado de tendencias.
Resultados2.789 pacientes fueron intervenidos en el periodo indicado, de los que 2.757 se operaron de forma ambulatoria (índice de sustitución global del 17,99%). El rendimiento quirúrgico medio fue 74,36%. El índice de ingresos tras la cirugía fue 2,62% (14 pacientes), siendo ingresos inmediatos en el 85,71% de los casos (12). Nueve pacientes sufrieron complicaciones graves (cardiovasculares, neurológicas, metabólicas e infecciosas), representando un riesgo proporcional de 1:59. En 25 pacientes aparecieron complicaciones de menor gravedad (hipertensión arterial, náuseas, vómitos, síncope vasovagal) que requirieron ingreso hospitalario.
ConclusionesLa cirugía mayor ambulatoria (CMA) es un excelente modelo organizativo de asistencia quirúrgica multidisciplinar, que permite tratar pacientes bien seleccionados de una manera efectiva, segura y eficiente. A pesar del cumplimiento de los requisitos óptimos, existe un porcentaje pequeño de complicaciones postoperatorias de gravedad variable, aunque afortunadamente la mortalidad es prácticamente nula.
Minor dermatology surgical interventions are typically performed in ambulatory settings. A range of anesthetic techniques are used in dermatology, including different types of general or locoregional anesthesia, monitored anesthesia care, and local anesthesia. Important benefits are reported for both the patient and the dermatologist when procedures are performed using a range of different approaches to anesthesia in the outpatient setting.1
The term major ambulatory surgery refers to surgical treatment in an outpatient setting under conditions that have traditionally required admission to hospital. The term excludes disorders that have always been treated in an ambulatory setting (mainly the excision of skin lesions), collectively referred to as minor ambulatory surgery. Major ambulatory surgery is the optimal model for multidisciplinary surgical care, as selected patients can be treated effectively, safely, and efficiently, and no hospital bed is required. The resulting reduction in bed occupancy rates reduces surgery waiting times for conditions for which admission is necessary. In an increasing number of medical-surgical specialties, including dermatology, there is a growing interest in reducing the length of hospital stays.2 Patient safety does not depend so much on whether the intervention takes place in an inpatient or outpatient setting as on adherence to rigorous patient selection principles.
Even when procedures are optimally complied with, however, complications may arise after discharge, whether as a result of the surgical procedure, or because the anesthesia used in surgery exacerbates a preexisting condition. According to the literature, the most frequent complications are surgical wound infection and bleeding.3 Even so, mortality is practically zero, and the complication rate is extremely low.
This article presents the results and postoperative complications in a retrospective study of a cohort of dermatology department patients who underwent major ambulatory surgery or short-stay surgery.
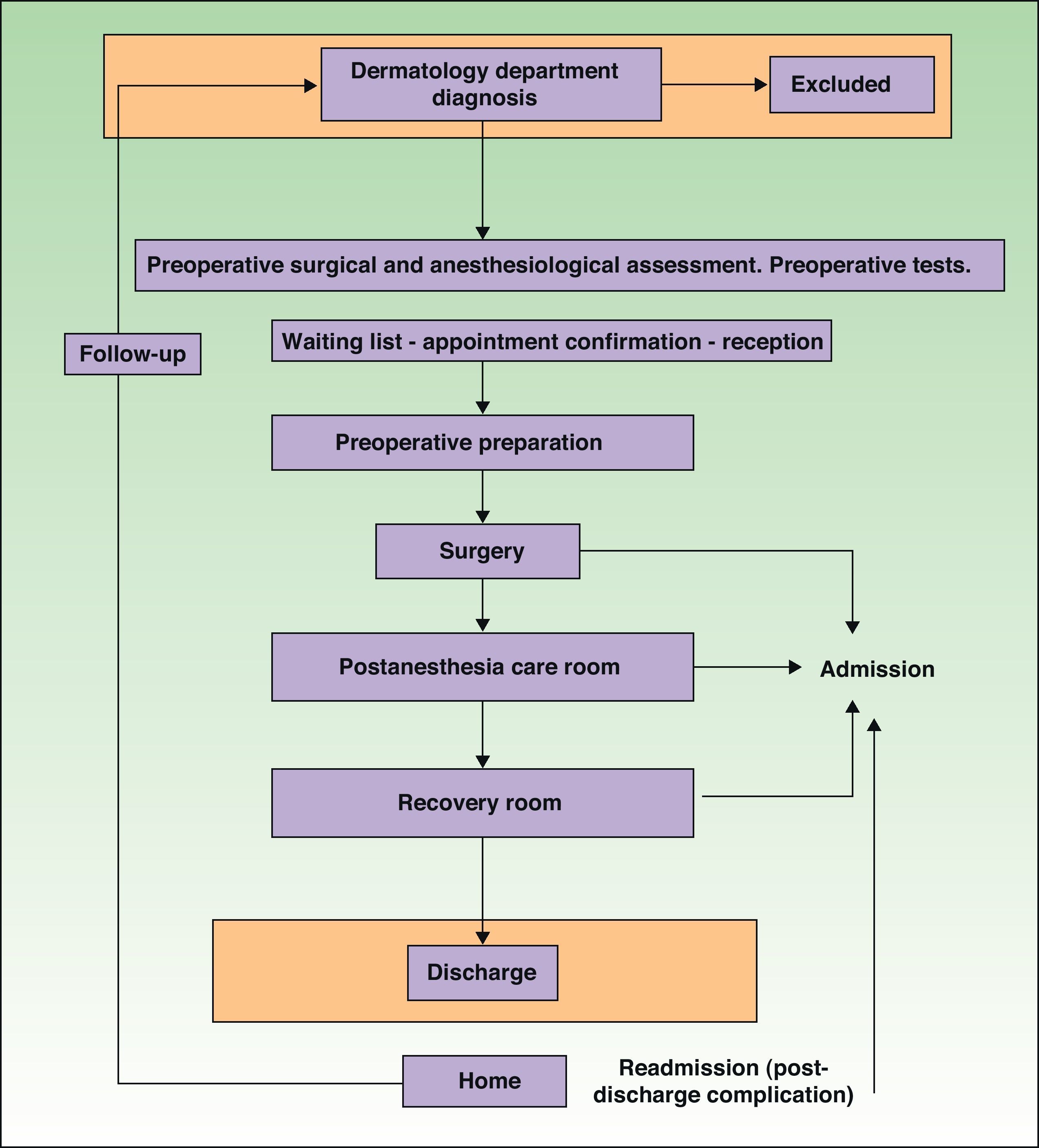
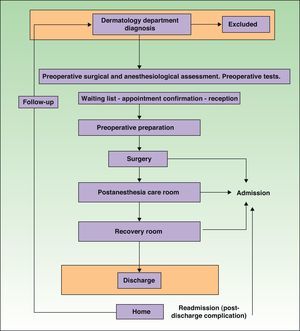
Material and MethodsThis retrospective observational study was conducted in a public hospital with an outpatient surgery unit that is physically and organizationally part of the hospital, but independently managed. The unit has an independent section specifically for the treatment of skin disorders (Fig. 1). The hospital's catchment area has 325000 inhabitants. In the 4-year study period from January 2004 to December 2007, major surgery was performed on a total of 33127 outpatients. In the dermatology department, patients who had been diagnosed were included in the surgery waiting list, and then scheduled for major ambulatory surgery, short-stay surgery, or minor ambulatory surgery, depending on the complexity of the intervention and the patient's baseline status. The following cases were classified as major ambulatory surgery: patients with large, multiple, or surgically complex skin lesions; patients with high associated comorbidity; and patients who required monitored anesthesia care, sedation, or general or neuraxial anesthesia. Patients programmed for major ambulatory surgery, just like candidates for traditional surgery, were assessed before surgery in accordance with anesthesiology department procedures regarding age and comorbidity. This assessment included laboratory tests (blood count, basic coagulation study, routine blood glucose and urea tests, and additional specific tests relating to comorbidities), electrocardiogram, and chest X-ray. Note that the study also included patients with mental disabilities, patients with high associated comorbidity (American Society of Anesthesiologists [ASA] physical status 3 and 4), and cases in which the dermatology department required the presence of an anesthesiologist in the operating room.
The anesthetic techniques used were chosen in each case by the anesthesiologist, who took into account, whenever possible, the fact that the patient would be discharged home rather than to a hospital ward. After the intervention, patients were first transferred to a postanesthesia care room and subsequently to a recovery room. Once they met the general discharge criteria specified in the unit's postoperative analgesia protocol, they were allowed to go home.
Data were collected on substitution, theater utilization, reasons for patient admission and readmission after discharge (within 72h of surgery), as well as the reasons for surgery delays and cancellations. The data were compiled from computerized emergency department records and from the minimum basic data set of hospital discharge records for the years of the study. Surgical procedure records are entered into PLAN HP-HIS and HP-DOCTOR (clinical and financial management systems), and these data are automatically integrated into the module for managing surgery waiting lists in the patient information system.
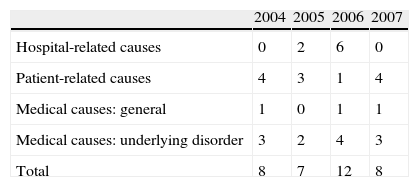
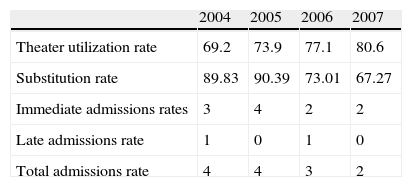
The substitution rate is the number of major ambulatory surgery interventions expressed as a percentage of all surgical interventions in the dermatology department. The theater utilization rate reflects percentage occupation or use of operating rooms. The admissions rate refers to unplanned admissions, whether immediate (from the postanesthesia care room) or late (from the recovery room). The readmissions rate refers to admission for a complication that occurred after the patient returned home. The cancellation rate refers to the interventions that failed to take place on the scheduled date. Cancellations were classified into 3 broad groups: hospital-related cancellations (changes to referrals, scheduling errors, lack of equipment, inappropriate preparation, and time constraints); patient-related cancellations (refusal to undergo surgery or to be admitted), and cancellations for medical reasons (underlying disorder, surgery not indicated, nonavailability of surgeon or anesthesiologist, or contraindication on the part of the anesthesiology department).
On discharge from the unit, all patients received a discharge report and specific postoperative recommendations. Within 24h of surgery, the patients were followed up by telephone, and 48–96h after surgery they attended the dermatology outpatient department for follow-up according to the usual protocol.
Variables were expressed in terms of relative frequency. A descriptive analysis of the variables was performed in order to study complications in terms of possible associations. For quantitative variables we used the Student t test or the Kruskal–Wallis test when variances were unequal, and for qualitative variables we used the χ2 test with Yates correction or Fisher's exact test.
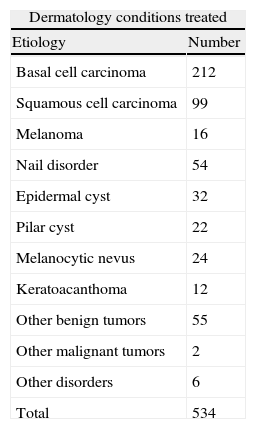
ResultsA total of 2789 scheduled surgeries (32 inpatient and 2757 outpatient) were performed by the dermatology department during the study period (2004–2007). The final study cohort comprised the 534 patients from this group who underwent dermatological procedures that required anesthesia. The most frequent intervention was the excision of squamous or basal cell carcinomas, with and without graft reconstruction. Other diseases treated were melanomas, carcinoma of the lip, scars of various kinds, fibromas, dermatofibromas, common melanocytic nevi, cheilitis, leukoplakia on the lip, actinic keratoses, seborrheic keratoses, pilar cysts, epidermal cysts, and warts. Table 1 summarizes the etiology of the dermatology lesions treated surgically. The overall substitution rate was 17.99%.
Etiology of Dermatology Conditions Treated in Major Ambulatory and Short-Stay Surgery Regimes.
| Dermatology conditions treated | |
| Etiology | Number |
| Basal cell carcinoma | 212 |
| Squamous cell carcinoma | 99 |
| Melanoma | 16 |
| Nail disorder | 54 |
| Epidermal cyst | 32 |
| Pilar cyst | 22 |
| Melanocytic nevus | 24 |
| Keratoacanthoma | 12 |
| Other benign tumors | 55 |
| Other malignant tumors | 2 |
| Other disorders | 6 |
| Total | 534 |
Of the 2789 interventions, 1265 were in men (45.36%) and 1524 in women (54.64%). The mean age of patients was 73.65±4.89 years. Only 42 patients (7.86%) had ASA physical status 1 and 2; 276 patients (51.31%) had ASA status 3 (severe systemic disease), and the remaining 216 patients had ASA status 4 (severe systemic disease that is a constant threat to life). General anesthesia was used for 56 patients (10.48%), and neuraxial anesthesia was used for 32 patients (5.99%). In the remaining cases different moderate sedation and analgesia protocols were used. No statistically significant association was found between complications and the type of anesthesia used (P=.23).
The most frequent surgical intervention was skin graft or debridement (60.75%). Interventions occurred at a rate of 6.02 patients a day. Mean surgery time was 39.56±18.45min.
The scheduled intervention was cancelled for 36 of the 534 cases in which anesthesia required monitoring by the anesthesiology department (an overall cancellation rate of 6.74%). The most frequent reasons for cancellation were medical (15 patients), mainly related to an underlying disease. Table 2 shows the reasons for cancellation and annual variations in the number of interventions cancelled.
The mean theater utilization rate for the study period was 74.36%, reaching a maximum of 80.6% in the final year of the study. Yearly variations are shown in Table 3; the gradual improvement can be attributed to accumulated experience and the inclusion in the protocol of a telephone interview in the days before surgery. The admissions rate was 2.62% (14 patients), mostly immediate admissions (12 patients). Yearly variations are shown in Table 3.
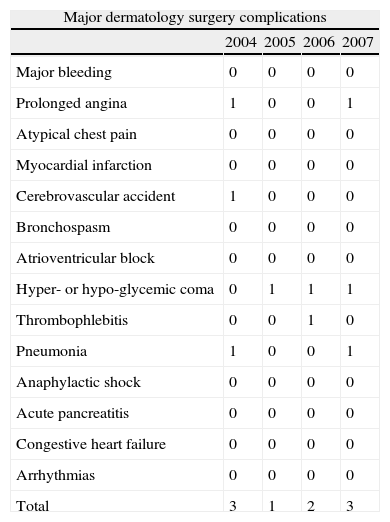
Major complications, such as cardiovascular and cerebrovascular events, severe infections, and exacerbation of preexisting disorders, occurred in 9 patients; the proportional risk of suffering a major complication in our series was 1:59. The most frequent major complication was diabetic coma, which accounted for a third of all complications. Of the 9 patients with major complications from the cohort of 534 patients, 2 had respiratory failure (mainly due to pneumonia), 2 had prolonged angina, 1 had a central nervous system deficit, and 1 had deep vein thrombosis. Minor complications (hypertension, vomiting, nausea, and surgical wound pain) led to the hospitalization of 25 patients; the most common causes were vasovagal syncope and surgical wound infection (Table 4). No statistically significant associations were found between the occurrence of minor and major complications and the ASA classification (P=.73 and P=.70, respectively), dermatological diagnosis (P=.54 and P=.46, respectively), or age (P=.43 and P=.67, respectively). A statistically significant association was found, however, between surgery duration and major complications (P=.04), although not minor complications (P=.28).
Major Dermatology Surgery Complications.
| Major dermatology surgery complications | ||||
| 2004 | 2005 | 2006 | 2007 | |
| Major bleeding | 0 | 0 | 0 | 0 |
| Prolonged angina | 1 | 0 | 0 | 1 |
| Atypical chest pain | 0 | 0 | 0 | 0 |
| Myocardial infarction | 0 | 0 | 0 | 0 |
| Cerebrovascular accident | 1 | 0 | 0 | 0 |
| Bronchospasm | 0 | 0 | 0 | 0 |
| Atrioventricular block | 0 | 0 | 0 | 0 |
| Hyper- or hypo-glycemic coma | 0 | 1 | 1 | 1 |
| Thrombophlebitis | 0 | 0 | 1 | 0 |
| Pneumonia | 1 | 0 | 0 | 1 |
| Anaphylactic shock | 0 | 0 | 0 | 0 |
| Acute pancreatitis | 0 | 0 | 0 | 0 |
| Congestive heart failure | 0 | 0 | 0 | 0 |
| Arrhythmias | 0 | 0 | 0 | 0 |
| Total | 3 | 1 | 2 | 3 |
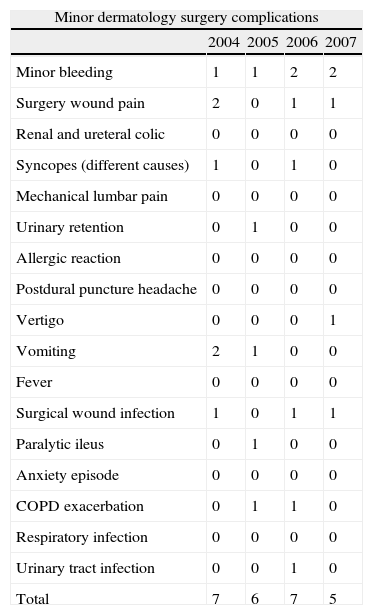
In total, 34 patients (6.34%) were admitted from home with major (9 patients) or minor (25 patients) complications; none of the patients died. Tables 4 and 5 summarize the major and minor complications, respectively, that led to hospitalization during the study period.
Minor Dermatology Surgery Complications.
| Minor dermatology surgery complications | ||||
| 2004 | 2005 | 2006 | 2007 | |
| Minor bleeding | 1 | 1 | 2 | 2 |
| Surgery wound pain | 2 | 0 | 1 | 1 |
| Renal and ureteral colic | 0 | 0 | 0 | 0 |
| Syncopes (different causes) | 1 | 0 | 1 | 0 |
| Mechanical lumbar pain | 0 | 0 | 0 | 0 |
| Urinary retention | 0 | 1 | 0 | 0 |
| Allergic reaction | 0 | 0 | 0 | 0 |
| Postdural puncture headache | 0 | 0 | 0 | 0 |
| Vertigo | 0 | 0 | 0 | 1 |
| Vomiting | 2 | 1 | 0 | 0 |
| Fever | 0 | 0 | 0 | 0 |
| Surgical wound infection | 1 | 0 | 1 | 1 |
| Paralytic ileus | 0 | 1 | 0 | 0 |
| Anxiety episode | 0 | 0 | 0 | 0 |
| COPD exacerbation | 0 | 1 | 1 | 0 |
| Respiratory infection | 0 | 0 | 0 | 0 |
| Urinary tract infection | 0 | 0 | 1 | 0 |
| Total | 7 | 6 | 7 | 5 |
Abbreviation: COPD, chronic obstructive pulmonary disease.
The main contribution of this study is its confirmation that major ambulatory surgery is an excellent organizational model for multidisciplinary surgical care and one that enables carefully selected dermatology patients to be treated effectively, safely, and efficiently.
The fundamental difference between inpatient and outpatient surgery is that, in the latter, patients spend the postoperative period at home, so even small incidents tend to be viewed by patients and their families as complications. In major outpatient surgery, the anesthesiologist plays a key role during all stages of perioperative care. Although dermatology and cosmetic surgery techniques are now extremely safe, trivial complications are relatively common and frequently lead to delays in discharge, unplanned admissions, and readmissions. Despite the increasing complexity of surgical techniques and cancer surgery in recent years, short-stay and major ambulatory surgery can be considered to be well established in dermatology. Outpatient surgery offers significant cost savings and reduces bed occupancy without compromising patient safety or quality of care.4
Most of the dermatology surgery cases in our series did not require hospitalization. In the 4 years of the study, 80.85% (2255) of the 2789 patients had minor surgery as outpatients with local anesthesia. Other anesthetic techniques or monitored anesthesia care were required in 534 of the 2789 patients because the surgical intervention was complex, comorbidity was high, or the patient was noncooperative. These patients remained in postoperative care until full recovery, after which they returned home. A short hospital stay was required for 32 of the 2789 patients (1.14%). As can be seen in the literature, dermatological surgery can sometimes be complex.5
The results for our series corroborate those of other surgical series3 in that resections of basal and squamous cell carcinomas were the procedures that most often required some degree of anesthesia.
The contraindication for anesthesia is often provisional, and is usually related to the need to stabilize a progressive disease. Preoperative visits are aimed at stabilizing underlying disorders and minimizing perioperative risk.3 Noteworthy in our study is the fact that, once we exclude those with mental disabilities, most of the patients (91.94%) had high associated morbidity (ASA physical status 3 or 4). The last decade has witnessed a sharp decline in the use of general anesthesia (now largely used only for children and noncooperative patients) in favor of conscious sedation and monitored anesthesia care.6 Analysis of our series revealed no association between medical complications and the anesthesia procedure, patient age, or patient baseline status according to the ASA classification. A significant proportion of our dermatology surgery cohorts were elderly patients (mean age, 73.65±4.89), for whom intervention was essential for their autonomy and psychological wellbeing. Outpatient regimes have the advantage that they cause minimal disruption to patients’ routines and frees patients from the inconvenience of spending a night away from home.
The rate of admissions after outpatient surgery in dermatology units is usually between 1% and 2%,7,8 although the literature reflects great variations worldwide, with figures ranging between 0.28% and 9.50%.17 The unplanned admissions rate for our study (2.62%) was within acceptable limits, although higher than that reported for other series.9 One explanation may be that we included complex surgical procedures in our series, and did not apply exclusion criteria related to the duration of the procedure or the patients’ baseline physical status. Normally, outpatient surgery is performed in healthy patients with no significant pathology and without supervision by an anesthesiologist. Our data refer to a cohort of 534 patients in poor physical health. No data were collected on the social reasons for admission. The inclusion of patients with poor physical health and a greater number of comorbid conditions naturally gave rise to a higher admissions rate.
Since several studies report extremely low readmission rates from home—below 1%,10,11 and even as low as 0.15%10—our readmission rate of 6.34% is at odds with the published data. Complications due to the patient's medical history are common. New anesthetic techniques minimize the cardiovascular and respiratory effects of general anesthesia, and also reduce postoperative morbidity. These results suggest that major ambulatory surgery is an effective approach to treating many dermatological disorders. Major complications are adverse reactions with a potential to cause serious harm, whereas minor complications are those with only minimal potential to cause serious harm. The evidence indicates that major complications are rare,12 and that mortality is extremely rare. 13 Mortality following major ambulatory surgery ranges between 1/66500 and 1/11273; Natof,13 for example, published results for a series of 1.1 million outpatients who had undergone general anesthesia, reporting a mortality rate of 0.15/10000. All these rates are considerably lower than those reported for traditional inpatient surgery. Mortality mainly affects elderly patients, and cardiovascular complications are the main cause of death. There were no deaths in our major ambulatory surgery cohort.
Myocardial infarction, pulmonary embolism, and cerebral deficit are all extremely rare and the reported incidence is as low as that which could be expected in a cohort of patients of the same age who have not undergone surgery.14 In our series of 534 patients, there were only 9 major complications, despite the fact that the study cohort was composed mostly of patients with very poor health who required complex surgery. Adverse events usually occur within 2 days of surgery, although it has been reported that approximately 40% of complications occur between 2 days and 30 days after surgery.15
The key issue is not mortality, which is lower than would be expected given the demographic data; the main challenge is the morbidity associated with the surgery and the anesthesia.16 With an incidence estimated to be around 3%, perioperative complications are more often related to surgery than to the patient's medical condition.17 The most commonly reported complications are graft failure, wound infection, and bleeding.2,3,11 In our series of 534 patients, most complications were minor, mainly bleeding (6 cases, 1.12% of the cohort), followed by pain and surgical wound infection. These results indicate the importance of strict compliance with analgesic protocols for all kinds of interventions and for all types of anesthesia. Severe pain can trigger vomiting, and pain relief can also exacerbate vomiting.14,18
In our series, as in other studies in the literature,7,19,20 the most frequent reasons for admission to hospital were altered glucose metabolism. Vomiting and nausea have traditionally been considered a major reason for admission,14 but their incidence has declined in recent years due to the availability of new antiemetic drugs. About 90% of major ambulatory surgery patients experience some complication after discharge,21 and approximately one-third of all postoperative complications occur within 2 days of surgery. Liaison between specialist care and primary care is therefore crucial in the postoperative follow-up of these patients.22
The main limitation of this study, apart from the fact that it was retrospective, is that the disproportionate weight of patients with high comorbidity requiring complex surgery is likely to have affected the results. Furthermore, the database from which the data were compiled is managed by the anesthesiology department and is lacking in surgical data. This problem should be remedied in the immediate future by greater collaboration on the part of surgery departments. Coding systems are also needed that would enable surgeons to evaluate the complexity associated with individual patients and procedures. Major ambulatory surgery units need to keep records and periodically measure and compare a range of quality indicators.23 Such records and indicators could lay the groundwork for national standards and guidelines that would help to improve outcomes.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as. Cortiñas Saenz M, et al. Análisis de resultados, índices de calidad y complicaciones extrahospitalarias de un programa de cirugía ambulatoria en Dermatología. Actas Dermosifiliogr. 2012;103:36–43.