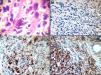
An 86-year-old man with an inconspicuous medical history was seen at the Dermatology Department of the Instituto de Investigaciones Médicas “A. Lanari” in April 2015, due to an infiltrated reddish plaque of hard elastic consistency localized in the scalp margin in the frontal region. This plaque had appeared 4 months before, and the patient was asymptomatic (Fig. 1). He also had severe actinic damage evidenced by multiple actinic keratoses in his face, mainly in the forehead, temples and nose. He had been prescribed several courses of 5 fluorouracil cream to be applied at night for a month.
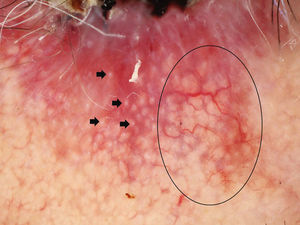
The dermoscopy showed arborizing vessels, reddish and whitish structureless areas and shiny white linear structures (Fig. 2). Based on the clinical analysis and dermatoscopy, a biopsy was performed.
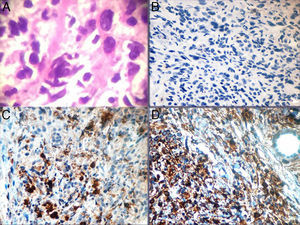
Examination of the histological sections (H&E) revealed proliferation of cells with abundant cytoplasm, some multinucleated and others with bizarre nuclei, showing marked pleomorphism. Tapered cells coexist, and stroma presented myxoid changes. Immunohistochemistry showed positive staining for CD68 and vimentin and negative staining for cytokeratins (AE1–AE3), smooth muscle actin and S100 protein (Fig. 3).
What is your diagnosis?
DiagnosisA plaque-like variant of an atypical fibroxanthoma.
ConclusionAtypical fibroxanthoma (AFX) is a rare mesenchymal tumor considered a superficial variant of undifferentiated pleomorphic sarcoma. It exhibits locally aggressive behavior, and a tendency to recur after surgery. Metastasis rates are low. The plaque-like variant is a very rare morphological variety, not usually diagnosed clinically.1,2
FXA has preferential location in sun-exposed areas in elderly patients, so it is believed that ultraviolet radiation plays an important role in its pathogenesis. Our patient matches the description as he is 86 years old and has photodamaged skin marked by multiple actinic keratoses.
The plaque-like variant is a very rare morphological variety, not usually diagnosed clinically. Dermatoscopy is a useful tool in these cases; publications about the dermoscopy of an atypical fibroxanthoma in the literature are scarce. The following dermoscopic findings has been described: (1) atypical vascular pattern with irregularly distributed polymorphic vessels: linear (tortuous and arborizing), dotted and globular, (2) shiny white structures (linear, white areas or rosettes), (3) heterogeneous hyperpigmentation, and (4) rainbow pattern.3
Although the most consistent finding is the atypical vascular pattern, as in the case of our patient, it is unspecific because it can be seen in other clinically similar tumors exhibiting chaotic neoangiogenesis during growth. However, it is important to emphasize that its detection should raise suspicion of malignancy, and complete surgical excision of the lesion should be performed, as we did with our patient who was referred to the Surgery Department for a complete removal of the lesion.4
AFX should be included in the list of differential diagnoses of reddish malignant cutaneous tumors such as squamous cell carcinoma, basal cell carcinoma, Merkel cell carcinoma, amelanotic/hypomelanotic melanoma and eccrine poroma.5
Conflicts of interestThe authors declare that they have no conflicts of interest