Acquired perforating dermatosis (APD) is an uncommon disease characterized by lesions exhibiting transepidermal elimination of collagen or elastic fibers. APD affects adults and is associated with systemic diseases, mainly diabetes mellitus and renal failure.
We present 8 cases of APD. Seven patients had concomitant diabetes mellitus with or without chronic renal failure, and 1 had alcoholic cirrhosis. In the patients with chronic renal failure, the onset of APD coincided with transient worsening of renal function. The mean increase in creatinine concentrations above baseline was 1.14mg/dL. Acute deterioration of renal function may be involved in APD. Further studies are needed to investigate this association.
La dermatosis perforante adquirida (DPA) es una enfermedad infrecuente caracterizada por la aparición de lesiones que presentan eliminación transepidérmica de colágeno o fibras elásticas. Afecta a adultos y se asocia a enfermedades sistémicas, principalmente diabetes mellitus e insuficiencia renal.
Presentamos 8 casos de DPA, 7 con diabetes mellitus e insuficiencia renal crónica (IRC) y uno con cirrosis alcohólica. Los pacientes con IRC tuvieron un empeoramiento transitorio de la misma coincidiendo con la aparición de la DPA. La creatinina se elevó de media 1,14mg/dl. El deterioro agudo de la función renal podría estar implicado en la DPA. Se necesitan más estudios para confirmar esta relación.
The perforating dermatoses are a heterogeneous group of diseases characterized by the transepidermal elimination of one or more components of the skin. Four types are traditionally recognized: elastosis perforans serpiginosum, perforating folliculitis, Kyrle disease, and reactive perforating collagenosis (RPC). Two variants of RPC have been described: a rare hereditary form that presents in childhood and a more common acquired form that appears in adult life and mainly affects diabetic patients with chronic renal failure (CRF).1 Over the years, there has been a degree of confusion regarding the terminology. At the present time, the majority of authors use the term reactive perforating collagenosis for the hereditary form, while the term acquired perforating dermatosis (APD), proposed by Rapini et al., is preferred for the adult form and for any perforating disease that is clinically and histologically similar to the primary disease but that is associated with a systemic disease.1
APD is a rare disease. The majority of descriptions are in the form of isolated case reports; a few case series exist.2–4 We present a series of 8 cases.
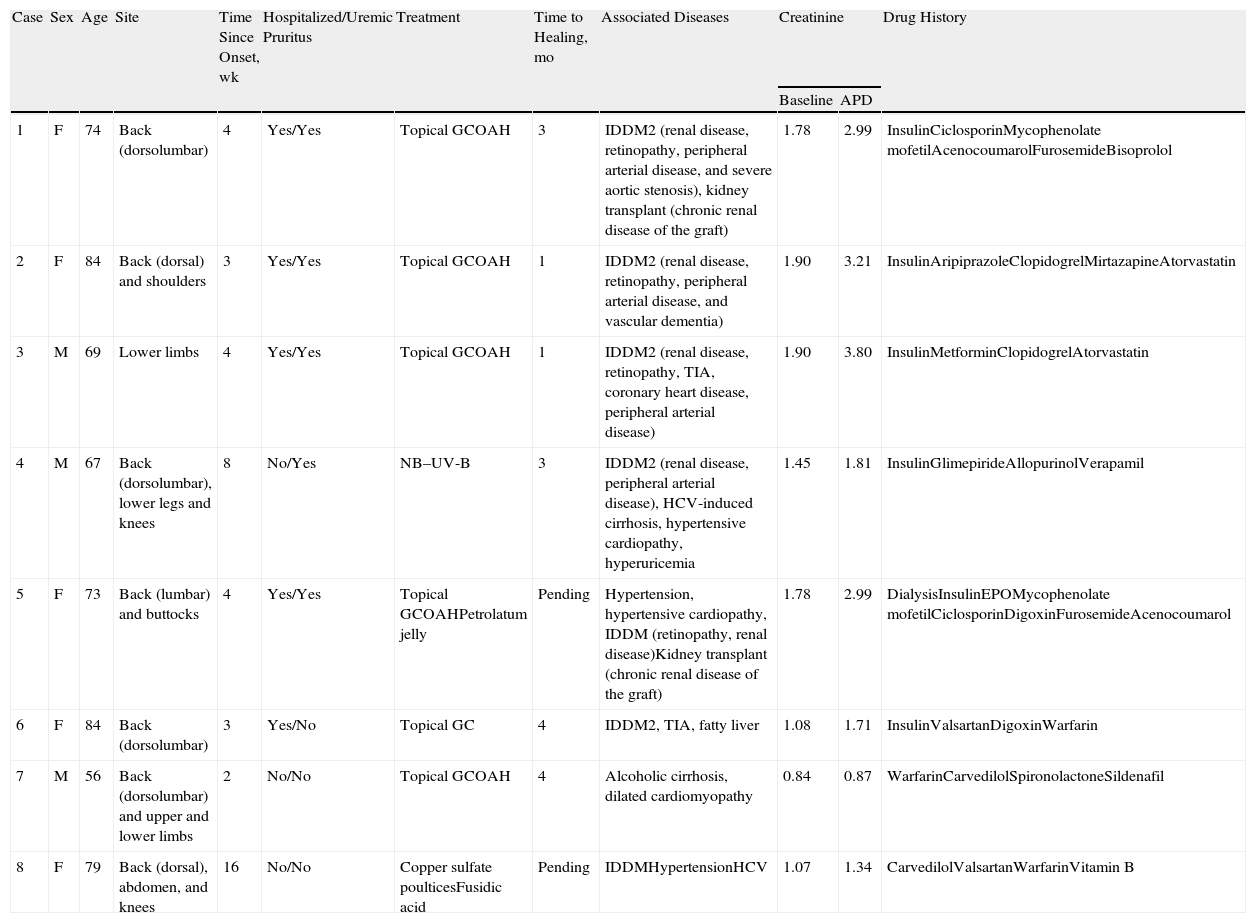
Case DescriptionsWe present 8 cases of APD in 3 men and 5 women with a mean age of 73 years (Table 1). The time from the onset of symptoms to diagnosis varied between 2 weeks and 4 months, with a mean of 5.5 weeks.
Case Descriptions.
| Case | Sex | Age | Site | Time Since Onset, wk | Hospitalized/Uremic Pruritus | Treatment | Time to Healing, mo | Associated Diseases | Creatinine | Drug History | |
| Baseline | APD | ||||||||||
| 1 | F | 74 | Back (dorsolumbar) | 4 | Yes/Yes | Topical GCOAH | 3 | IDDM2 (renal disease, retinopathy, peripheral arterial disease, and severe aortic stenosis), kidney transplant (chronic renal disease of the graft) | 1.78 | 2.99 | InsulinCiclosporinMycophenolate mofetilAcenocoumarolFurosemideBisoprolol |
| 2 | F | 84 | Back (dorsal) and shoulders | 3 | Yes/Yes | Topical GCOAH | 1 | IDDM2 (renal disease, retinopathy, peripheral arterial disease, and vascular dementia) | 1.90 | 3.21 | InsulinAripiprazoleClopidogrelMirtazapineAtorvastatin |
| 3 | M | 69 | Lower limbs | 4 | Yes/Yes | Topical GCOAH | 1 | IDDM2 (renal disease, retinopathy, TIA, coronary heart disease, peripheral arterial disease) | 1.90 | 3.80 | InsulinMetforminClopidogrelAtorvastatin |
| 4 | M | 67 | Back (dorsolumbar), lower legs and knees | 8 | No/Yes | NB–UV-B | 3 | IDDM2 (renal disease, peripheral arterial disease), HCV-induced cirrhosis, hypertensive cardiopathy, hyperuricemia | 1.45 | 1.81 | InsulinGlimepirideAllopurinolVerapamil |
| 5 | F | 73 | Back (lumbar) and buttocks | 4 | Yes/Yes | Topical GCOAHPetrolatum jelly | Pending | Hypertension, hypertensive cardiopathy, IDDM (retinopathy, renal disease)Kidney transplant (chronic renal disease of the graft) | 1.78 | 2.99 | DialysisInsulinEPOMycophenolate mofetilCiclosporinDigoxinFurosemideAcenocoumarol |
| 6 | F | 84 | Back (dorsolumbar) | 3 | Yes/No | Topical GC | 4 | IDDM2, TIA, fatty liver | 1.08 | 1.71 | InsulinValsartanDigoxinWarfarin |
| 7 | M | 56 | Back (dorsolumbar) and upper and lower limbs | 2 | No/No | Topical GCOAH | 4 | Alcoholic cirrhosis, dilated cardiomyopathy | 0.84 | 0.87 | WarfarinCarvedilolSpironolactoneSildenafil |
| 8 | F | 79 | Back (dorsal), abdomen, and knees | 16 | No/No | Copper sulfate poulticesFusidic acid | Pending | IDDMHypertensionHCV | 1.07 | 1.34 | CarvedilolValsartanWarfarinVitamin B |
Abbreviations: EPO, erythropoietin; GC, glucocorticoid; HCV, hepatitis C virus; IDDM2, insulin-dependent type 2 diabetes mellitus; NB–UV-B, narrowband UV-B; OAH, oral antihistamines; TIA, transient ischemic attack.
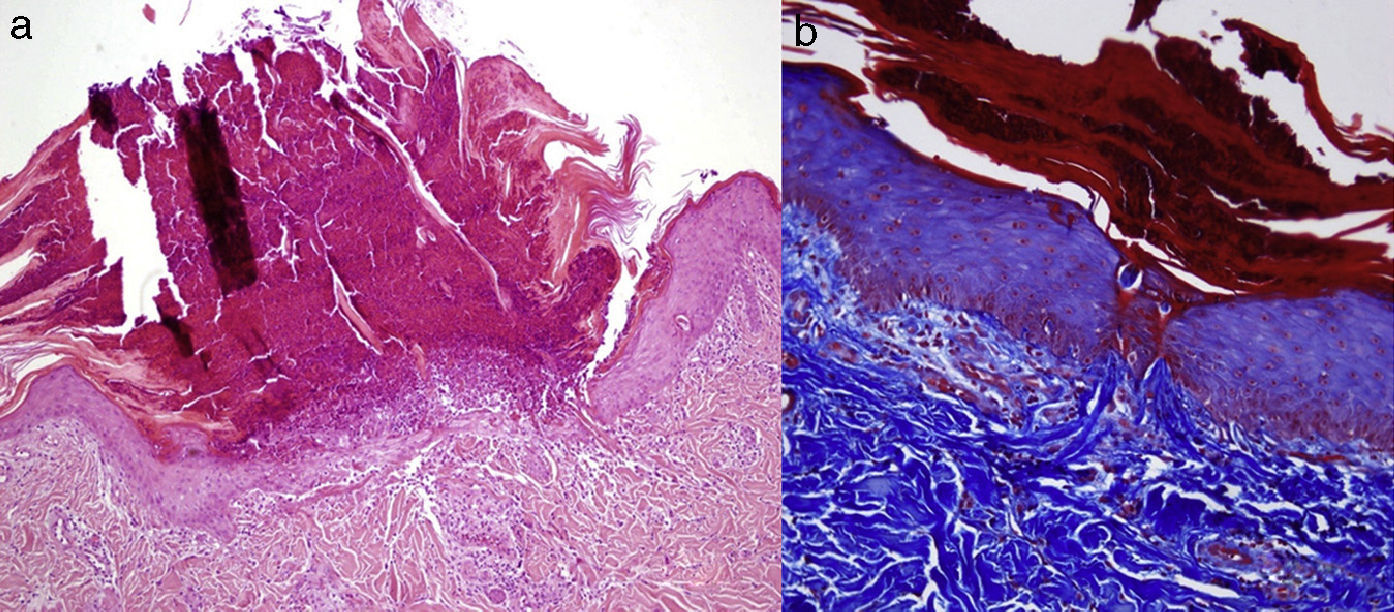
Clinically, patients presented multiple umbilicated papules that were highly pruritic and had a firmly adherent central keratotic plug (Figs. 1 and 2). The most common sites were the back and the lower limbs. Histopathology study, performed in all patients using hematoxylin-eosin, Masson trichromic, and Verhoeff stains, revealed epidermal hyperplasia with a cup-shaped central depression covered by keratin and cell remnants, as well as the transepidermal elimination of verticalized collagen fibers (Fig. 3, A andB). The elimination of elastic fibers was not detected in any of the patients. All patients satisfied the diagnostic criteria proposed by Faver: umbilicated papules or nodules with an adherent center of keratotic appearance, histopathological identification of the elimination of basophilic collagen, and onset of the skin lesions after 18 years of age.5 Diabetes mellitus (DM), with or without CRF, was the most common association and was present in 7 cases. Three patients had liver disease (fatty liver, alcoholic cirrhosis, and hepatitis C virus-induced chronic liver disease).
Larger lesions than in Figure 1, in this case on the back of patient 8.
All the patients with DM and/or CRF presented a deterioration of renal function coinciding with the onset of the skin lesions. The increase in the creatinine level was of 0.36-1.90mg/dL, with a mean elevation of 1.14mg/dL with respect to baseline levels, and the levels returned to baseline in the follow-up laboratory tests at 1 to 2 months. The majority of our cases were treated with topical corticosteroids and antihistamines; 1 patient received narrowband UV-B and another received topical antibiotics and copper sulfate poultices. The lesions resolved in 1 to 4 months (mean, 2.6 months), leaving residual hyperpigmented scars. Follow-up at 1 year revealed no new lesions.
DiscussionThe term acquired perforating dermatosis, introduced in 1989 by Rapini et al.,6 refers to the perforating dermatoses that appear in adults and are associated with systemic diseases (mainly DM and CRF). Publications prior to the study by Rapini et al. used other terms to refer to this disease (Kyrle-like lesions, perforating folliculitis of hemodialysis, Kyrle disease in patients with CRF, uremic follicular hyperkeratosis, perforating pseudoxanthoma elasticum associated with CRF and hemodialysis, elastosis perforans serpiginosum, and reactive perforating collagenosis of DM and CRF7–9), exacerbating the confusion that has surrounded this disease up to now. APD presents as a rash of umbilicated papules with a central keratotic cap and is associated with widespread pruritus. The most common sites are the trunk and limbs, usually in areas accessible to scratching and sometimes show a linear distribution, as manifestations of the Koebner phenomenon.
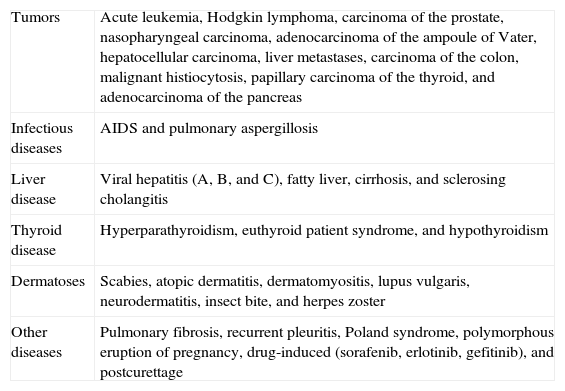
Histopathology reveals findings of any of the 4 classic perforating diseases, and more than 1 pattern may be observed in a single patient.2,6 APD has been reported in association with numerous systemic diseases (Table 2). A typical case would be a patient with DM and CRF of diabetic origin. The DM is usually long-standing, and micro- and macroangiopathic complications may be present.6,10 But other causes of CRF, such as human immunodeficiency virus infection,6 immunoglobulin A nephropathy, glomerulonephritis, and heroin abuse have also been described.10 APD can develop during the course of various liver diseases without accompanying DM and/or CRF, as occurred in case 7 in our series. These liver diseases include viral hepatitis (hepatitis A, B, or C viruses), fatty liver,2 cirrhosis, hepatocellular carcinoma, and liver metastases.
Associated Systemic Diseases.
| Tumors | Acute leukemia, Hodgkin lymphoma, carcinoma of the prostate, nasopharyngeal carcinoma, adenocarcinoma of the ampoule of Vater, hepatocellular carcinoma, liver metastases, carcinoma of the colon, malignant histiocytosis, papillary carcinoma of the thyroid, and adenocarcinoma of the pancreas |
| Infectious diseases | AIDS and pulmonary aspergillosis |
| Liver disease | Viral hepatitis (A, B, and C), fatty liver, cirrhosis, and sclerosing cholangitis |
| Thyroid disease | Hyperparathyroidism, euthyroid patient syndrome, and hypothyroidism |
| Dermatoses | Scabies, atopic dermatitis, dermatomyositis, lupus vulgaris, neurodermatitis, insect bite, and herpes zoster |
| Other diseases | Pulmonary fibrosis, recurrent pleuritis, Poland syndrome, polymorphous eruption of pregnancy, drug-induced (sorafenib, erlotinib, gefitinib), and postcurettage |
Our 7 patients with DM and/or CRF presented a deterioration of renal function coinciding with the onset of the skin lesions. In a review of the literature we found no data to suggest that creatinine levels can play a role in the onset of APD or of uremic pruritus. The temporal coincidence of the elevation of the creatinine levels and the onset of the APD lesions observed in our patients would suggest that there may be a relationship between the acute deterioration of renal function and APD in patients with CRF and/or DM. However, because of the small number of patients in our series, we cannot establish a firm causal relationship between the acute deterioration of renal function and the onset of APD. Studies with a larger number of patients would be necessary to confirm this association.
The pathogenesis of APD is not fully understood. The most widely accepted hypothesis involves pruritus as the principal trigger, as it is present in all cases. Scratching produces microtrauma that leads to changes in the collagen fibers of the papillary dermis, facilitating their transepidermal elimination as the final stage.2,6 Numerous skin or systemic diseases that provoke pruritus and scratching can therefore lead to the onset of APD in patients with underlying metabolic changes.11 Some publications have related the onset of APD to dialysis,10 but it has subsequently been shown that APD can occur both before and after dialysis. In addition, APD can appear in patients on hemodialysis, peritoneal dialysis, or even in patients without dialysis.7,10 Although an improvement in APD lesions has been reported after kidney transplant, APD lesions have developed after transplant in some patients, as occurred in cases 1 and 5 in our series, coinciding with a deterioration in graft function.2
Numerous treatments for APD have been described, aimed mainly at controlling the pruritus.1 The most widely used are emollients, keratolytics, topical retinoids, topical, oral, or intradermal corticosteroids, phototherapy (broadband and narrowband UV-B), photochemotherapy (psoralen–UV-A),12and allopurinol.1 Other options, including oral retinoids, doxycycline, rifampicin, amitriptyline, surgical debridement, electrical nerve stimulation, photodynamic therapy, and topical cantharidin, have produced satisfactory results in isolated cases.
APD develops in patients with widespread pruritus and systemic diseases, the most common association being with DM and CRF. We present a series of 8 cases of APD, 7 with DM, of whom 5 also presented CRF, and a single patient with cirrhosis of the liver. A deterioration of renal function was observed in all the patients with DM and/or CRF, coinciding with the onset of APD. In patients with DM and/or CRF of diabetic origin, acute deterioration of renal function may be implicated in the onset of APD. Further studies are necessary to confirm this relationship.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information and that written informed consent for voluntary participation was obtained for all patients.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Lara L, Gómez-Bernal S, Vázquez-López F, Vivanco-Allende B. Dermatosis perforante adquirida: presentación de 8 casos. Actas Dermosifiliogr. 2014;105:e39–e43.