Basaloid follicular hamartoma (BFH) is an uncommon benign neoplasm that may be familial or acquired, generalized or localized. Because the malignant transformation of this tumor to basal cell carcinoma has been reported, it is considered a premalignant lesion.1
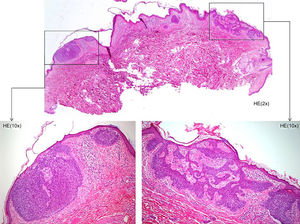
The characteristic histologic features of BFH are the proliferation of strands of basaloid epithelial cells that originate in the infundibular portion of hair follicles, branch outward, and are surrounded by a loose fibrous stroma. There is usually a clear transition between tumor cells and the adjacent stroma. The tumor cells do not usually display pleomorphism, nuclear atypia, or mitotic activity.2
BFH treatments include surgical excision, cryotherapy, laser therapy, topical imiquimod or retinoids, and photodynamic therapy.3,4 In case of malignant transformation to basal cell carcinoma, surgical removal is the treatment of choice because it has the lowest recurrence and complication rates.
We report the case of a 60-year-old woman who complained of a pruritic lesion on her chest that had grown in recent months. She also reported having had many small lesions on the right side of her chest, pubic area and groin since the age of 30 years, although she never sought care because they were stable and asymptomatic. She did not report hair loss, ptosis, difficulty swallowing, or any other systemic symptoms, and she could not recall similar complaints in relatives. A physical examination revealed multiple skin-colored erythematous papules on the right side of her chest, right breast, pubic area, and groin. The lesions followed Blaschko lines, and some were comedones measuring less than 1cm in diameter (Fig. 1). Above the right breast was an erythematous plaque measuring 1cm. The surface was pearly and dermoscopy revealed telangiectases and blue-gray globules.
A biopsy of the supramammary plaque showed nests of basaloid cells that originated in the epidermal basement membrane; they were separated by fragments of healthy epidermis. The periphery was pale, and mitotic figures and apoptotic bodies were numerous. The lesion also contained areas where basaloid cells proliferated, arranged in strands with pilar differentiation, low mitotic activity, and a loose fibroblastic stroma (Fig. 2).
A diagnosis of basal cell carcinoma arising in a BFH was based on the clinical history, physical examination, and biopsy.
This type of acquired, segmental, unilateral BFH can appear at birth or develop in adolescence. Unlike generalized familial forms, this phenotype is not associated with hypotrichosis, cystic fibrosis, or other autoimmune diseases such as myasthenia gravis or systemic lupus erythematosus.5
A diagnosis of BFH does not require laboratory tests or imaging. However, a complete medical history and physical examination is essential even though associations between localized BFH and systemic diseases have not been reported. If there is clinical suspicion of autoimmune disease, antinuclear antibody and antiacetylcholine receptor tests should be ordered in addition to any other tests the patient's symptoms suggest.
The main differential diagnoses are infundibulocystic basal cell carcinoma (IBCC)2 and trichoepithelioma,5 which are also hair follicle tumors. BFH tends to center around the follicle and involve the interfollicular dermis less than IBCC. Deep infiltration, epidermal ulceration, and rapid growth would suggest IBCC. Some authors nevertheless consider BFH and IBCC to be the same diagnosis because their morphology is so similar and both express cytokeratin 20.6
Trichoepithelioma can be distinguished from BFH by the greater stromal cellularity of the former. In addition, a trichoepithelioma shows fissures caused by retraction as the tumor stroma separates from the adjacent dermis.
Because of the coincidence of unilateral BFH and basal cell carcinoma lesions distributed along Blaschko lines in this case, segmental Gorlin syndrome had to be considered in the differential diagnosis.7 However, such a diagnosis was unlikely because of the absence of a family history of this syndrome or characteristic signs such as the presence of basal cell carcinoma from an early age, keratocystic odontogenic tumors in the maxilla, palmoplantar pitting, or developmental skeletal abnormalities. The unilateral distribution along Blaschko lines could be owing to the presence of a somatic mutation early in embryonic development.
Although detection of a mutation in the patched 1 gene (PTCH1) in healthy or affected skin,8 or in peripheral blood lymphocytes, would have been useful for distinguishing BFH from segmental Gorlin syndrome in our patient, this gene test was unavailable in our hospital.
In conclusion, although BFH is a very rare benign neoplasm, diagnosis is important so that periodic follow-up can be scheduled in the interest of early detection of basal cell carcinoma. BFH lesions can develop morphologic changes or grow and should be biopsied.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Requena López S, Maldonado Seral C, Vivanco Allende B. Pápulas múltiples con distribución unilateral y segmentaria en mujer de 65 años. Actas Dermosifiliogr. 2018;109:190–192.