Cutaneous leishmaniasis (CL) manifests as a papule or nodule that forms in response to the bite of mosquitoes that carries this parasitosis. These lesions tend to grow to form a well-defined plaque with a raised violaceous border that may ulcerate, leading to subsequent formation of a crust. Atypical presentations of CL are increasingly common, and pose a diagnostic challenge.
Diagnosis is based on histological and microbiological findings (ie, a positive result in polymerase chain reaction [PCR] analysis of blood or tissue). However, skin ultrasound can be a useful complementary technique for CL diagnosis and a tool to monitor treatment response in CL patients.
We describe 2 cases of CL with an unusual, erysipeloid presentation, and the corresponding ultrasound findings.
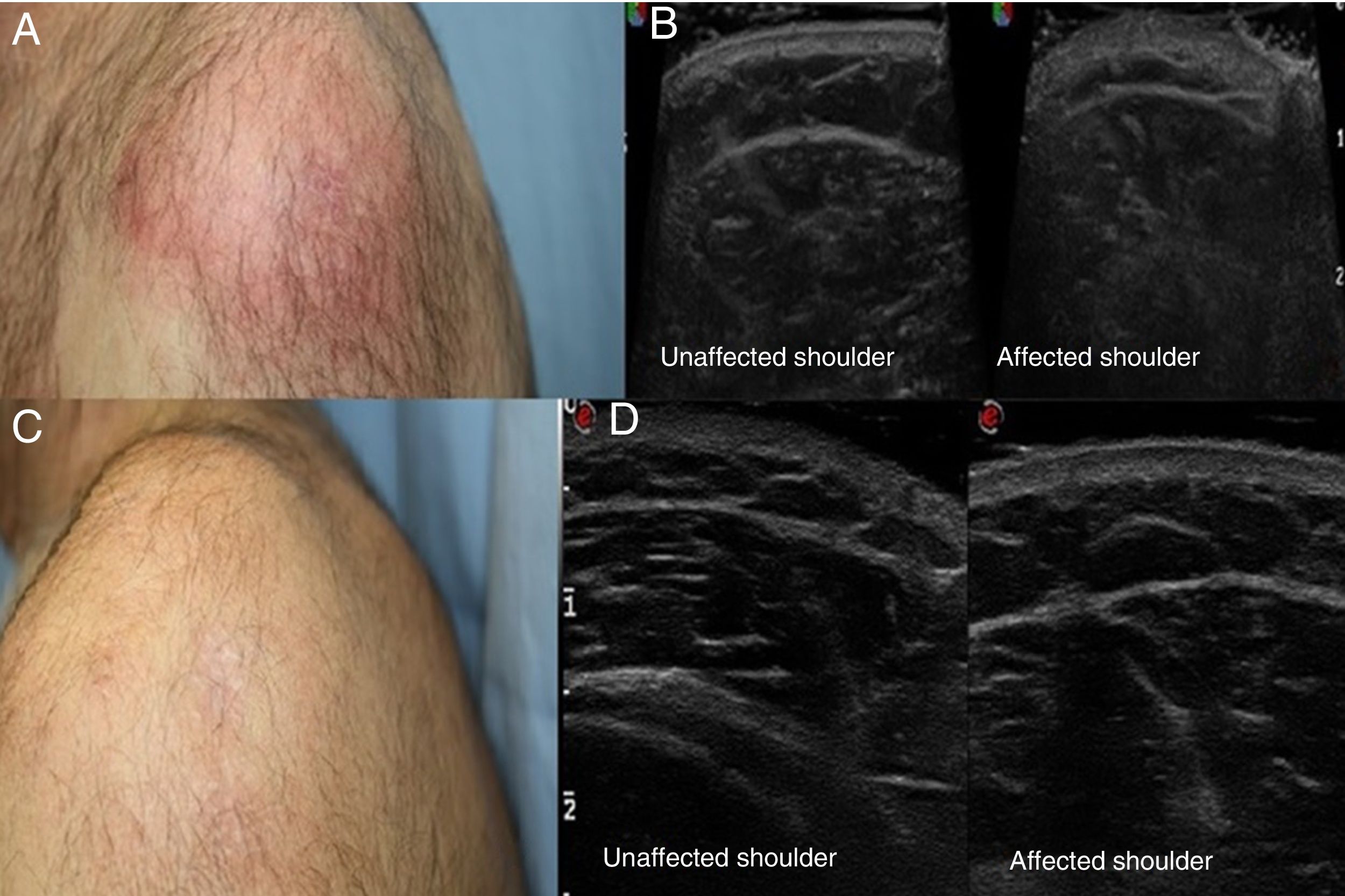
Case 1A 62-year-old man with a personal history of hepatic porphyria cutanea was seen for a lesion covering a large portion of the external aspect of the shoulder and upper left arm. The lesion had appeared 2 months earlier and was occasionally suppurative. The patient had been previously treated for suspected cellulitis with multiple oral antibiotics, without improvement. Physical examination revealed an indurated, erythematous plaque (9×7cm) with poorly defined borders that was hot to the touch (Fig. 1A). Histology revealed non-necrotizing granulomatous dermatitis and the presence of Leishmania bodies within the cytoplasm of the histiocytes. Skin ultrasound (SonoScape, 15-MHz linear probe) was performed to evaluate the extent of the lesion and showed diffuse thickening of the dermis in the affected area (Fig. 1B). Because of the lesion's large size, the patient was treated with intravenous amphotericin B (5mg/kg/d) for 3 days (total dose, 15mg/kg). The lesion resolved in response to treatment (Fig. 1C), as confirmed by subsequent ultrasound (Fig. 1D).
A, Poorly delimited erythematous plaque. B, Ultrasound images showing thickening of the dermis in the affected shoulder, as compared with the unaffected shoulder. C, Resolution of the lesion after treatment. D, Ultrasound images showing the affected and unaffected shoulders after treatment.
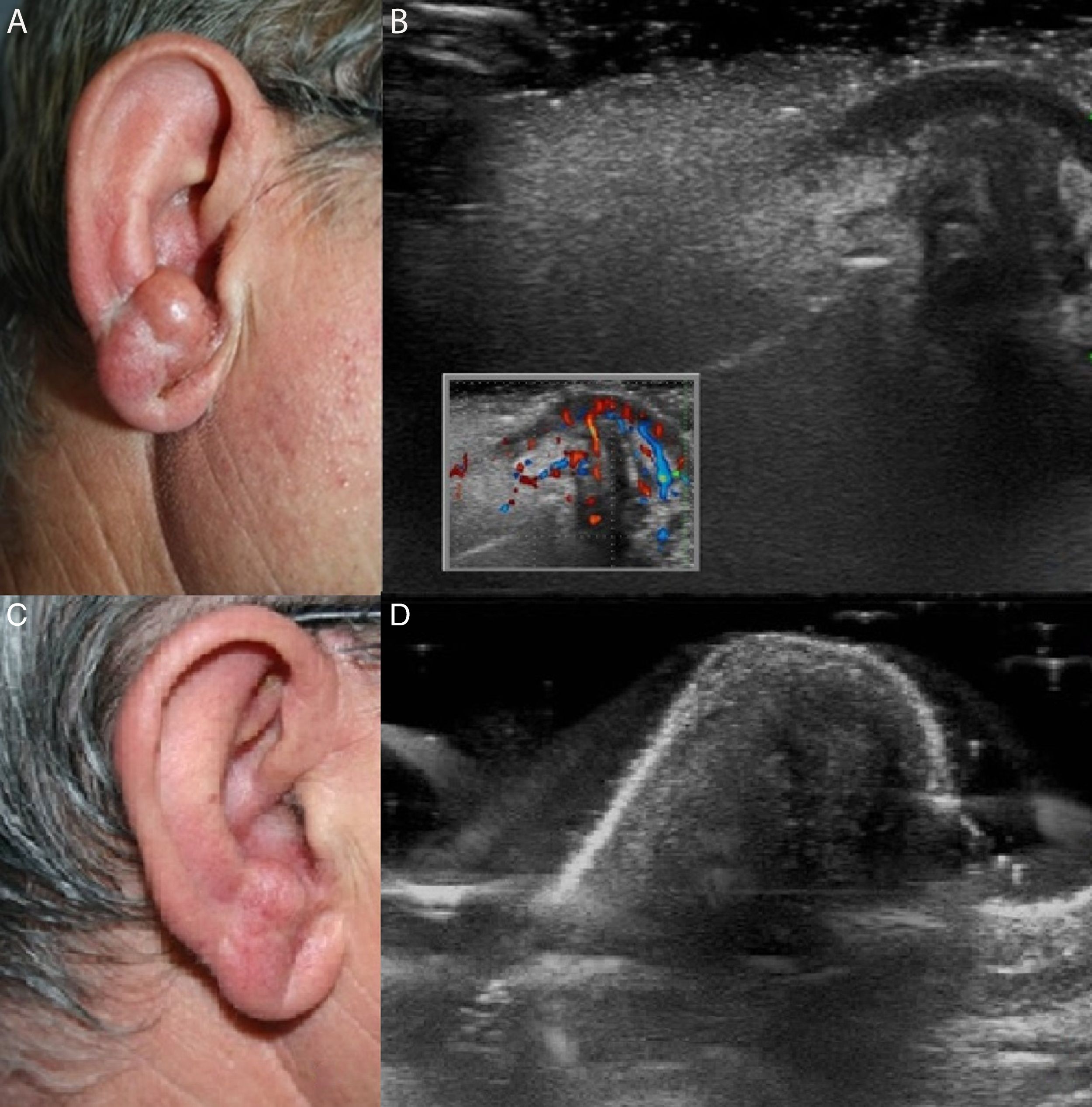
A 66-year-old man with a personal history of diabetes mellitus type 2 and dyslipidemia was referred from the otorhinolaryngology department with an asymptomatic lesion on the right pinna that had appeared 5 months earlier. He reported no previous trauma or insect bites in the affected location. The patient had been diagnosed with erysipela, for which he was treated with several oral and topical antibiotics, with no improvement. Physical examination revealed diffuse erythema on the right pinna. On the earlobe and antitragus the erythema was more pronounced and was accompanied by marked thickening (Fig. 2A). Histology revealed similar findings to those described for Case 1. The result of a PCR test for Leishmania DNA was positive. Ultrasound (SonoScape, 15-MHz linear probe) revealed an unencapsulated, hypoechoic structure in the superficial dermis that was well-delimited near the surface and less so at deeper levels, and exhibited increased low-resistance flow on Doppler imaging (Fig. 2B). The lesion resolved after treatment for 4 weeks with weekly infiltrations of intralesional meglumine antimoniate (injected subdermally until a wheal formed) (Fig. 2C and D).
A, Thickening and erythema of the antitragus and the pinna. B, Ultrasound image showing an unencapsulated, hypoechoic structure in the superficial dermis that was well-delimited near the surface and less so at deeper levels, and exhibited increased low-resistance flow on Doppler imaging. C, Resolution of the lesion after treatment. D, Ultrasound image showing the affected area after treatment.
Examination of both patients after 6 months revealed no signs of lesion recurrence or reactivation.
Leishmaniasis is a group of diseases caused by infection with any of over 20 protozoan species of the genus Leishmania, and is transmitted by the bite of insects of the genera Phlebotomus and Lutzomyia in the Old World and New World, respectively. The most common reservoirs are domestic mammals such as the dog, cat, rat, hare, and rabbit.1–3
CL has many different presentations, and recent years have seen an increase in atypical forms. The clinical presentation of leishmaniasis depends, among other factors, on the species involved and the immune response of the host.1,2,4
In a series published by Bari and Rahman,4 up to 5.7% of the 718 cases described were considered unusual forms of CL. These included lupoid, sporotrichoid, paronychial, erysipeloid, palpebral, psoriasiform, mycetoma-like, chancriform, scar, zosteriform, palmar/plantar, verrucous, and eczematous CL.1,4Lutzomyia mexicana causes a form of CL that is uncommon in the Old World but is transmitted by Lutzomyia olmeca in the New World, where it typically affects rubber workers and in over 50% of cases results in the formation of an ulcerated lesion on the pinna known as a chiclero ulcer.1,2,5,6
Occasionally these atypical presentations can simulate other infectious or inflammatory skin conditions. The erysipeloid form, of which few cases are described in the literature, is characterized by poorly defined erythematous plaques that resemble those seen in erysipelas or cellulitis.2,7,8 In our patients, who had erythematous and indurated plaques on the shoulder and pinna, respectively, the initial diagnostic suspicions were cellulitis and erysipelas, respectively. Both patients responded poorly to subsequent antibiotic treatment.
Although suspected CL is often diagnosed clinically, diagnosis should be confirmed using microbiological (Leishmania culture in special media, direct examination, PCR of tissue and/or blood samples) and/or histological techniques.9,10
Skin ultrasound is a fast, safe, and effective technique, and is increasingly used in dermatology. We have found no published descriptions of ultrasound findings in CL patients.
In our patients, ultrasound revealed diffuse thickening of the dermis in the first case, accompanied in the second case by a poorly defined and vascularized structure in the superficial dermis and an increase in the thickness of the dermis. These alterations resolved after treatment.
Although the ultrasound findings were nonspecific, ultrasound served as a useful additional diagnostic tool to identify dermal alterations and increased Doppler flow. More importantly, in both cases it allowed us to monitor the treatment response, and revealed resolution of the structural alterations in the subepidermal tissue. This would not have been possible by visual examination.
We describe 2 cases of erysipeloid CL. CL should be included in the differential diagnosis of lesions suggestive of erysipelas or cellulitis that do not respond to conventional antibiotics.
We wish to highlight the role of ultrasound in these cases not only as an additional diagnostic technique, but also as a means of monitoring treatment response.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rojas Mora E, Garrido Ríos A, Echeverría García B, Borbujo J. Leishmaniasis cutánea de presentación inusual. Papel de la ecografía cutánea. Actas Dermosifiliogr. 2019;110:171–174.