At present, Alzheimer disease has no effective treatment due to its complex pathophysiology, which is not yet completely understood. However, abnormal cholinergic function has been shown to play an important role in the many types of brain neurotransmitter dysfunction found in Alzheimer patients. Accordingly, cholinesterase inhibitors that strengthen cholinergic neurotransmission, including galantamine, donepezil, and rivastigmine, are considered first-line drugs for the treatment of mild to moderate Alzheimer disease.
We present the first reported case of acute generalized exanthematous pustulosis (AGEP) following the administration of galantamine.
An 81-year-old woman with a history of hypertension, dyslipidemia, spondyloarthropathy, and recently diagnosed Alzheimer-type degenerative dementia was brought to our department for emergency examination. She presented with a generalized itchy skin rash that had developed 5 days earlier, associated with a sensation of poor temperature regulation and no measurable fever.
The physical examination showed large erythematous, edematous plaques on the trunk and limbs with multiple nonfollicular monomorphic pustules. The lesions on the limbs were more isolated and had a target morphology (Fig. 1). Small isolated areas of superficial epidermal detachment were also observed.
No involvement of the oral or genital mucosa or ocular discomfort was observed. Palpation did not reveal visceromegaly or enlarged lymph nodes.
The only relevant recent change in medication was the addition of galantamine, which had been prescribed by the neurologist in the preceding month to treat the patient's dementia. Galantamine was being administered in increasing doses and the dosage of all other drugs had not changed.
Based on the suspected diagnosis of AGEP induced by galantamine, the patient was admitted to hospital for monitoring and treatment with the drug was discontinued. Her symptoms were treated with fluid therapy, oral antihistamines, and local dressings.
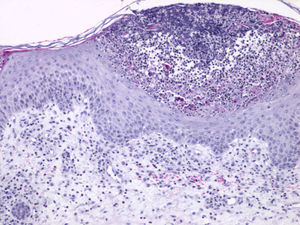
Histology revealed subcorneal pustules filled with neutrophils, edema in the papillary dermis, and a slight perivascular infiltrate of lymphocytes and eosinophils (Fig. 2).
Blood tests showed intense leukocytosis (38 × 109/L) with neutrophilia (34.6 × 109/L), normal blood cell morphology, and increased levels of acute phase reactants, including fibrinogen and C-reactive protein.
During her stay in hospital, the patient's condition improved rapidly with a reduction in rash severity, no progression of the de-epidermized areas, and a return to normal blood test results. On examination 2 weeks after withdrawal of galantamine the lesions had completely disappeared and only slight superficial scaling was observed.
AGEP is a rare condition characterized by an initially acute nonbacterial pustular rash that is frequently febrile and resolves quickly and spontaneously.
Over 90% of AGEP cases are induced by medication, mainly antibiotics such as macrolides and β-lactams.1 Other drugs associated with AGEP include nonsteroidal anti-inflammatory drugs, antimycotics, calcium channel blockers, paracetamol, carbamazepine, and hydroxychloroquine.2,3
Based on the frequently positive patch test results reported in these patients, the presence of neutrophilia in peripheral blood, and the accumulation of neutrophils in the lesions, it is currently believed that AGEP is mediated by T cells. However, the specific underlying mechanism of this condition is still unknown.
Clinically, AGEP presents as a febrile pustular rash that appears suddenly and is preceded by an itching or burning sensation that starts on the face and intertriginous areas and spreads to the trunk and limbs.4 Typically, hundreds of sterile nonfollicular pustules (<5mm) develop on large erythematous, edematous areas. The lesions sometimes develop an erythema multiforme-like target morphology, as was the case in our patient.
Following withdrawal of the drug, generalized superficial scaling develops and the lesions completely resolve, usually after a period of 2 weeks.
The most frequent laboratory findings are intense leukocytosis with neutrophilia and, occasionally, eosinophilia.5
Characteristic histologic findings include subcorneal spongiform pustules associated with foci of necrotic keratinocytes, edema in the papillary dermis, and perivascular infiltrate containing lymphocytes, neutrophils, and a few eosinophils.
A diagnosis of AGEP is based on a combination of medication history, clinical course, and pathologic findings. Patch tests are a useful way to confirm the diagnosis, although it should be noted that the results are positive in only 50% of cases.4,6
Treatment consists of withdrawing the causative agent and symptomatic treatment with antihistamines, antipyretics, or topical corticosteroids.
In our review of the literature we found no reported cases of AGEP induced by galantamine, although there are reports involving other cholinergic drugs, including varenicline, a partial agonist of the receptor acetylcholine that was approved by the FDA in 2006 for the treatment of tobacco addiction.7,8
In our patient the diagnosis was based on clinical, histologic, and laboratory criteria. We identified galantamine as the probable cause because of its recent introduction, the absence of any other triggering agents, and the rapid resolution of the symptoms upon withdrawal of the drug.
We present this case because it involves an emergent drug being used to treat Alzheimer disease, a condition that has recently been reported to affect 5% to 10% of the Spanish population over 65 years of age.
Please cite this article as: Pérez-García MP, Sánchez Motillas JM, Mateu-Puchades A, Díaz-Corpas T. Pustulosis exantemática aguda generalizada inducida por galantamina. Actas Dermosifiliogr. 2013;104:930–931.