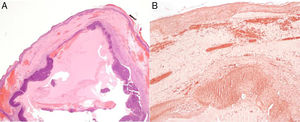
Pilomatrixoma or pilomatricoma is a relatively common benign cutaneous tumor that is derived from immature cells in the matrix of the hair follicle. It presents clinically as a slow-growing solid nodular lesion. There are 2 peaks in its incidence, the first during the first 20 years of life and the second smaller peak in individuals aged 50 to 60 years. In biopsy, the anetodermic or lymphangiectatic variant shows a decrease in collagen and elastic fibers as well as dilated lymphatic vessels in the superficial dermis. Clinically, these findings are manifest as hard palpable nodules within elastic sacs or as pseudobullous lesions.
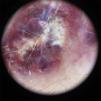
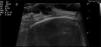
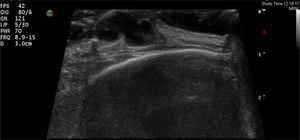
A 61-year-old woman, whose only relevant condition in her medical history was an operation for breast fibroadenoma, attended the clinic for a mildly painful, rapidly growing lesion in the right frontoparietal region, next to the hairline. The lesion had appeared 1 month earlier, a few days after trauma to the region. Physical exploration showed an exophytic lesion measuring 15mm across. This lesion was well defined and soft to the touch, of reddish and violaceous color with white-yellow patches (Figure 1). The dermatoscopic image showed a lesion with homogeneous red areas, irregular white-yellow structures, areas covered with a blue-white veil, irregular linear vessels, and some chrysalides (Figure 2). Skin ultrasound showed a hypoechoic, lobulated lesion in the superficial dermis, with discrete posterior reinforcement and increased perilesional vascularization (Figure 3). The lesion was completely excised under local anesthetic and sent for histopathological analysis, which confirmed the suspected diagnosis of anetodermic pilomatrixoma (Figure 4).
Anetodermic pilomatrixoma is an uncommon variant of a relatively common and well-known tumor. Its etiology is not clear, but recent studies postulate that mechanical trauma could play an essential role in its development by compromising the dermal integrity and altering the vascular microenvironment.1 Some authors have suggested that the trigger could be an increase in the number or activity of mast cells, which would favor elastolysis and increase epidermal proliferation of the lesion through the activation of certain cytokines.2 This would also explain why some of these tumors exhibit hyperpigmentation in the basal layer due to the capacity of mast cells to activate melanocyte proliferation through certain mediators.
Clinically, anetodermic pilomatrixoma presents as an excrescent tumor with a predilection for the skin of the arms and shoulders, with normal skin coloration, a hyperpigmented appearance, or a vascular appearance.3 The lesions are soft on palpation and can be depressed at the center when vertical pressure is applied.
If we compare the dermatoscopic characteristics of our lesion with those reported for nonanetodermic pilomatrixomas in the study by Zaballos et al.,4 we find that irregular white structures, homogeneous red areas, and irregular linear vessels are common features. The dilated vessels and hemorrhages observed in pathology may correspond to the linear vessels and homogeneous reddish areas present in the dermatoscopic image.
The ultrasound image of conventional pilomatrixoma shows a lesion with a hypoechoic halo and a central hyperechoic region (corresponding to calcification) that generates the posterior shadow.5 In 1999, Hughes et al.6 published a retrospective preoperative ultrasound study of 28 suspected conventional pilomatrixomas. In 20 of these, the ultrasound findings supported the suspected clinical diagnosis and in 16 of these 20 lesions, histological study confirmed diagnosis of pilomatrixoma. In the literature that we reviewed, we could not find a description of skin ultrasound of anetodermic pilomatrixoma.
Differential diagnosis should include basal cell carcinoma (BCC) and melanoma,4 and in both cases, the dermatoscopic and ultrasound studies can help in the preoperative diagnosis. From the ultrasound point of view, BCC and melanoma are also considered hypoechoic lesions. The characteristics that can help differentiate these lesions from pilomatroxima are the presence of small hyperechoic nodules in the lesion characteristic of BCC and an irregular border with abundant vascularization within the tumor in characteristic melanoma lesions.7,8
In conclusion, we present the clinical description and the first dermatoscopic and ultrasound findings for anetodermic pilomatrixoma.
Please cite this article as: Martínez-Morán C, Echeverría-García B, Nájera L, Borbujo J. Un tumor en imágenes: pilomatrixoma anetodérmico. Actas Dermosifiliogr. 2015;106:241–243.