The term primary cutaneous amyloidosis (PCA) refers to a group of diseases caused by the extracellular deposition of amyloid in the skin without the involvement of other organs. PCA has been divided into the following types: macular, lichen and nodular. The first 2 types are characterized by the deposition in the papillary dermis of amyloid derived from the degeneration of keratin filaments. Primary localized cutaneous nodular amyloidosis (PLCNA) is the rarest form of PCA and the only one in which the amyloid deposits are of the amyloid light-chain (AL) type, as in the primary and myeloma-associated systemic forms of amyloidosis. AL amyloidosis is due to monoclonal immunoglobulin (Ig) light-chain deposition.
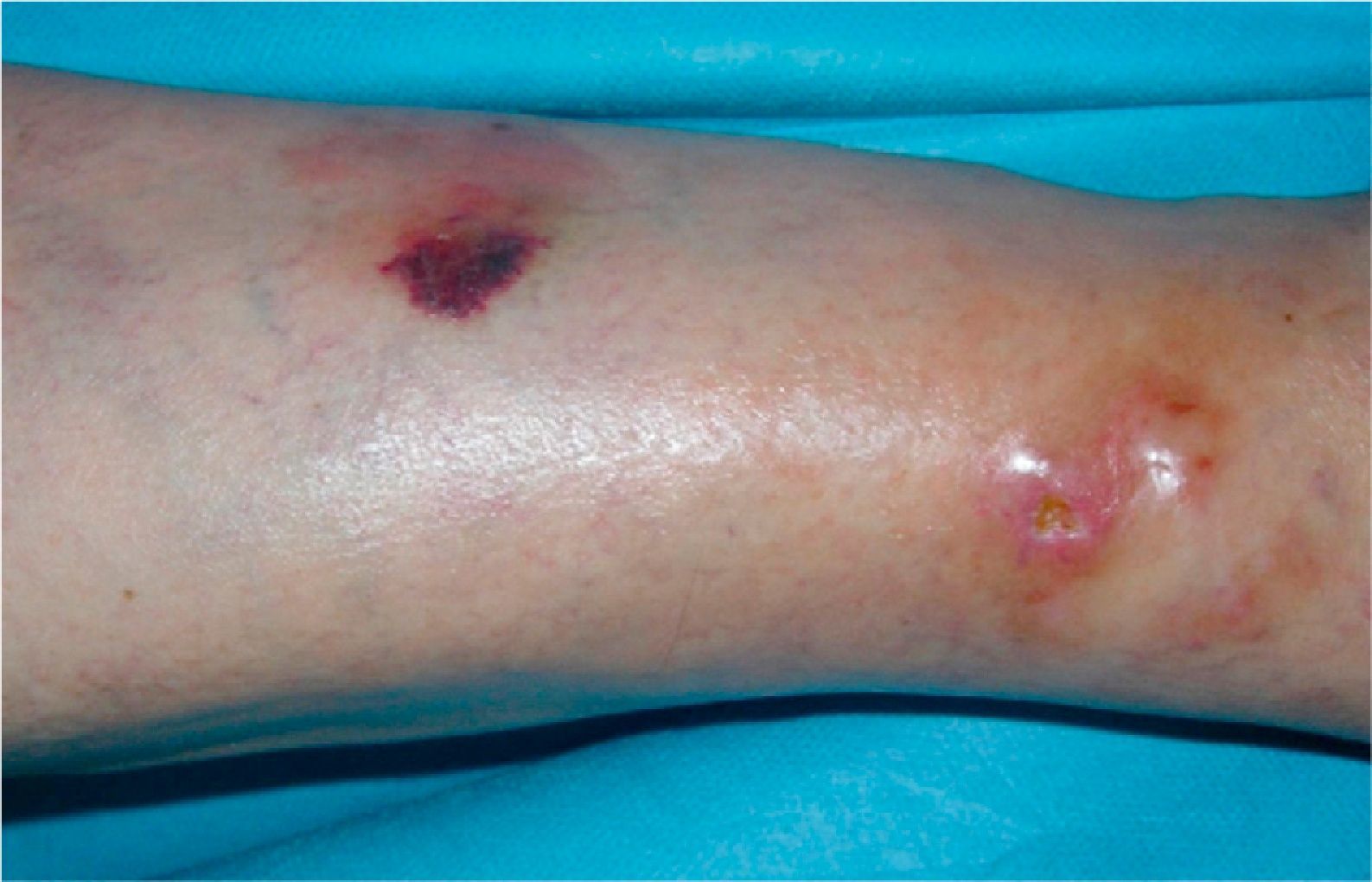
We report the case of an 83-year-old man with a history of systemic hypertension, type 2 diabetes mellitus, and hyperuricemia, who was seen for a 2-year history of asymptomatic but progressive lesions that had appeared on the left lower limb. One year before consultation, he had been diagnosed with monoclonal gammopathy of undetermined significance (MGUS), after detecting an IgG(κ) paraprotein in the serum with no evidence of multiple myeloma in the bone marrow study. Physical examination revealed a plaque with an area of ecchymotic appearance and several hard, reddish-orange nodules with an ulcerated surface in the pretibial region of the left leg (Fig. 1).
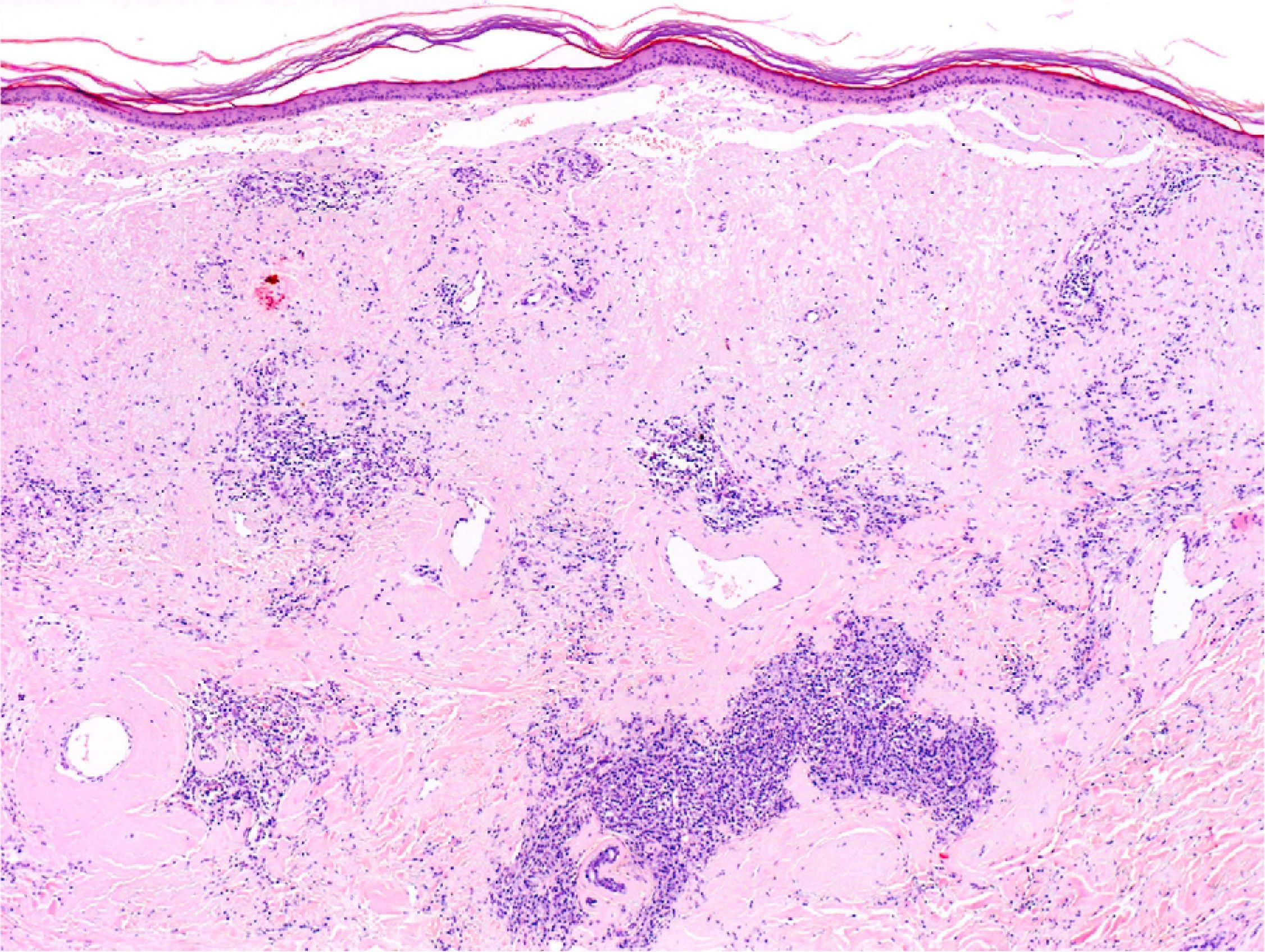
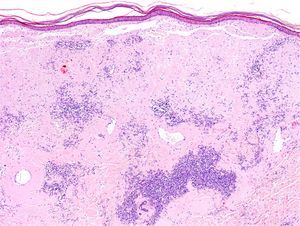
Histopathological examination showed deposits of an amorphous eosinophilic material diffusely distributed through the papillary and reticular dermis, extending into the subcutaneous tissue, accompanied by a dense infiltrate of plasma cells (Fig. 2). When stained with thioflavin, the deposits fluoresced under ultraviolet light. Immunohistochemical staining demonstrated λ light-chain restriction in the majority of the plasma cells. These findings suggested a possible diagnosis of PLCNA, although systemic amyloidosis could not be ruled out.
Laboratory tests including complete blood count, biochemistry tests, and liver and kidney profiles were normal. Immunoglobulin concentrations were normal, although the IgG value was at the upper limit of normal: 1590mg/dL (normal range, 700–1600mg/dL). Immunoelectrophoresis showed a monoclonal IgG(κ) band with oligoclonal λ bands in the serum, but was normal in the urine. No amyloid deposits were observed in a biopsy of the abdominal fat. After 18 months of follow-up, the patient has not shown evidence of progression to myeloma or systemic amyloidosis.
PLCNA is a disease that occurs predominantly in women, with a mean age at diagnosis of 60 years.1 It has sometimes been described in association with systemic diseases such as Sjögren syndrome,2 diabetes mellitus, or CREST syndrome.3 It manifests as waxy nodules that are usually solitary or localized or, less commonly, disseminated.4 It tends to affect acral areas, the most common site being the lower limbs, followed by the face and trunk. Histopathological findings are indistinguishable from those of primary systemic amyloidosis or myeloma-associated amyloidosis.5 Immunohistochemical staining may show the presence of immunoglobulin light chains in the amyloid or in the cytoplasm of plasma cells.
Based on the demonstration of clonality of the plasma cell infiltrate in the skin using gene rearrangement techniques and on the absence of clonal rearrangement in bone marrow, some authors have suggested that PLCNA should be considered an extramedullary plasmacytoma that produces localized amyloid deposition.6 Extramedullary plasmacytomas are plasma cell neoplasms that arise in any organ except bone marrow; they are able to produce an M-component in the serum in up to 20% of cases.7 Extramedullary plasmacytomas that initially do not produce the M-component in serum progress to multiple myeloma in 20% of cases.8
In our patient, there was a monoclonal infiltrate of plasma cells that synthesized λ chains and produced the amyloid deposits in the skin, and a finding of a monoclonal IgG(κ) band and oligoclonal λ bands in the serum. This suggests a biclonal gammopathy (the presence of 2 monoclonal components in serum), which has been observed in approximately 3% of MGUS.9
The appearance of paraproteinemia in cases of PLCNA has rarely been described in the literature, though it should always be investigated at the initial assessment. In the cases in which it has been observed, it was generally associated with an advanced stage of the disease, and may indicate progression to systemic amyloidosis.10
The risk of progression to systemic amyloidosis in PLCNA has been well defined by several authors. Since 1970, the risk has been established at around 50%. However, in 2001, Woollons and Black5 observed only 1 case of progression to systemic amyloidosis in a series of 15 patients with PLCNA, in addition to high immunoglobulin concentrations in 40% of cases. In 2003, Moon et al.10 obtained similar results after 10 years of follow-up in 16 patients with PLCNA and reported progression in the only patient presenting with paraproteinemia at the time of diagnosis.
Despite its generally benign course, it is important to follow-up these patients closely, especially in cases associated with paraproteinemia, to monitor for possible progression to systemic amyloidosis and to exclude plasma cell dyscrasias.
Please cite this article as: Villar M, et al. Amiloidosis nodular primaria cutánea localizada en un pacinete con paraproteinemia. Actas Dermosifiliogr. 2012;103:161–2.