Hand eczema is not uncommon in children but it is rarely studied using skin-prick tests. Few reports have addressed their usefulness in children and none has specifically analyzed their use in children with hand eczema.
Material and methodsWe performed a retrospective study of all children up to 16years of age with hand eczema who were assessed in the Department of Dermatology at Hospital General Universitario in Alicante, Spain with the standard GEIDAC panel over a 5-year period. We compared the epidemiologic data and results of skin-prick tests in this group with those obtained in children with eczema at any site and in adults with hand eczema.
ResultsThe study included a total of 1695 patients: 141 (8.3%) children and 1533 (91.7%) adults. Hand eczema was diagnosed in 496 (31.9%) adults and 32 (22.7%) children. Positive results were obtained in skin-prick tests in 50% of children with hand eczema compared with 37.6% of children with eczema at any site and 50.6% of adults with hand eczema. The current relevance of the positive allergens found in children with hand eczema (76.2%) was greater than that observed in children with eczema at any site (61%) or in adults with hand eczema (43%). The most common allergens in children with hand eczema were kathon CG and fragrance mix I, whereas in the other 2 groups metals were the most common. The most common final diagnosis in children with hand eczema was allergic contact dermatitis (34.3%), which proved to be more common than atopic dermatitis.
ConclusionsWe recommend the use of skin-prick tests in all children with chronic hand eczema.
El eczema de manos en la edad infantil no es infrecuente, pero raramente es estudiado mediante pruebas epicutáneas. Existen pocos trabajos que estudien la utilidad de las mismas en los niños, pero no existe ninguno que aborde su utilidad en el eczema de manos en la población infantil.
Material y métodosRealizamos un estudio retrospectivo con todos los niños (0-16 años) con eczema de manos estudiados en la Sección de Dermatología del Hospital General Universitario de Alicante con la batería estándar del GEIDAC durante los últimos 5 años. Comparamos los datos epidemiológicos y los resultados de las pruebas epicutáneas de este grupo con los obtenidos en la población infantil con eczema de cualquier localización y en los adultos con eczema de manos.
ResultadosEstudiamos 1.695 pacientes, 141 (8,3%) niños y 1.553 (91,7%) adultos. 496/1.553 (31,9%) adultos y 32/141 (22,7%) niños presentaban eczema de manos. El 50% de los niños con eczema de manos, frente al 37,6% de los niños con eczema y el 50,6% de los adultos con eczema de manos presentaron algún alérgeno positivo en las pruebas epicutáneas. La relevancia presente de los alérgenos positivos encontrados en los niños con eczema de manos (76,2%) fue mayor que las obtenidas en los niños con eczema (61%) y los adultos con eczema de manos (43%). Los alérgenos más frecuentes en los niños con eczema de manos fueron el kathon CG y la mezcla de fragancias I, mientras que en los otros dos grupos fueron los metales. El diagnóstico final más frecuente en niños con eczema de manos fue el eczema de contacto alérgico (34,3%) por delante de la dermatitis atópica.
ConclusiónRecomendamos la realización de pruebas epicutáneas a todo niño con eczema crónico de manos.
Hand eczema is a common skin disease and one of the most frequent presenting complaints in contact allergy units. Prevalence in the general population ranges from 2.0% to 8.9%,1–3 and approximately 20.0% to 30.0% of all cases are thought to affect the hands.4–6 The etiology of hand eczema is multifactorial and includes exposure to external agents-both irritants and allergens-and endogenous factors, such as atopic dermatitis and other skin diseases involving skin barrier abnormalities.7 Contact dermatitis (both allergic and irritant) is the most common diagnosis in patients with hand eczema.8 Patch testing is highly recommended in cases of chronic eczema. The frequency of positive patch test results in patients with hand eczema is approximately 59%.9
Allergic contact dermatitis is considered an uncommon finding in children, and eczema is generally considered to be due to endogenous factors, such as atopic dermatitis, or irritants such as soap and clothing.10–13 The low incidence of allergic contact dermatitis was believed to be due to reduced exposure to allergens13 and to an immature immune system leaving children less susceptible to sensitization.12 During the last decade, several articles from various European countries have confirmed that not only does allergic contact dermatitis occur in children, but that it is also relatively common.13 However, no studies have addressed the usefulness of patch testing in children with chronic hand eczema.
The main objectives of the present study were as follows:
- 1.
To perform an epidemiologic study of children with hand eczema.
- 2.
To evaluate the results of patch tests in children with eczema in order to prove their usefulness.
- 3.
To compare the results in this population with those obtained for other children studied and in adults with hand eczema who have also undergone patch tests.
We performed a retrospective study in the Skin Allergy Clinic of the Department of Dermatology at Hospital Universitario de Alicante in Alicante, Spain. Our health district covers approximately 275 000 inhabitants, of whom 18.79% are children aged up to 16 years. Our catchment area serves mainly the tourist and service sectors and has no noteworthy industrial base. The study period was from January 2004 to December 2009.
Study populationThe study population comprised all children aged up to 16 years with hand eczema who were tested using the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC)14 during the study period; a subanalysis of patients with a positive result was also performed.
Data were obtained from an electronic database that records patient data and the test series applied, as well as the results and their relevance. The clinical data recorded for each patient were history number, age, sex, personal and family history of atopy, occupation, location of the lesions, allergen series tested, number of positive results, type and relevance of the positive results, source of sensitization, and diagnosis.
TerminologyHand eczemaOur criterion for defining hand eczema was appearance of eczema on the palm of the hand, dorsum of the hand, sides of the fingers, finger pads, or on the hand and other sites that had appeared once and lasted at least 2 weeks, had appeared on several occasions, or was persistent. Eczema affecting 2 different parts of the hand was considered diffuse disease.
AtopyA history of allergic rhinitis or allergic asthma was considered personal atopy, familial atopy, or both. We differentiated the variable atopy according to 4 possibilities: patients with a personal history of atopy, patients with a family history of atopy, patients with a personal history of atopic dermatitis, and patients with no personal or family history of atopy.
Age groups (children)The 141 children who underwent patch testing were divided into 3 age groups: up to 5 years, 6 to 10 years, and 11 to 16 years.
MOALFHA indexThe MOALFHA index was used to study patient characteristics. This index scores the following characteristics: male sex, occupational dermatitis, atopic dermatitis, leg dermatitis, face dermatitis, hand dermatitis, and age >40 years.15
Patch testing methodThe allergens used in the GEIDAC standard series were supplied by Chemotechnique Diagnostics (Malmö, Sweden). The standard series applied in our department also includes palladium chloride and methyldibromo glutaronitrile. The patches were prepared using Finn Chamber adhesive strips (Epitest, Oy, Tuusala, Finland) that were fixed with Scampor adhesive (Norgeplaster A/S, Kristiandsand, Norway) and removed after 48hours’ contact with the skin. Test results were read at 48 and 96hours, according to the criteria of the International Contact Dermatitis Research Group (ie, +, ++, +++). When results were doubtful, a late reading was taken at 7 days. Relevance was considered present if symptoms could be totally or partially attributed to the allergen obtained, past if a positive result only referred to previous eczema, and unknown if symptoms could not be attributed to the allergen obtained.
Statistical analysisData were processed using SPSS 15.0 (SPSS Inc, Chicago, Illinois, USA). Qualitative variables were analyzed using the χ2 test. When the conditions for application of the χ2 test were not met, we used the Fisher exact test. Statistical significance was set at P≤.05. A tendency toward statistical significance was set at P≤.1. The results were analyzed and interpreted and compared with those from similar studies.
ResultsBetween January 2004 and December 2009, we performed patch tests with the standard GEIDAC series on 1694 patients, of whom 1553 (91.7%) were adults and 141 (8.3%) were children. Hand eczema was observed in 496 adults and 32 children (Tables 1 and 2). Children younger than 16 years accounted for 6% (32/528) of all the cases of hand eczema studied.
Comparison Between the Pediatric Population With Eczema at Any Site and Children With Hand Eczema.a
| Eczema in the Pediatric Population | Hand Eczema in Children | P Value | |
| Number of patients | 141 | 32 | |
| Boys | 62 (44.0%) | 15 (46.9%) | P=.8 |
| Girls | 79 (56.0%) | 17 (53.1%) | P=.8 |
| Personal history of atopy | 21/70 (30.0%) | 3/28 (10.7%) | P=.04b |
| Personal history of atopic dermatitis | 20/70 (28.6%) | 11/28 (39.3%) | P=.3 |
| Family history of atopy | 24/70 (34.3%) | 9/28 (32.1%) | P=.8 |
| No personal or family history of atopy | 27/70 (38.6%) | 12/28 (42.8%) | P=.7 |
| Number of patients by age group | |||
| 0.5 y | 24 (17.0%) | 6 (18.7%) | P=.8 |
| 6-10 y | 47 (33.3%) | 8 (25.0%) | P=.4 |
| 11-16 y | 70 (49.7%) | 18 (56.3%) | P=.5 |
| Positive patch test result | 53 (37.6%) | 16 (50%) | P=.2 |
| Boys | 24 (38.7%) | 7 (46.7%) | P=.9 |
| Girls | 29 (36.7%) | 9 (53.0%) | P=.9 |
| Positive patch test result | |||
| 0.5 y | 6 (25%) | 3 (50%) | P=.4 |
| 6-10 y | 19 (40.4%) | 4 (50%) | P=.4 |
| 11-16 y | 28 (40%) | 9 (50%) | P=.8 |
| Patients with a history of allergic dermatitis | 20 | 11 | |
| Patch test (+) | 4 (20%) | 5 (45.5%) | P=.14 |
| Patch test (−) | 16 (80%) | 6 (54.5%) | |
| Most common site, % | Hands, 22.7% | Palms, 40.6% | |
| Most common diagnoses, % | Atopic dermatitis, 32.6% | Allergic contact dermatitis, 34.3% | |
| Most common cause, No. | Clothing, 19 | Cosmetics, 9 | |
| Most common allergen, No. | Thiomersal, 17 | Methylchloroisothiazolinone, 5 | |
| Relevance | |||
| Present | 78 (61%) | 32 (76.2%) | P=.07c |
| Past | 14 (11%) | 2 (4.7%) | P=.2 |
| Unknown | 36 (28%) | 8 (19.1%) | P=.2 |
Comparison Between Children With Hand Eczema and Adults With Hand Eczema.a
| Hand Eczema in Children | Hand Eczema in Adults | P Value | |
| Number of patients | 32 (22.7%) | 496 (31.9%) | P=.7 |
| Male | 15 (46.9%) | 214 (43.1%) | |
| Female | 17 (53.1%) | 282 (56.9%) | |
| Personal history of atopy | 3/28 (10.7%) | 26/161(16.1%) | P=.5 |
| Personal history of allergic dermatitis | 11/28 (39.3%) | 10/161 (6.2%) | P<.001b |
| Family history of atopy | 9/28 (32.1%) | 34/161 (21.1%) | P=.2 |
| No personal or family history or atopy | 12/28 (42.8%) | 103/161(64%) | P=.03b |
| Positive patch test result | 16 (50%) | 251 (50.6%) | P=.9 |
| Boys/Men | 7 (46.7%) | 90 (42%) | P=.5 |
| Girls/Women | 9 (53%) | 161(67.7%) | P=.5 |
| Patients with a history of atopic dermatitis | 11 | 10 | |
| Patch test (+) | 5 (45.5%) | 3 (30%) | P=.4 |
| Patch test (−) | 6 (54.5%) | 7 (70%) | |
| Most common site, % | Palms (40.6%) | Diffuse (25.6%) | |
| Most common diagnosis, % | Allergic contact dermatitis (34.3%) | Irritant contact dermatitis (38.9%) | |
| Most common cause, No. | Cosmetics, 9 | Occupational | |
| Most common allergen, No. | Methylchloroisothiazolinone, 5 | Nickel sulfate, 136 | |
| Relevance | |||
| Present | 32 (76.2%) | 263 (43%) | P<.001b |
| Past | 2 (4.7%) | 202 (33%) | P<.001b |
| Unknown | 8 (19.1%) | 145 (24%) | P=.5 |
Of the 141 children studied, 62 were boys and 79 girls.
Table 1 shows the distribution by age group. We recorded a history of atopy in 70 children (Tables 1 and 2).
The distribution of eczema was as follows: hands, 32 (22.7%) patients; generalized, 30; trunk, 11; feet, 11; dorsum of the feet, 10; legs, 9; face, 8; eyelids, 5; and other, 25.
Analysis by age group revealed that, in children aged up to 5 years and 11-16 years, the most common site was the hands (37.5% and 24.3%, respectively), whereas in those aged 6-10 years, the most common site was the feet (25.5%). Table 3 shows the demographic characteristics of the study populations according to the MOALFHA index. We found a higher percentage of male patients with hand eczema in the pediatric population than in the total population (46.9% and 37.5%; P=.28).
Demographic Characteristics of the Study Populations According to the MOALFHA Index.
| Total Study Population | Pediatric Population With Hand Eczema | Pediatric Population With Eczema in General | Adults With Hand Eczema | ||||||
| Total | Percentage | Total | Percentage | Total | Percentage | Total | Percentage | ||
| Patients studied | 1694 | 100 | 32 | 1.9 | 141 | 8.3 | 496 | 29.3 | |
| M | Male sex | 636 | 37.5 | 15 | 46.9 | 62 | 44 | 214 | 43.1 |
| O | Occupational dermatitis | 230 | 13.6 | 1 | 3.1 | 2 | 1.4 | 173 | 34.9 |
| A | Atopic dermatitis | NR | NR | 11/28 | 39.3 | 20/70 | 28.6 | 10/161 | 6.2 |
| L | Leg dermatitis | 212 | 12.5 | - | - | 30 | 21.3 | - | - |
| F | Face dermatitis | 268 | 15.8 | - | - | 8 | 5.7 | - | - |
| H | Hand dermatitis | 528 | 31.2 | 32 | 100 | 32 | 22.7 | 496 | 100 |
| A | Age >40 | 982 | 58 | - | - | - | - | 265 | 53.2 |
Abbreviation: NR, not recorded for all the patients in our database.
Of note, occupational dermatitis was more prevalent in adults with hand eczema than in the general population (34.9% and 13.6%; P<.001).
The most common site of eczema in the total study population and in the pediatric population was the hands (31.2% and 22.7%, respectively; P=.03), although we observed more children with eczema on the legs (21.3% vs 12.5%; P=.003) and fewer with eczema on the face (5.7% vs. 15.8%, respectively; P=.001) compared with the total population that underwent patch testing.
Frequency in the pediatric population with hand eczemaThe median age of children with hand eczema was 12 years.
We did not perform patch testing on any patient aged less than 2 years. The group contained 15 boys and 17 girls. Table 1 shows the distribution by age group.
We recorded a history of atopy in 28/32 children with hand eczema (Table 1). The most common site was the palms, which were affected in 13 (40.6%) patients, followed by the sides of the fingers in 6 patients, finger pads in 4 patients, dorsum of the hand in 1 patient, hands and eyelids in 2 patients, hands and forearms in 1 patient, and soles and palms in 2 patients. Diffuse eczema on the hands was observed in 2 patients and diffuse involvement of the hands and feet in 1 patient (Tables 4 and 5). Eczema was present at sites other than the hands in 6 of the 32 patients.
Characteristics of Children With Hand Eczema and Positive Patch Test Results.
| Patient No. | Sex, age, y | History of Atopy | Location | Cause | Series Tested | No. of Positive Results | Allergens and Relevance | Diagnosis |
| 1 | Female, 2 | No | Sides of fingers | Medication | Standard | 2 | NS (RU)/Hg (Pre) | ACD |
| 2 | Female, 8 | No | Finger pads | Cosmetics | Standard | 2 | Thio (RU)/MCI (Pre) | ACD |
| 3 | Female, 16 | No | Diffuse | Occupational | Standard/hairdressing | 5 | PPDA (Pre)/TM (Pre)/AP (Pre)/Nit (Pre)/Dia (Pre) | ACD |
| Nit (Pre)/Dia (Pre) | ||||||||
| 4 | Male, 15 | - | Palms | Cosmetics | Standard | 3 | FM I (Pre)/PB (Pre)/Thio (RU) | ACD |
| 5 | Female, 16 | - | Sides of fingers | Cosmetics | Standard | 2 | MCI (Pre)/Thio (RU) | ACD |
| 6 | Male, 5 | - | Palms | Cosmetics | Standard | 2 | FM I (PR)/PB (PR) | ACD |
| 7 | Male, 9 | No | Palms | Unknown | Standard/cosmetics | 3 | OG (Pre)/PG (Pre)/DG (Pre) | ICD |
| 8 | Male, 5 | No | Palms | Cosmetics | Standard/fragrance | 5 | FM I (Pre)/PB (Pre)/Iso (Pre)/Jas (Pre) | ACD |
| 9 | Female, 14 | No | Dorsum | Tattoo | Standard/hairdressing/dyes | 1 | Harquus dyes (Pre) | ACD |
| 10 | Male, 8 | AD | Palms | Cosmetics | Standard/fragrance | 3 | FM I (Pre)/PB (Pre)/MCI (Pre) | ACD |
| 11 | Female, 11 | AD | Palms | Unknown | Standard | 1 | Cob (RU) | AD |
| 12 | Female, 12 | AD and FA | Lateral aspect of fingers | Cosmetics | Standard | 1 | MCI (Pre) | ACD |
| 13 | Male, 5 | AD and FA | Palms | Cosmetics | Standard | 2 | MCI (Pre)/Pal (Pre) | ACD |
| 14 | Male, 12 | AD | Lateral aspect of fingers | Unknown | Standard | 2 | Thio (RU)/Hg (RU) | ICD |
| 15 | Female, 14 | No | Finger pads | Unknown | Standard | 1 | Hg (RU) | ICD |
| 16 | Female, 12 | No | Lateral aspect of fingers | Cosmetics | Standard/fragrance | 7 | MFI (Pre)/FM II (Pre)/Ger (Pre)/Hyd (Pre)/NS (Pas)/Cob (Pas)/Citral (Pre) | ACD |
Abbreviations: ACD, atopic contact dermatitis; AD, atopic dermatitis; AP, ammonium persulfate; Cob, cobalt chloride; Dia, 2-5-diamine toluene; DG, dodecyl gallate; Dys, dyshidrosis; Eug, eugenol; FA, familial atopy; FM I, fragrance mix I; Ger, geraniol; Hg, mercury; Hyd, hydroxycitronellal; ICD, irritant contact dermatitis; Iso, isoeugenol; Jas, jasmine absolute; MCI, methylchloroisothiazolinone; Nit, 2-nitro-4-phenyl; NS, nickel sulfate; OG, octyl gallate; Pal, palladium chloride; PA, personal atopy; Pas, past relevance; PB, Peru balsam; PG, propyl gallate; PPDA, paraphenylenediamine base; Pre, present relevance; RU, relevance unknown; Thio, thiomersal; TM, thiuram mix.
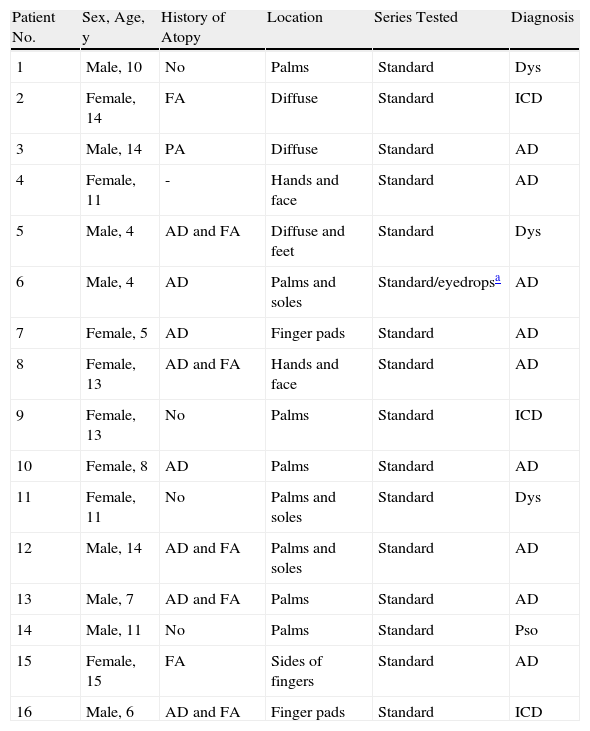
Characteristics of Children With Hand Eczema and Positive Patch Test Results.
| Patient No. | Sex, Age, y | History of Atopy | Location | Series Tested | Diagnosis |
| 1 | Male, 10 | No | Palms | Standard | Dys |
| 2 | Female, 14 | FA | Diffuse | Standard | ICD |
| 3 | Male, 14 | PA | Diffuse | Standard | AD |
| 4 | Female, 11 | - | Hands and face | Standard | AD |
| 5 | Male, 4 | AD and FA | Diffuse and feet | Standard | Dys |
| 6 | Male, 4 | AD | Palms and soles | Standard/eyedropsa | AD |
| 7 | Female, 5 | AD | Finger pads | Standard | AD |
| 8 | Female, 13 | AD and FA | Hands and face | Standard | AD |
| 9 | Female, 13 | No | Palms | Standard | ICD |
| 10 | Female, 8 | AD | Palms | Standard | AD |
| 11 | Female, 11 | No | Palms and soles | Standard | Dys |
| 12 | Male, 14 | AD and FA | Palms and soles | Standard | AD |
| 13 | Male, 7 | AD and FA | Palms | Standard | AD |
| 14 | Male, 11 | No | Palms | Standard | Pso |
| 15 | Female, 15 | FA | Sides of fingers | Standard | AD |
| 16 | Male, 6 | AD and FA | Finger pads | Standard | ICD |
Abbreviations: AD, atopic dermatitis; Dys, dyshidrosis; FA, familial atopy; ICD, irritant contact dermatitis; PA, personal atopy; Pso, psoriasis.
The adult population comprised 214 women and 282 men. The distribution of eczema in this group was as follows: hands, 127 (25.6%); palms, 84; dorsum of the hands, 49; palms and dorsum, 17; finger pads, 48; sides of the fingers, 55; dorsum of the fingers, 6; hands and feet, 65; hands and face, 16; hands and arms, 15; and palms and soles, 14. We recorded a history of atopy in 161 of the 496 adults (Table 2).
Patch testsPediatric populationPositive patch test results were recorded in 53 (37.6%) patients.
Table 1 shows the distribution of positive results by sex and age group. Of the 20 children with a history of atopic dermatitis, 20% had at least 1 positive result, whereas in the remaining 50 with no history of atopic dermatitis, 42% had at least 1 positive result (P=.08).
The most common allergens were thiomersal (17 cases), nickel sulfate (11 cases), chrome (8 cases), mercury (8 cases), methylchloroisothiazolinone (8 cases), palladium chloride (7 cases), fragrance mix I (6 cases), and Peru balsam (6 cases).
The most common confirmed diagnosis in the pediatric population was atopic dermatitis (46 patients, 32.6%), followed by allergic contact dermatitis (40 patients), irritant contact dermatitis (24 patients), and psoriasis (3 patients). The most frequent causes of eczema in patients with allergic contact dermatitis were clothing (including footwear, 19 patients), medication (17 patients), and cosmetics (14 patients) (Table 1).
Pediatric population with hand eczemaAt least 1 positive result was observed in 16 children with hand eczema (50%). Tables 1 and 4 show the distribution of positive results by sex and age group. We recorded 42 positive results. The mean number of positive allergens per patient with positive patch test results was 2.62 per patient. Of the 11 children with a history of atopic dermatitis, 45.5% had at least 1 positive result in the patch tests. Of the 17 children with no history of atopic dermatitis, 47% had at least 1 positive result (P=.9).
The most common allergens in this group were methylchloroisothiazolinone (Kathon CG) and fragrance mix I, both with 5 positive results, followed by thiomersal with 4, Peru balsam with 4, and mercury with 3. Only 2 positive results were recorded for nickel sulfate.
Twelve children (34.3%) were diagnosed with allergic contact dermatitis, 10 with atopic dermatitis, 6 with irritant contact dermatitis, 3 with dyshidrotic eczema, and 1 with psoriasis. The most frequent cause of allergic contact dermatitis was cosmetics (9 patients) (Table 4).
Adult population with hand eczemaOf the 496 adults with hand eczema, 251 (50.6%) had at least 1 positive result in the patch tests. Table 2 shows the distribution by sex. Of the 10/161 adults with a history of atopic dermatitis, 30% had at least 1 positive result in the patch tests. In the 151 adults with no history of atopic dermatitis, 52.3% had a positive result (P=.17).
The most frequent allergens in the adult population were nickel sulfate (136 cases), cobalt chloride (61 cases), palladium chloride (51 cases), thiomersal (44 cases), potassium dichromate (44 cases), Peru balsam (31 cases), fragrance mix I (23 cases), methylchloroisothiazolinone (18 cases), and mercury (18 cases). The most frequent diagnosis in adult patients was irritant contact dermatitis, with 196 cases (38.9%); allergic contact dermatitis affected 137 patients, psoriasis 76, dyshidrosis 29, and allergic contact dermatitis 27. The most common source was occupational (173 patients, 34.9%), followed by cosmetics (33 patients), clothing and footwear (19 patients), and medication (16 patients) (Table 2).
RelevanceTables 1 and 2 show the number of positive results with present, past, and unknown relevance in children with eczema at any site, in children with hand eczema, and in adults with hand eczema.
If we take the group of children with hand eczema, the relevance of methylchloroisothiazolinone and fragrance mix I was considered present in 5 cases (100%), whereas that of nickel sulfate was considered past in 1 case and unknown in 1 case (Tables 1 and 4).
DiscussionHand eczema is a common skin disease in adults. The prevalence in the general population ranges from 2.0% to 8.9%.1–3 Between 20% and 30% of all skin diseases are thought to affect the hands.4–6 Warshaw et al6 recorded a prevalence of 31.6% for hand eczema in a population of patients who had undergone patch testing, a finding that was very close to the 31.9% we found in our series. In our group, hand eczema in children accounted for 22.7% of all cases of eczema, somewhat less than the 27% found by Fernández Vozmediano et al.16 In our series, children younger than 16 years accounted for 6% of all the cases of hand eczema studied. Mörtz et al17 reported that 9.2% of the pediatric population had had hand eczema at some time in their life. Therefore, hand eczema in children is common, although it is not usually studied using patch tests, probably because the condition is initially thought to be a manifestation of atopic dermatitis.
According to Lantinga et al,18 irritant contact dermatitis is the most common diagnosis in adults with hand eczema. In our adult population, the most common diagnosis was irritant contact dermatitis, followed by allergic contact dermatitis, psoriasis, and atopic dermatitis. However, the most common diagnosis in children is allergic contact dermatitis, followed by atopic dermatitis, then irritant contact dermatitis, and psoriasis, which was observed in a minority of cases. This finding supports the idea that we should recommend patch testing in all children with hand eczema, as is the case with adults.
The distribution by sex in adult patients with hand eczema reveals a slight predominance among women. The explanation lies in differences in domestic and occupational exposure, as well as in the higher rates of atopic dermatitis in women.19–21 However, we found almost no differences between the sexes in children with hand eczema or in the pediatric population with eczema. This could be because they have not yet been exposed in an occupational setting.
We observed that the prevalence of eczema increased with age.
Atopic dermatitis, whether previous or concomitant, has been reported to be a predisposing factor in children.10 Mörtz et al17 reported that 24.5% of children with atopic dermatitis had had an episode of hand eczema during their life, whereas this only occurred in 5.1% of nonatopic children. Furthermore, a Norwegian study found that around 90% of children with hand eczema had a personal history of atopic dermatitis.22 Our figures were not so high, although 39.3% of our patients had a personal history of atopic dermatitis, which is higher than that found in the pediatric population with eczema at any site (28.6%). However, we did observe that the presence of previous atopic dermatitis is 6 to 7 times greater in children than in adults and that this difference is statistically significant (P≤.05); therefore, atopic dermatitis is a predisposing factor for hand eczema at any age, although this is more so in children.
It is generally accepted that patch tests should be used in adult patients with chronic hand eczema. This very useful test can help with patient management. However, despite the frequency of hand eczema in children, we were unable to find studies on the usefulness of patch tests in this population. We found that 37.6% of patch tests were positive in children with eczema at any site. This figure increased to as much as 50% in children with hand eczema. These results do not reveal statistically significant differences between the groups.
We did not observe significant differences between the sexes or age groups; therefore, we believe that patch testing should be indicated in all children with chronic hand eczema, as is the case with adults.
The issue of whether patients with atopic dermatitis suffer more or less from allergic contact dermatitis is subject to debate.5 It is very likely that there are no differences in patients without atopic dermatitis, since their lower immunologic predisposition is offset by greater deterioration of the skin barrier and greater exposure to allergens. Such was our finding for children with hand eczema and atopic dermatitis and children with hand eczema and no history of atopic dermatitis. This is consistent with the findings of most studies5,22,23; however, we did find that children with eczema at any site and a history of atopic dermatitis had fewer positive patch test results than children without atopic dermatitis.
The most common allergens in previous studies in children were metals, rubbers, and perfumes.24–31 We found that thiomersal, metals, Kathon CG, fragrance mix I, and Peru balsam, in that order, were the most common allergens in children with eczema. These results are consistent with those of other Spanish studies, in which nickel sulfate, mercury, and thiomersal were the most common allergens.16,26 This order, however, is reversed in children with hand eczema, in whom the most common allergens were Kathon CG, fragrance mix I, thiomersal, and Peru balsam. Furthermore, the order does not coincide with that found in our adult population, where the most frequent allergens were metals (nickel, chrome, cobalt), thiomersal, fragrance mix, mercury, and Kathon CG. We stress that most positive results with Kathon CG in children were found in patients with hand eczema and that nickel was not among the most common allergens in children with hand eczema. Therefore, the allergens involved in hand eczema in the pediatric population differ from those linked to eczema at other sites.
In our study, the sources of exposure most commonly related to the allergens found in children with hand eczema were cosmetics and medications, whereas in the pediatric population with eczema at any site the most common source was footwear, followed by medication and cosmetics. Therefore, the sources of exposure most commonly related to hand eczema in children were cosmetics and hygiene products, which contain fragrances and preservatives that eventually sensitize the child.
An evaluation of the relevance of patch tests is essential if we wish to establish their usefulness.5 This element is missing in many published studies on allergic contact dermatitis in children; however, when it is included, percentages are relatively high, and clinical relevance (present or past) ranges from 40% to 87%.17,32,33 We found the present relevance of positive results in children with eczema to be 60%; in children with hand eczema, the figure was higher (76.2%). However, the difference was not statistically significant (P=.07). In contrast, among adults with hand eczema, we only found present relevance in 43% of patients with positive results, and the difference was statistically significant (P<.001) (Table 2). These findings confirm the usefulness of patch tests in children with hand eczema.
ConclusionsThere is consensus on the need to perform patch tests on adult patients with chronic hand eczema. Although hand eczema is frequent in children, we do not normally request patch tests. Our study shows that children with hand eczema in whom we performed patch testing had a higher number of positive allergens and greater present relevance. Furthermore, the allergens most frequently involved in hand eczema in children are different from those found in the other 2 groups. In children with hand eczema, allergic contact dermatitis is the most common confirmed diagnosis, ahead of atopic dermatitis. Therefore, we believe that patch testing is indicated in all children with hand eczema, as is the case with adults.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Toledo F, et al. Utilidad de las pruebas epicutáneas en el eczema de manos en niños: estudio comparativo con el eczema en la edad pediátrica y con el eczema de manos en adultos. Actas Dermosifiliogr.2011;102:429-438.