The risk of developing bacteremia and sepsis in patients with erythroderma has not been extensively studied. The most frequent foci of bacteremia in adults and elderly patients are the urinary, biliary, and respiratory. The cutaneous origin should be considered in the case of extensive cutaneous disease.
In elderly and immunosuppressed patients, bacteremia can go unnoticed until it causes the involvement of some other organs or tissues. Soft tissue infection, such as an abscess in the hip musculature, is a possible complication.
Psoas abscess is an uncommon but life-threatening condition, especially due to frequent delays in diagnosis. Symptoms are not specific: Hip, back, thigh, or abdominal pain and, occasionally, fever. Early diagnosis and treatment are key to preventing complications such as septic shock and death.
Psoas abscess can be classified as primary when it is due to hematogenous or lymphatic spread, or secondary when it is caused by contiguous infection. Primary abscesses are more frequent in children, developing countries, and immunocompromised patients. Risk factors include trauma, osteoarthritis, diabetes, HIV infection, intravenous drug user, renal failure, and immunosuppressives. Staphylococcus aureus (SA) is the most common agent in primary abscesses (42.9%), followed by Streptococcus viridans (19%).1
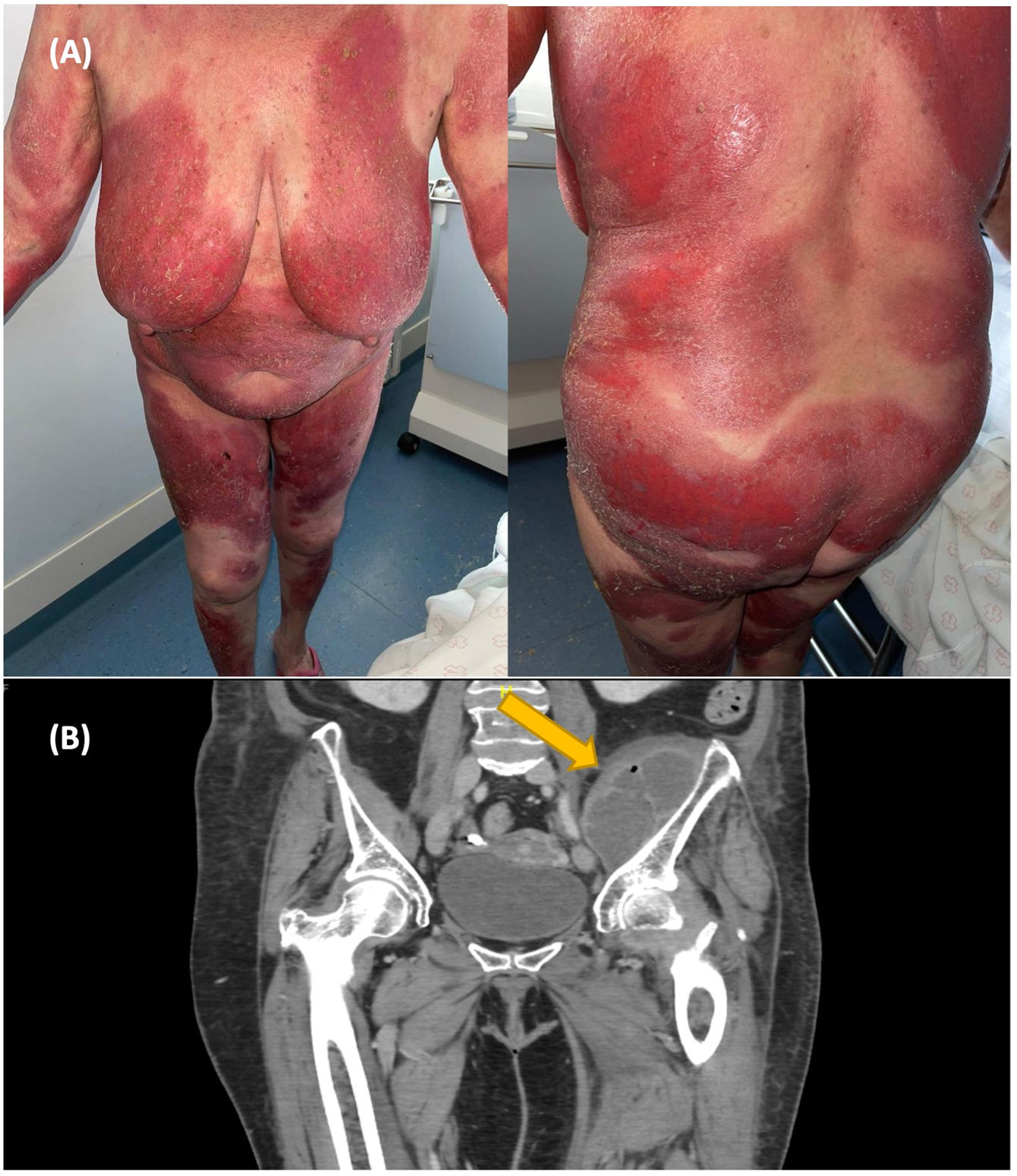
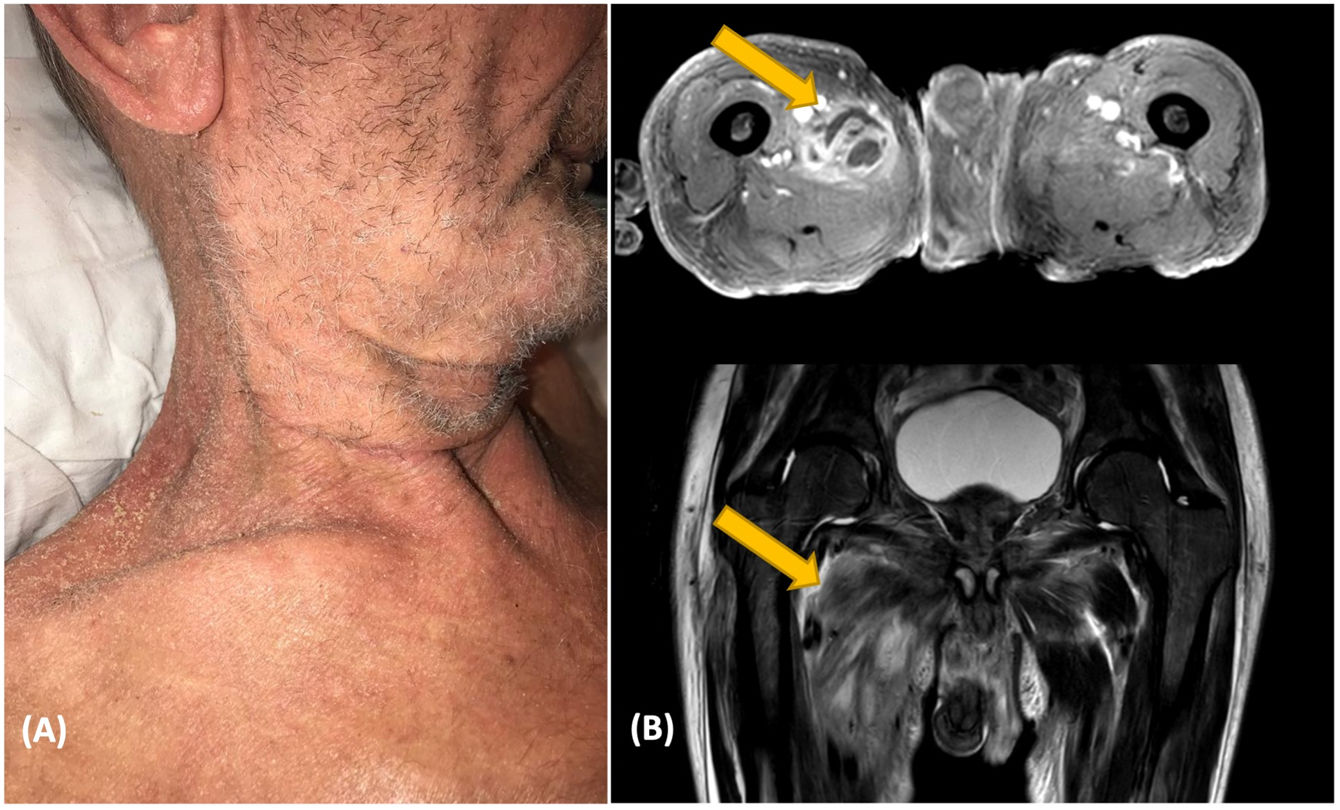
We report the case of two patients with erythroderma and hip abscess. Patient 1 was a 70-year-old woman who presented persistent psoriatic erythroderma despite treatment with etretinate, methotrexate, and cyclosporine (Fig. 1A). She was admitted to the hospital in March 2021 with a Psoriasis Area and Severity Index (PASI) of 41, and a body surface area (BSA) of 58. The psoriatic plaques were highly inflammatory with broken pustules on their surface, but without clear foci of erosions. One month later, she reported left thigh pain. No abnormalities were detected by X-ray and ultrasonography. Within one week, she developed chills and a fever. Blood cultures were positive for methicillin-sensitive SA (MSSA). With the suspicion of an infectious complication in the hip, MRI was requested, revealing a pus collection into the iliac muscle.
Patient 2 was a 76-year-old man who had a 2-year history of eczema outbreaks. He was admitted to the hospital after developing erythroderma with lymphadenopathy (Fig. 1B). A skin biopsy confirmed the clinical suspicion of mycosis fungoides. The complementary tests did not show clonality in peripheral blood or lymph nodes, so the diagnosis of mycosis fungoides stage IIIa (T4N1aM0B0) was established. Over the following days, the patient developed malaise, fever, and hip pain. Blood cultures were positive for MSSA and Streptococcus pyogenes. Body CT showed an iliac abscess. Endocarditis was discarded as the patient had a mechanical heart valve (Fig. 2).
There is little written in the literature about the risk of bacteremia and infectious complications in patients with extensive chronic dermatoses. A large Indian retrospective study evaluated the etiology and frequency of sepsis in patients admitted to the dermatology unit2. Among 860 patients, 4.65% developed sepsis. Within these cases, vesiculobullous diseases were the most frequent diagnosis (42.5%), followed by erythroderma (25%). Methicillin-resistant SA (MRSA) was the most common organism, but also MSSA was isolated in 8.7% of the patients.
Erythroderma may be a portal of entry to bacteremia as it involves an epidermal barrier dysfunction. Also, high-dose steroids and immunosuppressives are typically used in these patients, which favor infections and might cover up symptoms. Routier et al.3 describe 2 patients with psoas abscesses caused by streptococcal infection with a cutaneous portal of entry.
On the other hand, psoriatic erythroderma may be triggered by infections. Green et al.4 report 5 patients with erythrodermic psoriasis and hidden SA bacteremia. Skin manifestations only got better when the infection was controlled. Although it is unusual, bacteremia might have come from a primary abscess exacerbating skin lesions secondarily.
SA colonization has been associated with increased BSA involvement in psoriasis5 and cutaneous T-cell lymphoma (CTCL)6. CTCL patients frequently present bacterial infections, particularly SA. Staphylococcal decolonization often results in clinically significant improvements7.
The reason why abscesses in the iliopsoas are formed is not clear. A lower limb or perineal wound could explain the predisposition for an abscess to appear in that area. It is also a well-vascularized region where microorganisms could seed. In addition, elderly patients may suffer from osteoarthritis or trauma, which predisposes them to infection.
The diagnosis is based on clinical symptoms and imaging tests. CT and MRI are the gold standards, but in the early stages, they can present false negatives8. That is why it is important to have this diagnosis in mind and repeat imaging tests if necessary.
Treatment consists of broad-spectrum antibiotics and abscess drainage. Surgical drainage is the traditional treatment, but image-guided percutaneous drainage is an effective alternative.
In short, erythroderma involves an epidermal barrier dysfunction that predisposes to infection and bacteremia. Primary psoas abscess probably occurs as a consequence of hematogenous seeding. Therefore, erythroderma should be considered a risk factor.
A high degree of suspicion is needed for an early diagnosis: Thigh, hip, or back pain and bacteremia in an erythrodermic patient are mandatory to discard an iliopsoas abscess.
Conflict of interestsThe authors declare they have no conflicts of interest
Mariana Campayo Paños.