Hair transplantation is a continuously evolving field. Since 1959, when Orentreich1 described the phenomenon of donor dominance in androgenic alopecia, thus paving the way for body-hair transplants, new techniques have not ceased to appear. During the last 15 years, the perception of hair transplantation as an aggressive technique with an artificial result has finally disappeared thanks to the use of follicular units, which have made the technique minimally invasive with mostly acceptable results.2–4
We present the case of a 30-year-old man with Norwood class III alopecia who underwent hair transplantation at another center in 2008 with the strip method, by means of which he received 3800 follicular units in the frontoparietal region. The follicular units were harvested from the parieto-occipital region.
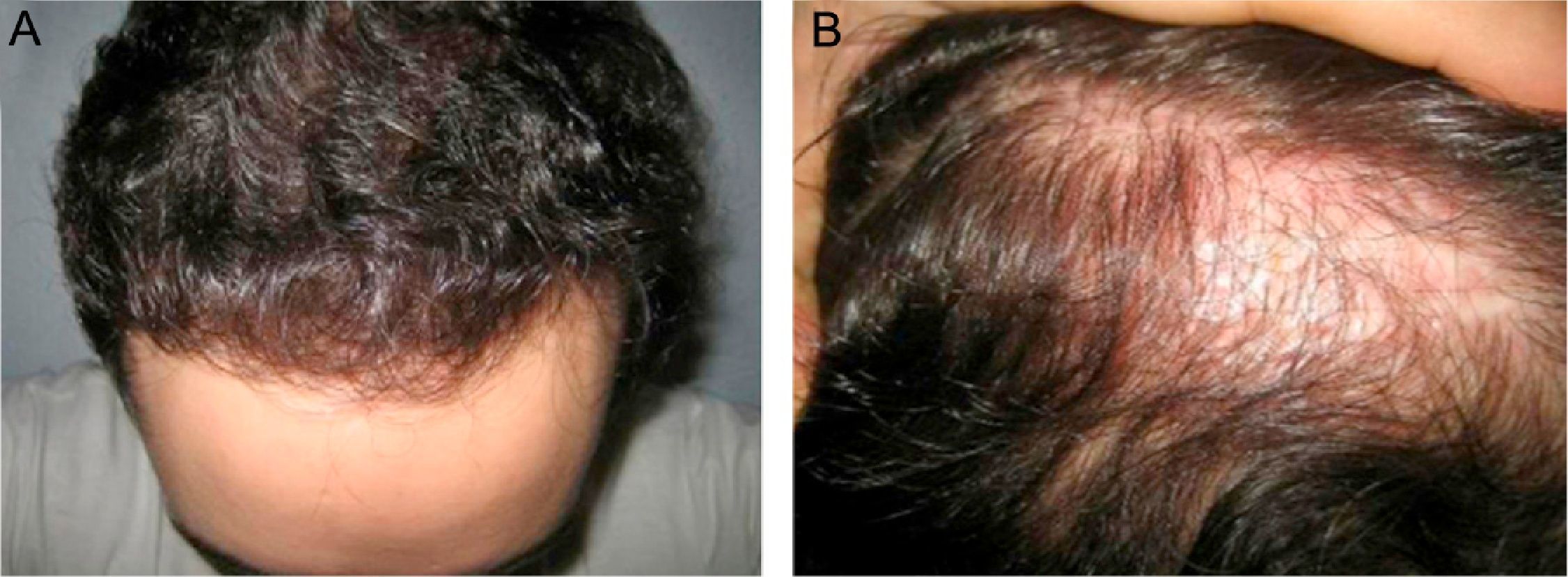
He consulted 1.5 years after the intervention for assessment of the reconstruction of the donor strip scar (3cm×2cm) and reinforcement of the frontal area behind the hairline (Fig. 1A and B).
We considered the possibility of using the occipital region as the donor strip. However, the low follicular density (50units/cm2) at this site led us to repopulate the frontal area using a combination of follicular units from the occipital region and chest. This approach provided a reasonable number of follicles.
Follicular units were obtained using a 0.8-mm punch after applying local anesthetic with 2% lidocaine with 1:100,000 epinephrine. A total of 335 follicular units were obtained from the chest (Fig. 2A) and 600 from the parieto-occipital region.
Once the recipient site had been anesthetized, the incisions were made in the scar area using a 19G needle, and the body hair follicular units were implanted at a density of 17units/cm2.
Of the 335 follicular units obtained, 100 were implanted in the scar of the parietotemporal area to evaluate the response (Fig. 2B), and the remaining body-hair units plus the 600 units from the parieto-occipital region were implanted in the frontal region.
Evaluation at 4 and 6 months after treatment revealed that more than 80% of the units had survived in the scar; the hair was practically indistinguishable from the scalp hair in terms of thickness and length (Fig. 3A and B). The donor area on the chest healed correctly without visible scars or keloids, thus leaving the patient with a very satisfactory cosmetic outcome.
Cicatricial alopecia resulting from burns, surgery, injury, or radiotherapy is an excellent indication for hair transplantation.5–7 Our patient developed an iatrogenic parietal scar after a “megasession” of follicle donation, possibly because the donor strip was larger than generally recommended in order to harvest as many follicles as possible. The therapeutic alternatives we considered to rebuild the scar were implantation of a tissue expander and direct closure, which the patient rejected, or a follicular unit transplant on the scar.
One of the precautions to be taken into account when performing a hair transplant on a scar is that the density in units/cm2 must be less than on an area of normal skin (30–40units/cm2), because of the risk of follicles competing for the reduced blood flow through the scar tissue.
In conventional hair transplantation, the donor strip is limited to the scalp. However, the follicular unit extraction technique enables body hair to be transplanted to the scalp: instead of removing the strip, the follicular units are extracted individually using circular punches measuring 0.7–1mm in diameter. The punch holes heal by second intention within a few days.
Transplantation of body hair follicular units has been described in the literature,4,5 which addresses the concept of “recipient-dominance”. In other words, the body hair that is transplanted takes on the characteristics of the hair at the receptor site5,8,9; better results are achieved with follicular units from the beard and chest.
While it is true that the chest is prone to keloids and that this should be taken into account and the patient informed, there have been no reports of keloids in white patients after follicular unit extraction using a punch.
Transplantation of body hair follicles is still a controversial technique with few published case reports. Nevertheless, we present this case of cicatricial alopecia, because, although the density obtained to cover the scar is not yet sufficient, we did observe a good growth rate for the body hair. We believe that it is important for the dermatologist to be aware of the usefulness and potential of hair transplantation, since we are often faced with patients who have not been adequately informed about the technique or who have even been discouraged by the specialist.
Please cite this article as: Meyer-González T, Bisanga C. Reconstrucción de alopecia cicatricial mediante transplante de pelo corporal. Actas Dermosifiliogr. 2012;103:163–164.