Acquired hyperpigmented facial macules were recently described in 25 children.1 This condition is characterized by the appearance of multiple, asymptomatic, hyperpigmented macular lesions on the forehead and in the temporal region with no segmental distribution and without the previous presence of erythema, edema, or desquamation. The mean age at presentation was 6 months (range, 2-24 months). The condition affected children of different races, and there was no history of similar lesions among family members or close contacts. We describe 3 new cases.
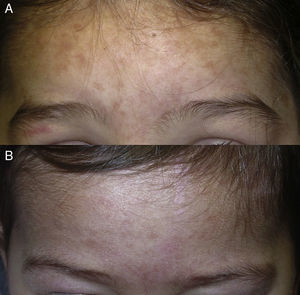
Case DescriptionsA 3-year-old girl with no past medical history of interest presented a number of asymptomatic hyperpigmented macules that had arisen spontaneously on the forehead and in the temporal region 4 months earlier (Fig. 1A). The lesions did not present desquamation, Darier sign was negative, and there was no history of inflammation in the affected area. The rest of the physical examination was normal. Her sister aged 2 years, diagnosed with atopic dermatitis, presented macules of similar characteristics in the same areas (Fig. 1B). Onset of the lesions occurred simultaneously in the 2 girls, during the winter months. Likely triggering factors were investigated but no relevant suspicious factors were detected. The other members of the family and closest contacts did not present any lesions. The adhesive tape test revealed no structures suggestive of a superficial mycosis, but remnants of pink-colored fibrillary structures were found on the surface of the adhesive tape; under polarized light, these fibers appeared synthetic (Fig. 2). At the 12-month follow-up the lesions persisted, but both girls presented a good general state of health, with no symptoms suggestive of systemic alterations.
The third patient was a 1-year-old girl of South American origin. She also presented asymptomatic hyperpigmented macules in the frontotemporal region. The macules had appeared during the first week of life and had remained clinically stable (Fig. 3). Immune studies including antinuclear antibodies and extractable nuclear antigen antibodies were performed on the girl and her mother and were negative.
Skin biopsy was not performed on any of the girls because of their age and the site and benign appearance of the lesions.
DiscussionHyperpigmented facial macules are a specific disease of unknown etiology and pathogenesis. Histology performed in some of the previously published cases showed postinflammatory changes. However, no trigger has been identified and the lesions cannot be attributed to other known causes of acquired hyperpigmentation in children.
The differential diagnosis to be considered during the initial evaluation of a patient with hyperpigmented macules includes a large group of disorders of very varied etiology, pathogenesis, and prognostic significance (Table 1). Postinflammatory pigmentation is the most common cause of transitory acquired hyperpigmentation in children. Pityriasis versicolor presents as hypo- or hyperpigmented macules with scaly desquamation; in children this disease can have a predominantly facial distribution.2 Direct observation of the fungus on microscopy confirms the diagnosis. Benign cephalic histiocytosis presents in infants as macules and papules that histologically show an infiltrate of histiocytes in the papillary dermis.3 The brownish lesions of urticaria pigmentosa typically present a positive Darier sign. The pigmented purpuric dermatoses are uncommon in children.4 Transient neonatal pustular melanosis, typical of black individuals, is characterized by transitory sterile pustules that rupture easily, even in utero, leaving hyperpigmented macules that disappear over the course of a few months. The so-called RASopathies (neurofibromatosis and Legius, Noonan, LEOPARD, cardiofaciocutaneous, and Costello syndromes) are a group of syndromes that share a mutation of the RAS/MAPK pathway and have some common cutaneous manifestations, such as pigmented lesions, and a frequent association with mental retardation, heart disorders, facial dysmorphism, and predisposition to develop cancer.5 Erythema dyschromicum perstans and idiopathic eruptive macular pigmentation, which some authors consider to be the same disease, are rare in children.6 Pigmented contact dermatitis, which presents as hyperpigmented macules with no previous eczematous phase, occurs mainly in dark skin phototypes, and a relationship with the use of dyes, cosmetics, fragrances, optical whiteners, and metals has been reported.7 Small children often have colognes applied to their hair, adults kiss them, leaving traces of lipstick on the forehead, or small adherent fibers from clothing can be left on their forehead on dressing or undressing, as was demonstrated in 2 of our patients. The young age of these patients makes it difficult to perform patch testing.
Differential Diagnosis of Facial Hyperpigmented Macules in Children.
| Condition | Distinctive Diagnostic Features | Facial Predominance |
|---|---|---|
| Postinflammatory pigmentation | History of previous lesions in the area | No |
| Pityriasis versicolor | Direct examination, adhesive tape test | Yes in children |
| Benign cephalic histiocytosis | Histology: Cells: CD68+, s100-, and CD1a- | Yes |
| Urticaria pigmentosa | Positive Darier sign | No |
| Pigmented purpuric dermatosis | Cayenne pepper spots | No |
| Transient neonatal pustular melanosis | Age at onset | No |
| RASopathies | Cardiac abnormalities, facial traits | No |
| Erythema dyschromicum perstans | Macules with a grayish color | No |
| Idiopathic eruptive macular pigmentation | Macules with a grayish color | No |
| Pigmented contact dermatitis | Patch testing | Yes |
In conclusion, we have described 3 new cases of the condition recently described by Hernández-Martín et al.; 2 of the cases were in sisters, rekindling the doubt over a possible common trigger or genetic predisposition.
Please cite this article as: Giacaman A, Knöpfel N, Campos M, Martín-Santiago A. Máculas hiperpigmentadas faciales adquiridas en la infancia: 3 nuevos casos. Actas Dermosifiliogr. 2016;107:83–85.