Acquired digital arteriovenous malformations (ADAVM) are uncommon acral vascular lesions most often affecting the finger. Treatment usually requires complete excision of the lesion with complex advancement flap or skin graft reconstruction. However, in recent years, some authors have reported satisfactory outcomes with laser treatment. We describe a series of 6 patients with ADAVM, 5 of whom received laser treatment and obtained a good response. The other patient was treated surgically. After an in-depth review of this type of lesion, we conclude that laser treatment is a safe and effective alternative for these malformations, provided the patients are appropriately diagnosed and have Schöbinger stage i lesions.
Las malformaciones arteriovenosas digitales adquiridas (MAVDA) son lesiones vasculares infrecuentes, habitualmente localizadas en zonas acrales, principalmente en los dedos de las manos. Su tratamiento a menudo requiere la extirpación completa de la lesión, requiriendo reconstrucciones complejas como colgajos o injertos. Sin embargo, en los últimos años se han comunicado algunos casos tratados satisfactoriamente con láser. Nosotros aportamos una serie de 6 pacientes con MAVDA, 5 de ellos tratados con láser con buena respuesta, y otro paciente tratado quirúrgicamente. En este trabajo hacemos una revisión exhaustiva de este tipo de lesiones y concluimos que la terapia láser es una alternativa terapéutica segura y efectiva para estas malformaciones, siempre y cuando los pacientes sean diagnosticados correctamente y se encuentren en estadio i de Schöbinger.
Acquired digital arteriovenous malformation (AVM) is a rare vascular anomaly that usually affects acral areas of the body, in particular the fingers. The lesions are complex and composed of multiple interconnected medium- or large-caliber arteries and veins lacking any intervening capillary bed. Although these lesions are not tumors, neither are they entirely benign since they can grow and invade adjacent tissue causing necrosis and bone resorption, inhibiting blood flow, and even leading to amputation of the affected region.
Although in most cases they appear spontaneously, these AVM have also been reported in association with trauma, inflammation, and surgery.1
Treatment of these lesions often requires complete excision followed by reconstruction with flaps or grafts. However, in recent years some authors have reported cases treated successfully with laser therapy.2 We present a series of 6 patients, 5 of whom were treated with laser therapy and 1 with surgery.
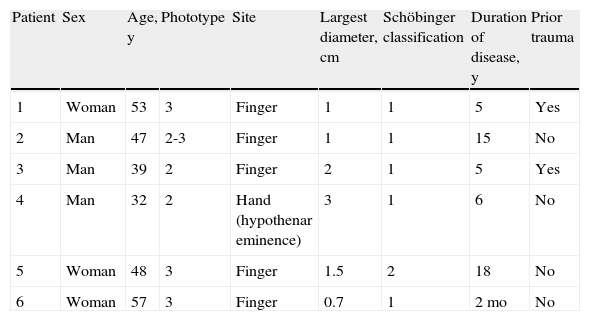
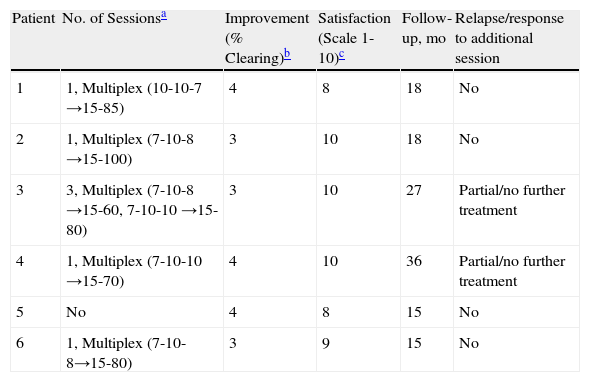
Case ReportPatients and MethodsWe present the cases of 6 patients who were referred to the dermatology department of Hospital Ramón y Cajal between 2010 and 2012. The patient characteristics are listed in Table 1.
Clinical Characteristics of the Patients.
| Patient | Sex | Age, y | Phototype | Site | Largest diameter, cm | Schöbinger classification | Duration of disease, y | Prior trauma |
| 1 | Woman | 53 | 3 | Finger | 1 | 1 | 5 | Yes |
| 2 | Man | 47 | 2-3 | Finger | 1 | 1 | 15 | No |
| 3 | Man | 39 | 2 | Finger | 2 | 1 | 5 | Yes |
| 4 | Man | 32 | 2 | Hand (hypothenar eminence) | 3 | 1 | 6 | No |
| 5 | Woman | 48 | 3 | Finger | 1.5 | 2 | 18 | No |
| 6 | Woman | 57 | 3 | Finger | 0.7 | 1 | 2 mo | No |
All the patients complained of severe bleeding after minor trauma, and 2 of them also reported intense pain that limited their daily activities.
On palpation, the lesions were firm and the temperature was raised locally. Only one patient presented a pulsatile lesion. Diascopy revealed incomplete emptying of the lesions, followed by rapid reengorgement. Physical examination revealed reticular arboriform erythematous-violaceous macular plaques with a longest diameter of between 1 and 3cm and a slightly keratotic surface. Dermoscopy revealed various vascular patterns: blue-red nodules, red ovoid patches, vascular dots, and tortuous vessels of diverse calibers radiating from a central nest.
Two of the patients provided samples from biopsies performed at other centers. Histologic study of these samples revealed a neoformation in the superficial dermis composed of thin-walled and thick-walled vascular structures lined with an endothelium without atypia and separated by loose connective tissue with a moderate number of cells.
The radiographs supplied by the patients were normal in all 6 cases, providing no evidence of bone involvement.
All the patients underwent a 20Mhz Doppler ultrasound study, which revealed well-defined hyperechoic lesions located in the superficial dermis. There was no evidence in any of the cases of involvement of adjacent tissue. Direct communications between large-caliber arteries and veins was observed. All the lesions had arterial and venous waveforms except for the pulsatile lesion in one patient, which was predominantly high-flow.
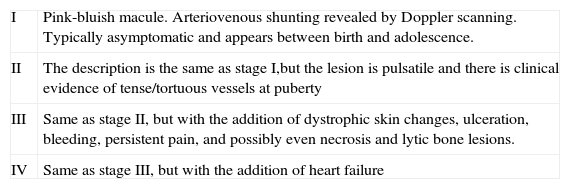
The lesions of 5 of these patients were stage i and in the sixth the pulsatile lesion was stage ii according to Schöbinger's classification of AVM (Table 2).
Schöbinger Classification.
| I | Pink-bluish macule. Arteriovenous shunting revealed by Doppler scanning. Typically asymptomatic and appears between birth and adolescence. |
| II | The description is the same as stage I,but the lesion is pulsatile and there is clinical evidence of tense/tortuous vessels at puberty |
| III | Same as stage II, but with the addition of dystrophic skin changes, ulceration, bleeding, persistent pain, and possibly even necrosis and lytic bone lesions. |
| IV | Same as stage III, but with the addition of heart failure |
On the basis of the clinical and exploratory findings we could reasonably rule out any involvement of bone or soft tissue and decided that further tests, for instance magnetic resonance imaging, were unnecessary.
ResultsThe patients with stage i lesions received laser treatment, which involved the application of pulsed dye laser at 595nm followed by long pulse Nd:YAG at 1064nm (Cynergy with Multiplex, Cynosure). A continuous flow of cold air was applied during treatment (Cryo5, Zimmer MedizinSystems GmbH) using the maximum level provided by the device.
The patient whose lesion was classified as stage ii was referred to another hospital for surgery. The stage ii lesion was complex and laser treatment would have entailed a high risk of bleeding and complications and the prospect of an acceptable response to laser treatment was poor. The stage iilesion was excised without significant complications and Doppler ultrasound follow-up a few months later showed no signs of recurrence.
Four of the patients treated with laser responded satisfactorily after 1 session (pain, bleeding, and functional limitation were reduced). In one case the lesion worsened after the first session and 2 more sessions were required to obtain optimal results.
The patients who received laser treatment were followed up for between 15 and 36 months after treatment. Three of them showed no signs of relapse; however, residual vessels were detected in the other 2 and confirmed by Doppler ultrasound in 1 patient. As the new lesions were asymptomatic it was decided that further laser treatment was not necessary, although these cases are being closely monitored.
Table 3 summarizes the doses used, the improvement and satisfaction achieved, and the duration of follow-up for each patient.
Results of Treatment.
| Patient | No. of Sessionsa | Improvement (% Clearing)b | Satisfaction (Scale 1-10)c | Follow-up, mo | Relapse/response to additional session |
| 1 | 1, Multiplex (10-10-7 →15-85) | 4 | 8 | 18 | No |
| 2 | 1, Multiplex (7-10-8 →15-100) | 3 | 10 | 18 | No |
| 3 | 3, Multiplex (7-10-8 →15-60, 7-10-10 →15-80) | 3 | 10 | 27 | Partial/no further treatment |
| 4 | 1, Multiplex (7-10-10 →15-70) | 4 | 10 | 36 | Partial/no further treatment |
| 5 | No | 4 | 8 | 15 | No |
| 6 | 1, Multiplex (7-10-8→15-80) | 3 | 9 | 15 | No |
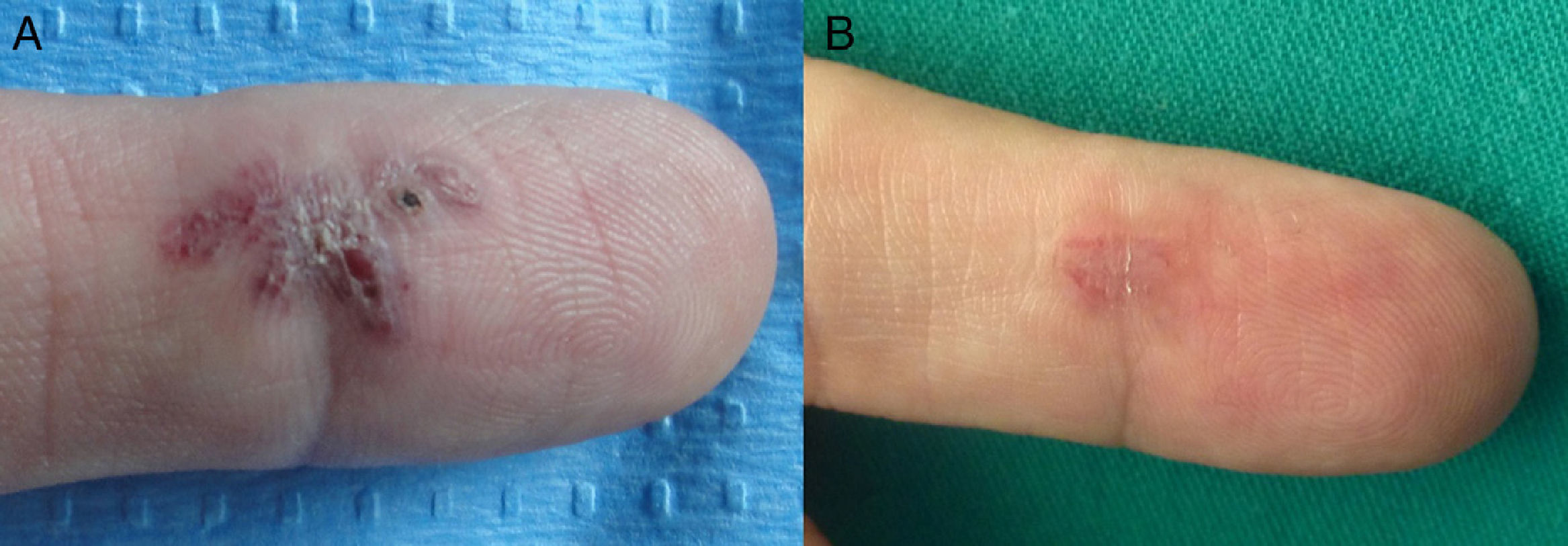
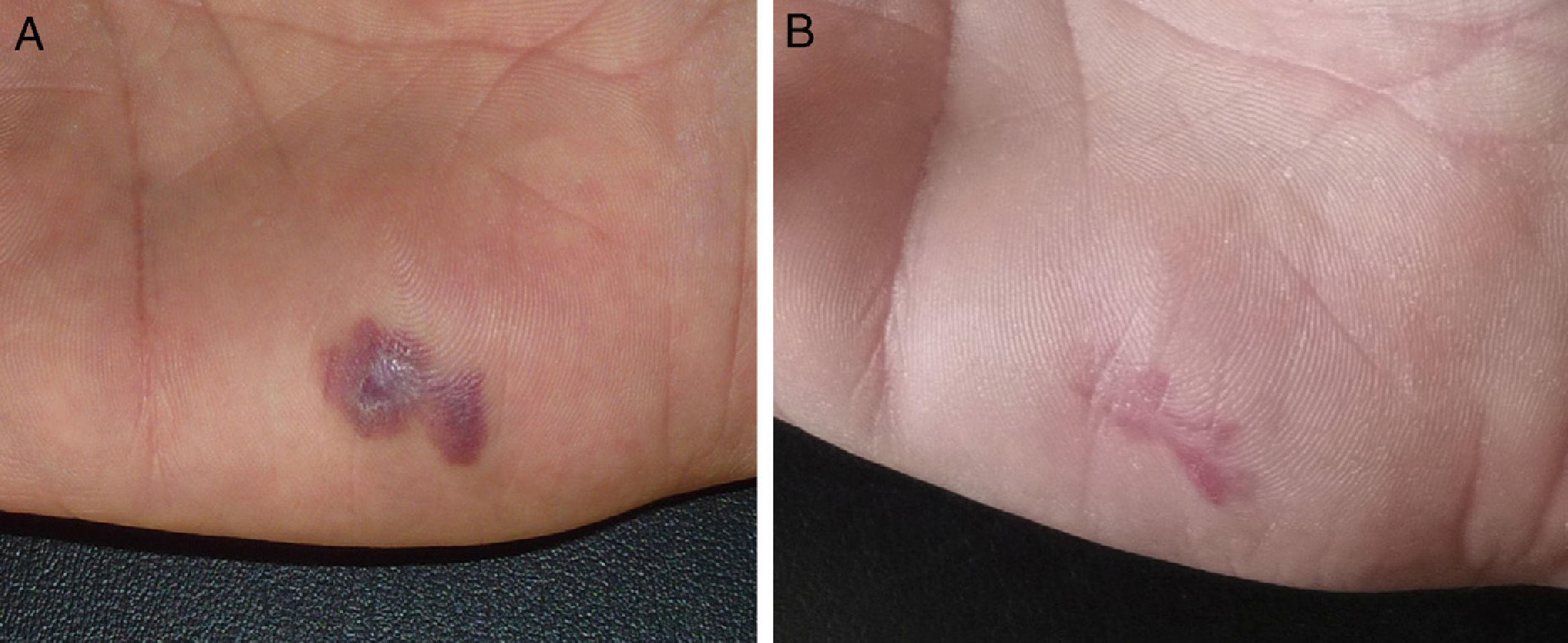
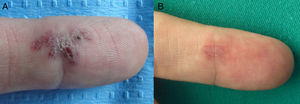
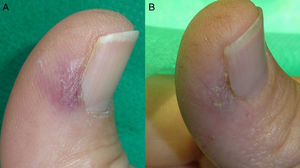
Figures 1–3 show some of the lesions before and after treatment.
A, Patient 3 had a bleeding and painful acquired digital arteriovenous malformation on the palmar surface of the 2nd finger of the right hand. B, Partial resolution after 3 treatment sessions. Recurrence of the vessels was observed on follow-up, but as the lesion remained asymptomatic, no more treatment was applied.
Acquired digital AVM are rare vascular anomalies.1–10
The term acquired digital AVM was first used in 1997 by McCulley,3 who reported the presence of a pulsatile purpuric mass on the finger of a pregnant woman. Histologic examination showed a vascular lesion with large-caliber arteries and veins and small endothelial spaces.3
The pathogenesis of these AVM is poorly understood. Even though no history of trauma is reported in most of the cases described in the literature, we partly share the view of Yang and O’Hara1 that the appearance of these lesions in acral zones suggests that the trigger may be small unnoticed traumas and that other factors must predispose certain patients to the development of these abnormal arteriovenous connections.
Although histologic examination may be useful, it is not indispensable and obtaining a sample for study may entail risks.4
Doppler ultrasound, however, should be used in all patients with a suspected AVM.4,5 This noninvasive technique can be used to delimit the lesion anatomically and to demonstrate the presence of arterial and venous flow. Ultrasound, clinical, and dermoscopic findings in conjunction with careful examination will provide sufficient evidence to make an accurate diagnosis. Although none of the authors in the literature we reviewed staged the lesions according to Schöbinger's classification for AVM, in our opinion staging is important in this setting because it influences both prognosis and choice of treatment.6,7
The differential diagnosis of these lesions should be primarily with glomus tumor (a very painful benign vascular tumor arising from glomus bodies and found primarily in acral sites) and pyogenic granuloma (a fast-growing vascular lesion that bleeds easily). In the cases presented here, both these possible diagnoses were reasonably ruled out by the duration of the lesions and the findings of explorations, in particular the presence of arterial and venous waveforms in the Doppler ultrasound.
We found surgery to be the treatment chosen by most authors.1,3,8–10 In 2007, Bekhor et al2 described the first 2 patients with acquired digital AVM treated with Nd:YAG laser and reported a reduction in the lesions of over 90%, which was sustained over the following months.
In the 6 cases reported here, we chose laser treatment for stage i lesions because they were in the embolization phase and surgery was not indicated. Moreover embolization in acral areas is not without complications because it can increase the risk of necrosis, and surgery in these areas requires very complex reconstructions that can affect the functionality of the digit.
We decided to treat the lesions using a Multiplex laser system because a more superficial laser, such as a pulsed dye laser, and insufficient doses would not treat the deepest part of the lesion and might, in fact, trigger progression of the malformation. Nd:YAG laser alone can be effective, as Bekhor et al. have shown, but high fluences are required for optimal results and these increase the risk of complications.2
With Multiplex laser it was possible to act on localized structures at different skin depths. The system emits pulsed dye laser with a penetration of 1mm that targets the more superficial structures followed by Nd:YAG with a penetration depth of 5 to 6mm. The pulsed dye laser converts oxyhemoglobin to methemoglobin, which increases absorption of the Nd:YAG laser, making possible the use of lower fluences, thereby reducing potential side effects such as necrosis and atrophic scars and, in the case of our patients, nail dystrophy. Although this is a novel laser system, it has already been shown to be effective in the management of resistant port wine stains,11 venous malformations,12 and residual infantile hemangiomas.13 The chief complications associated with laser treatment are, on the one hand, pain and bleeding during the application of treatment, and on the other, the possibility of leaving residual vessels that may trigger renewed growth of the lesion. If residual vessels are detected, the patient should be closely monitored, and a lesion that progresses should be treated by surgery or embolization.
For lesions classified as stage i using Schöbinger's criteria, laser treatment was shown to be a safe and effective alternative in this series. Tolerance was good and recurrence was low. However, accurate diagnosis and staging and correct selection of lesions is essential to avoid possible risks and complications.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their hospitals concerning the publication of patient data and that all patients included in this study were appropriately informed and gave their written informed consent.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Lapresta A, Hermosa E, Boixeda P, Carrillo-Gijón R. Malformaciones arteriovenosas digitales adquiridas. Una anomalía vascular infrecuente tratada con láser. Actas Dermosifiliogr. 2014;105:e33–e37.