Urticaria multiforme is a cutaneous disorder that affects infants and small children. It is characterized by large, annular urticarial plaques with a violaceous center and is frequently accompanied by fever. Urticaria multiforme follows a benign, self-limiting course, but the striking appearance of the lesions can cause alarm and considerable anxiety among parents.
We present 5 cases of urticaria multiforme seen in our hospital over a period of 18 months. All the cases were preceded by an infection of the upper airways or otitis, and they were all empirically with amoxicillin. It is important to be familiar with this condition to reassure parents and avoid unnecessary hospital admissions and tests.
La urticaria multiforme es un cuadro cutáneo, propio de lactantes y niños pequeños, caracterizado por la aparición de grandes placas anulares urticariformes de centro violáceo frecuentemente asociado a un proceso febril. Tiene un curso benigno y autolimitado, pero el llamativo aspecto de las lesiones puede ser alarmante y generar gran ansiedad en los padres.
Presentamos 5 casos de urticaria multiforme vistos en nuestro hospital a lo largo de 18 meses. El antecedente común a todos ellos fue una infección de vías respiratorias altas u otitis por la que fueron tratados empíricamente con amoxicilina. Es importante saber reconocer esta entidad para tranquilizar a los padres, ahorrar el ingreso hospitalario y evitar la realización de pruebas diagnósticas innecesarias.
Urticaria multiforme (UM) is a benign, self-resolving cutaneous disorder that affects children between 4 months and 4 years of age. It is characterized by the appearance of large annular and archiform erythematous plaques with a violaceous center and is very frequently accompanied by fever.
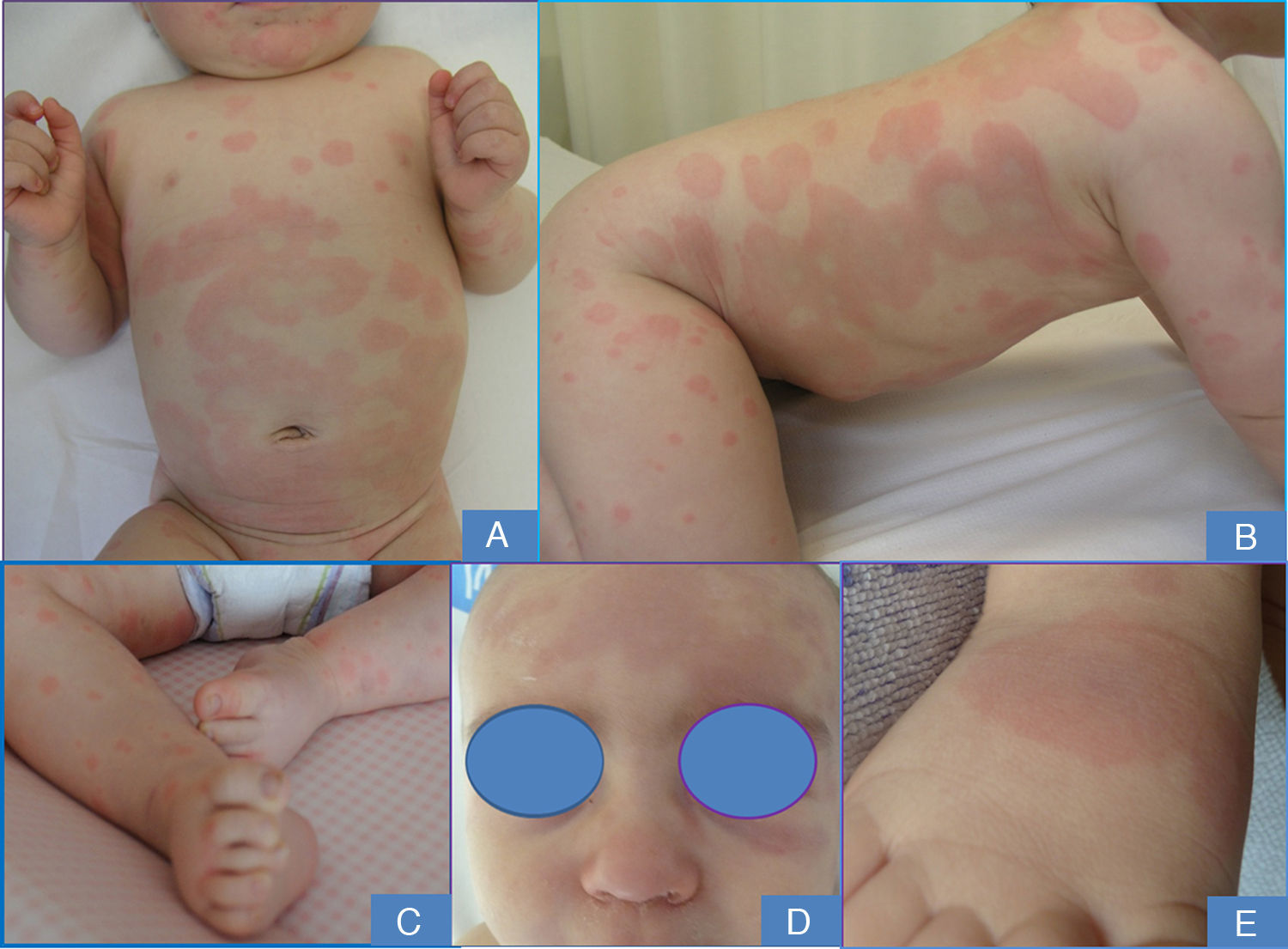
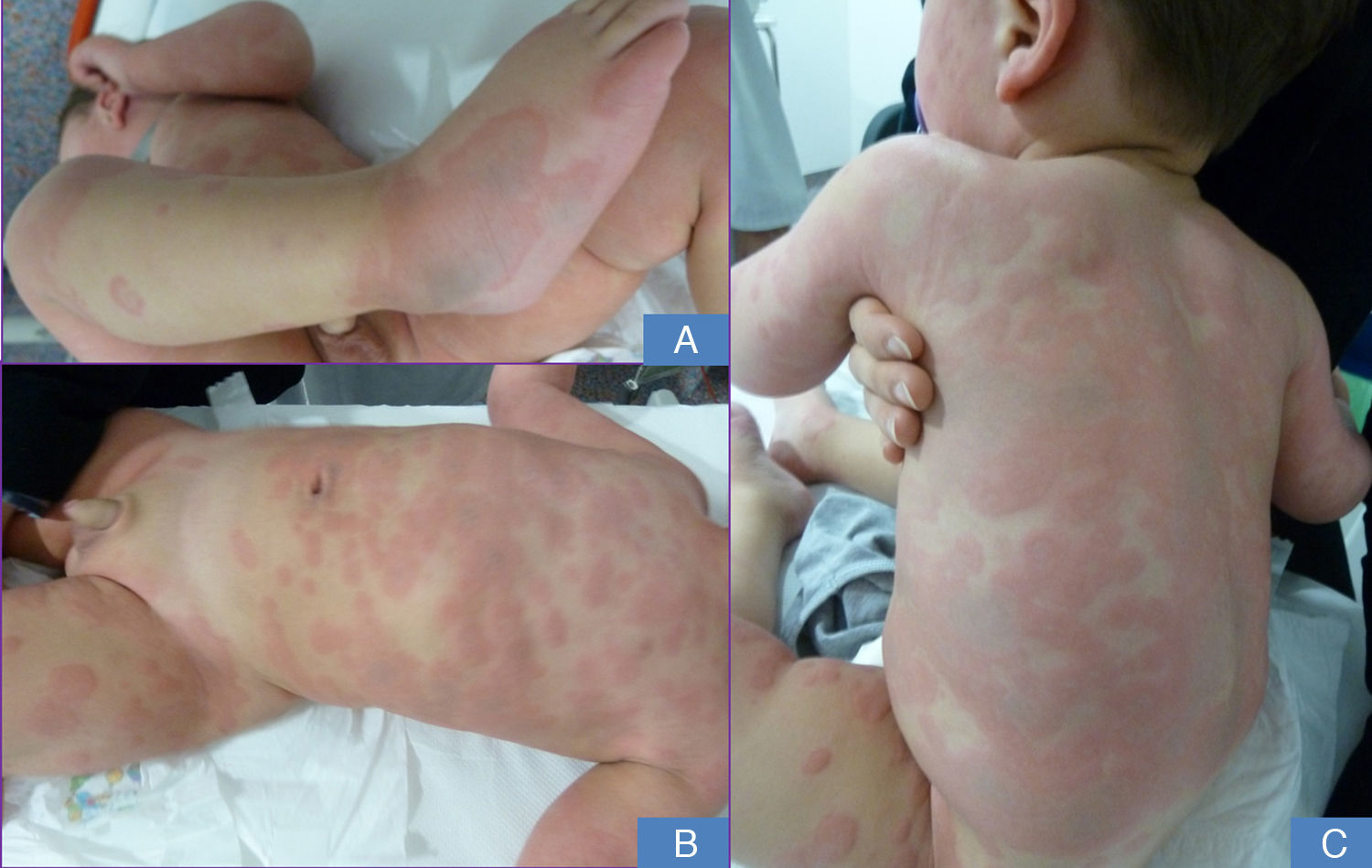
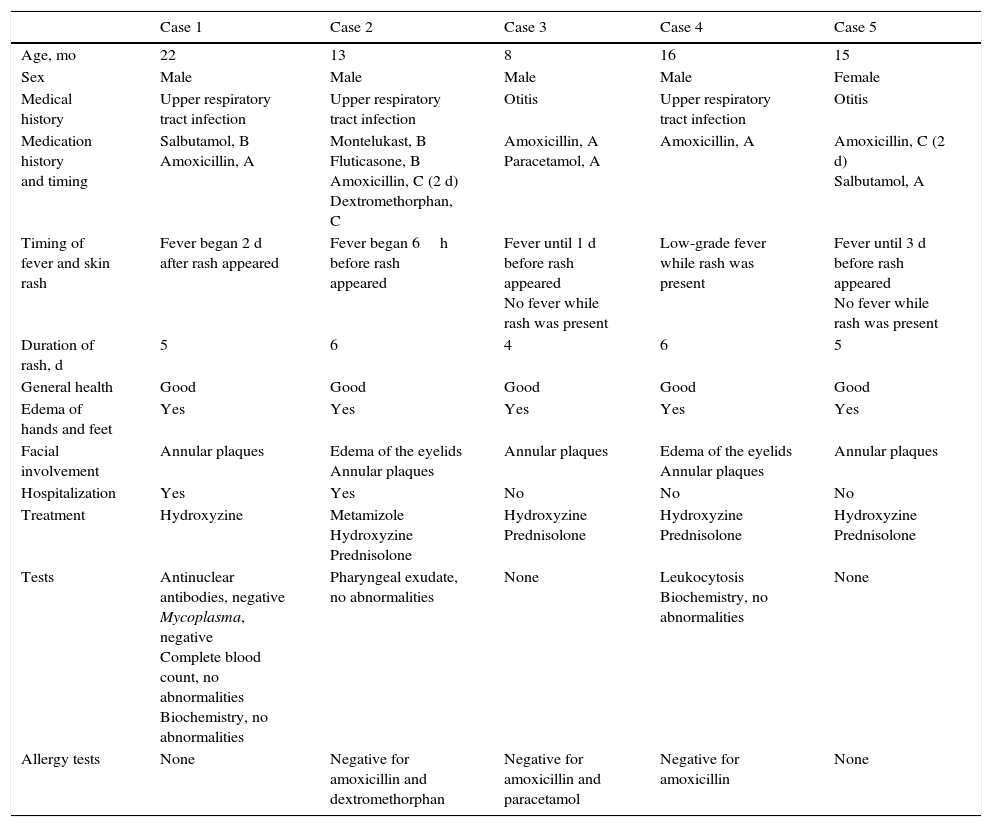
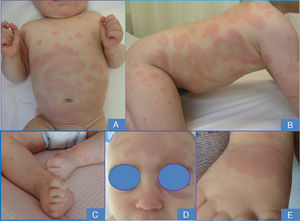
Case DescriptionsWe present 5 cases of UM seen in our hospital between December 2012 and June 2013. Case data are summarized in Table 1. The patients—4 boys and 1 girl between the ages of 8 and 22 months—were brought to our emergency department following the appearance of extensive urticarial lesions on the face, trunk, and limbs. The lesions had a violaceous center and were associated with edema of the hands and feet (Figs. 1 and 2). Despite the striking clinical appearance of the skin, the patients were in good general health. Fever was a variable finding. The mean duration of the skin lesions was 5 days, during which time oral antihistamines or corticosteroids were administered to alleviate the lesions, but new lesions continued to appear. The first 2 patients seen were admitted to the hospital, whereas the last 3 only required ambulatory follow-up. All patients had received oral amoxicillin during the course of the disease or shortly before the skin lesions appeared; 3 underwent amoxicillin allergy tests, with negative results.
Summary of Patient History in Our 5 Cases.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Age, mo | 22 | 13 | 8 | 16 | 15 |
| Sex | Male | Male | Male | Male | Female |
| Medical history | Upper respiratory tract infection | Upper respiratory tract infection | Otitis | Upper respiratory tract infection | Otitis |
| Medication history and timing | Salbutamol, B Amoxicillin, A | Montelukast, B Fluticasone, B Amoxicillin, C (2 d) Dextromethorphan, C | Amoxicillin, A Paracetamol, A | Amoxicillin, A | Amoxicillin, C (2 d) Salbutamol, A |
| Timing of fever and skin rash | Fever began 2 d after rash appeared | Fever began 6h before rash appeared | Fever until 1 d before rash appeared No fever while rash was present | Low-grade fever while rash was present | Fever until 3 d before rash appeared No fever while rash was present |
| Duration of rash, d | 5 | 6 | 4 | 6 | 5 |
| General health | Good | Good | Good | Good | Good |
| Edema of hands and feet | Yes | Yes | Yes | Yes | Yes |
| Facial involvement | Annular plaques | Edema of the eyelids Annular plaques | Annular plaques | Edema of the eyelids Annular plaques | Annular plaques |
| Hospitalization | Yes | Yes | No | No | No |
| Treatment | Hydroxyzine | Metamizole Hydroxyzine Prednisolone | Hydroxyzine Prednisolone | Hydroxyzine Prednisolone | Hydroxyzine Prednisolone |
| Tests | Antinuclear antibodies, negative Mycoplasma, negative Complete blood count, no abnormalities Biochemistry, no abnormalities | Pharyngeal exudate, no abnormalities | None | Leukocytosis Biochemistry, no abnormalities | None |
| Allergy tests | None | Negative for amoxicillin and dextromethorphan | Negative for amoxicillin and paracetamol | Negative for amoxicillin | None |
Abbreviations: A, patient was taking medication when the cutaneous signs appeared; B, patient was taking usual medication; C, patient had been taking medication in the days prior to the appearance of urticaria multiforme.
UM is an acute skin disorder that typically affects infants and very small children and tends to be accompanied by fever and good general health. The typical lesions are initially small urticarial lesions that spread outward and coalesce into large archiform plaques with polycyclic borders and a violaceous center. The individual lesions have a duration of less than 24hours, can affect any part of the body, and tend to be associated with edema of the face, hands, and feet. The lesions disappear spontaneously in 6 to 10 days without leaving any residual pigmentation.
UM was first described in 1997 by Tamayo-Sánchez et al.,1 who observed 34 patients with a rash that they called acute annular urticaria and which they proposed differentiating from acute urticaria. Ten years later, Shah et al.2 reported a new series of 19 cases and proposed the term urticaria multiforme because of the similarity of the entity to erythema multiforme. Unlike Tamayo-Sánchez et al., Shah et al. considered the disorder to be a subtype of urticaria because they found that the patients presented dermographism and pruritus, whereas Tamayo-Sánchez et al. had doubted whether pruritus was present because they did not find scratch lesions on any of their patients.
The clinical diagnostic criteria that both authors agree on are as follows:
- –
Large annular plaques with a transient ecchymotic center.
- –
Individual lesions with a duration of less than 24hours.
- –
Associated episode of fever.
- –
Total duration of disease: less than 10 days.
- –
Edema of the limbs.
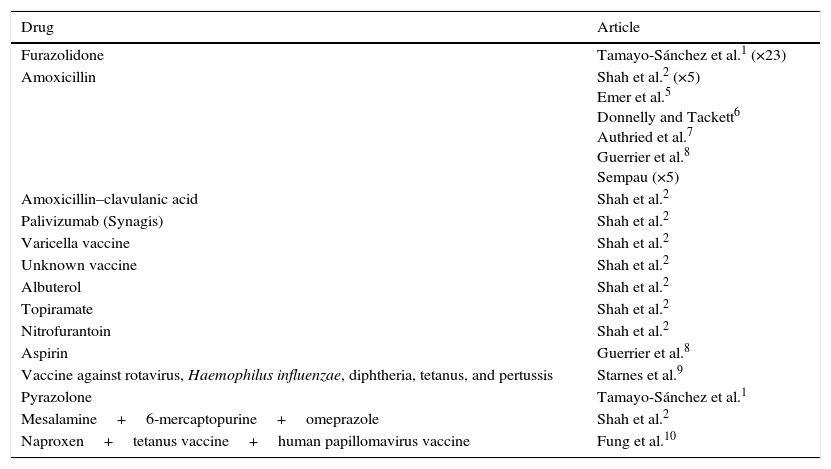
The etiology of UM is unknown. In the few reported cases in which the infectious agent was investigated, micoplasm,2,3 adenovirus,2Streptococcus organisms,2 herpes virus 6,4 and the Epstein-Barr virus5 were detected. However, most reports indicate the medications that the patient had been receiving before the appearance of the lesions (Table 2).1,2,5–10 Common medications include amoxicillin and furazolidone (an antibiotic used in the treatment of giardiasis in Mexico), which had been administered in 19 of the 34 cases reported by Tamayo-Sánchez. Likewise, vaccination in the days prior to symptom onset is frequently reported.2,9,10 In our series, all 5 patients had been taking amoxicillin at the time the lesions appeared or up to 3 days before the appearance of the lesions.
Drugs and Vaccines Associated With Urticaria Multiforme in the Literature.
| Drug | Article |
|---|---|
| Furazolidone | Tamayo-Sánchez et al.1 (×23) |
| Amoxicillin | Shah et al.2 (×5) Emer et al.5 Donnelly and Tackett6 Authried et al.7 Guerrier et al.8 Sempau (×5) |
| Amoxicillin–clavulanic acid | Shah et al.2 |
| Palivizumab (Synagis) | Shah et al.2 |
| Varicella vaccine | Shah et al.2 |
| Unknown vaccine | Shah et al.2 |
| Albuterol | Shah et al.2 |
| Topiramate | Shah et al.2 |
| Nitrofurantoin | Shah et al.2 |
| Aspirin | Guerrier et al.8 |
| Vaccine against rotavirus, Haemophilus influenzae, diphtheria, tetanus, and pertussis | Starnes et al.9 |
| Pyrazolone | Tamayo-Sánchez et al.1 |
| Mesalamine+6-mercaptopurine+omeprazole | Shah et al.2 |
| Naproxen+tetanus vaccine+human papillomavirus vaccine | Fung et al.10 |
Histologic studies have been carried out in only 3 cases.1,5 In these patients, histology revealed dermal edema with a perivascular lymphocytic infiltrate and a few eosinophils, but no epidermal involvement. On the basis of these findings, UM can be differentiated from erythema multiforme (which is usually associated with epidermal necrosis) and from acute urticaria (which is not normally associated with perivascular lymphocytic infiltrate).
The only treatment proposal put forth by Tamayo-Sánchez et al. is the introduction of antipyretics if fever is present and the suspension of suspicious medications, whereas Shah et al. recommend the use of antihistamines on the grounds that UM is a type of urticaria. All other authors propose the use of antihistamines for symptom relief.5,6,8–10 Our 5 patients initially received treatment with antihistamines, and oral corticosteroids were added when symptoms persisted. Both treatments alleviated the existing skin lesions but neither prevented the appearance of new lesions; we therefore doubt the utility of oral corticosteroids in UM. Like Tamayo-Sánchez et al., we observed no signs of scratching in our patients.
The differential diagnosis of UM includes other annular lesions11,12 such as acute urticaria (which is usually associated with intense pruritus but not with fever and lacks central bluish pigmentation), erythema multiforme, and urticarial vasculitis (in which the individual lesions usually persist for several days and leave residual lesions. Facial and acral edema may require differential diagnosis with a drug-induced serum sickness–like reaction that is typically (but not exclusively) associated with the administration of cefaclor and vaccines. This type of reaction appears around 7 to 10 days after the start of treatment and presents as urticarial lesions with a dark center. In contrast to UM, however, the lesions do not have day-to-day fluctuation and tend to be associated with general malaise, arthralgia, and enlarged lymph nodes. Finally, it is important to differentiate UM from acute hemorrhagic edema of infancy, which also appears in children under 24 months of age in association with low-grade fever and has little impact on general health. Unlike UM, in acute hemorrhagic edema of infancy purpuric plaques appear and spread outward, forming annular, targetoid lesions, occasionally with a necrotic or bullous center, which last several days and leave residual pigmentation.
ConclusionsThe 5 cases described in this article were seen over the course of 18 months, suggesting that UM is a relatively frequent entity in routine clinical practice. In all 5 cases, the patient had a history of upper respiratory tract infection and had been receiving amoxicillin in the days before the lesions appeared—a finding reported in practically all cases described in the literature. Because UM has an alarming appearance but a benign course, it is important that physicians be able to recognize it in order to reassure the family and avoid unnecessary hospital admissions and diagnostic tests.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that they followed their hospitals’ regulations regarding the publication of patient information.
Right to privacyThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sempau L, Martín-Sáez E, Gutiérrez-Rodríguez C, Gutiérrez-Ortega MC. Cinco casos de urticaria multiforme y revisión de la literatura. Actas Dermosifiliogr. 2016;107:e1–e5.