We read with interest the report by Horcajada-Reales et al.1 of 2 cases with overlapping clinical characteristics involving acute generalized exanthematous pustulosis (AGEP) and toxic epidermal necrolysis (TEN). We would like to share a similar case we encountered in our practice.
AGEP and TEN are well-established, distinct entities belonging to the group of severe cutaneous drug reactions. They both have characteristic clinical presentations and differ in pathogenesis, prognosis, and treatment. It is, however, sometimes hard to distinguish between the 2 conditions and this difficulty can lead to an erroneous clinical diagnosis.
AGEP is a skin condition generally associated with a good prognosis. It typically presents as a rapidly evolving pustular eruption accompanied by fever and leukocytosis with neutrophilia. A skin biopsy reveals a subcorneal pustule.
TEN, on the other hand, often affects the mucous membranes and is accompanied by fever and generalized discomfort, which precedes the appearance of eythematous-violaceous exanthema and epidermal detachment. Histological findings include epidermal necrosis and apoptotic keratinocytes.
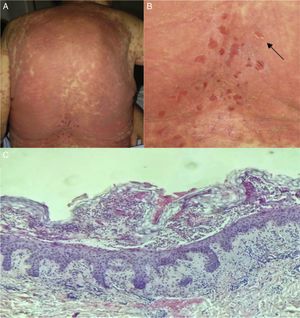
Our patient was an 82-year-old woman with no known allergies. She was admitted to hospital because of a 39°C fever and a violaceous exanthema mainly affecting the trunk. The eruption was characterized by skin detachment in some areas and a positive Nikolski sign (Figs. 1A and 1B). Laboratory testing revealed elevated transaminase levels: gamma glutamyl-transferase (GGT), 494 U/L; fatty acid (FA), 364 U/L; glutamic-oxalacetic transaminase (GOT), 91 U/L; and glutamic-pyruvic transaminase (GPT), 99 U/L.
Two weeks before admission she had been diagnosed with acute self-limited gastroenteritis and treated with trimethoprim sulfamethoxazole. The only personal medical history of interest was dyslipidemia.
Piperacillin-tazobactam was prescribed for a suspected biliary tract infection and cholangio-magnetic resonance imaging revealed a small extrahepatic bile duct ectasia. The results of blood cultures were negative. Enterococcus faecalis was isolated in a urine culture. Serology was negative for hepatitis A, B and C and HIV.
Given the suspected diagnosis of TEN secondary to sulfamethoxazole or cotrimoxazole, corticosteroids (prednisone 60mg/d for 5 days) and intravenous immunoglobulins (1g/kg/d for 2 days) were prescribed and achieved an excellent clinical response (complete resolution of the condition within 8 days).
Histological study revealed subcorneal pustules with abundant neutrophils, both findings consistent with a diagnosis of generalized exanthematous pustulosis (Fig 1C).
The possibility of different severe adverse drug reactions overlapping is a subject of some debate. Although they are distinct entities, the clinical features can be similar and have certain pathophysiologic mechanisms in common.
AGEP, for instance, can present with vesicular-bullous lesions that mimic the clinical appearance of TEN.2 There are also forms of TEN that manifest as pustules or blisters.
Cases have been reported of patients who, after initially presenting with AGEP, subsequently developed TEN.1 In other cases, such as the one described here, the patient presents the clinical features of TEN with histological findings consistent with AGEP.
There are 17 published cases of overlapping forms, most of which are associated with antibiotic use.1
The main differences between AGEP and TEN are shown in Table 1.3
Main Differences Between Acute Generalized Exanthematous Pustulosis (AGEP) and Toxic Epidermal Necrolysis (TEN).
| Variable | AGEP | TEN |
|---|---|---|
| Site | Flexural | Generalized |
| Pustules | Yes | No |
| Nikolsky+ | Rare | Frequent |
| Mucosal involvement | + oral mucosa | ++++ |
| Fever | Occasionally | Frequent high fever |
| Blood test results | Neutrophilia | Neutropenia and elevated transaminases |
| Latency period | Hours or days | 2-3 wks |
| Histopathology | Subcorneal pustules | Epidermal necrosis |
| Treatment | Withdrawal of the drug | Drug withdrawal and Intravenous immunoglobulins |
| Recovery | 15 d | 3-6 wks |
| Mortality | Rare | 30% |
In terms of pathogenesis, it seems clear that both conditions are type 4 hypersensitivity reactions (HSR) and that the difference between them lies in the type of T-cell activated in each case.4 In both cases, the initial stage is characterized by keratinocyte cytolysis caused by CD8+ T cells. Subsequently, the two conditions diverge and the pathway differs in each one. In AGEP, activated CD4+ T cells produce interleukin (IL) 8, IL-17 and IL-36, which recruit neutrophils and lead to the formation of pustules (type 4d HSR).5
In TEN, by contrast, CD8+ T cells release perforin and granzyme B, triggering massive keratinocyte apoptosis by activating the Fas-Fas-ligand receptor and tumor necrosis factor alpha (TNF-α) (type 4c HSR). The latest research is focused on the investigation of certain drug-specific human leukocyte antigens (HLA) that predispose individuals to a genetic susceptibility for TEN when an individual with a specific HLA allele is exposed to a specific drug.5
Overlapping forms are probably caused by a combined hypersensitivity reaction between such alleles and a specific drug.
In most cases, the eventual course of the disease will be AGEP. However, in some patients it has led to extensive skin lesions, multiorgan involvement, and even death.6
It is important to recognize these cases because, given their greater severity, they should be managed and treated as TEN.
Please cite this article as: García Abellán J, Matarredona Catalá J, Jaen Larrieu A, Valencia Ramírez I. Pustulosis exantemática generalizada aguda simulando necrólisis epidérmica tóxica: forma combinada. Actas Dermosifiliogr. 2018;109:460–462.