Amastigotes of the genus Leishmania have been observed in biopsies of apparently unrelated lesions in patients with AIDS and visceral leishmaniasis. We describe the case of a 40-year-old man with human immunodeficiency virus infection and severe immunodepression in whom the presence of the parasite was detected as an incidental finding on histological study of a perianal squamous cell carcinoma. This finding led to the diagnosis and subsequent treatment of previously unsuspected visceral leishmaniasis. In a review of the literature we have found no previous examples of this association.
En pacientes con SIDA y leishmaniasis visceral ha sido descrita la presencia de amastigotes de Leishmania en biopsias realizadas para estudiar diversas lesiones con las que no guardan aparente relación causal. Presentamos el caso de un varón de 40 años, VIH positivo severamente inmunodeprimido, en el que se observó incidentalmente la presencia del parásito al estudiar histológicamente un carcinoma epidermoide perianal. Dicho hallazgo permitió el diagnóstico y tratamiento de una leishmaniasis visceral insospechada. No hemos encontrado en la literatura ejemplos previos de esta asociación.
Amastigotes of the genus Leishmania have been observed in biopsies of apparently unrelated lesions in patients who have both AIDS and visceral leishmaniasis.1,2 We report the case of a man in whom the presence of the parasite was detected in a perianal squamous cell carcinoma. This association has not been reported in the literature to date.
Case DescriptionA 40-year-old human immunodeficiency virus (HIV)-infected homosexual man had been receiving antiretroviral therapy (abacavir, etravirine, and raltegravir) since 2005. He had been referred to our department on several occasions for evaluation of perianal condylomata, which were treated with cryotherapy. In April 2010, he was again referred for an erosive, erythematous, verrucous perianal plaque that had developed several months earlier (Fig. 1). A biopsy was performed to rule out malignant transformation.
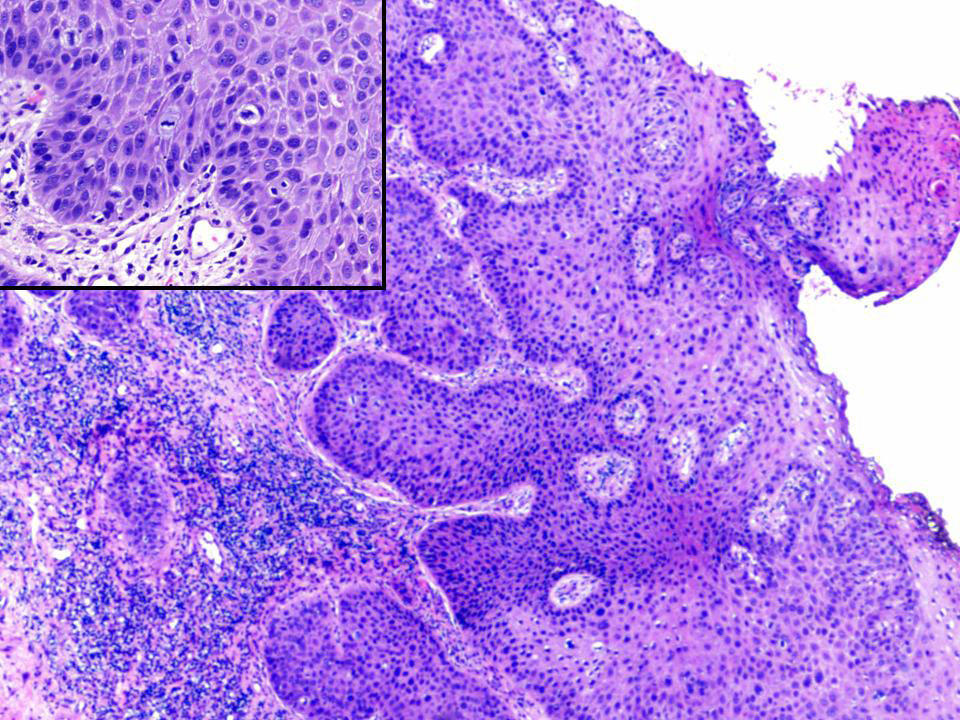
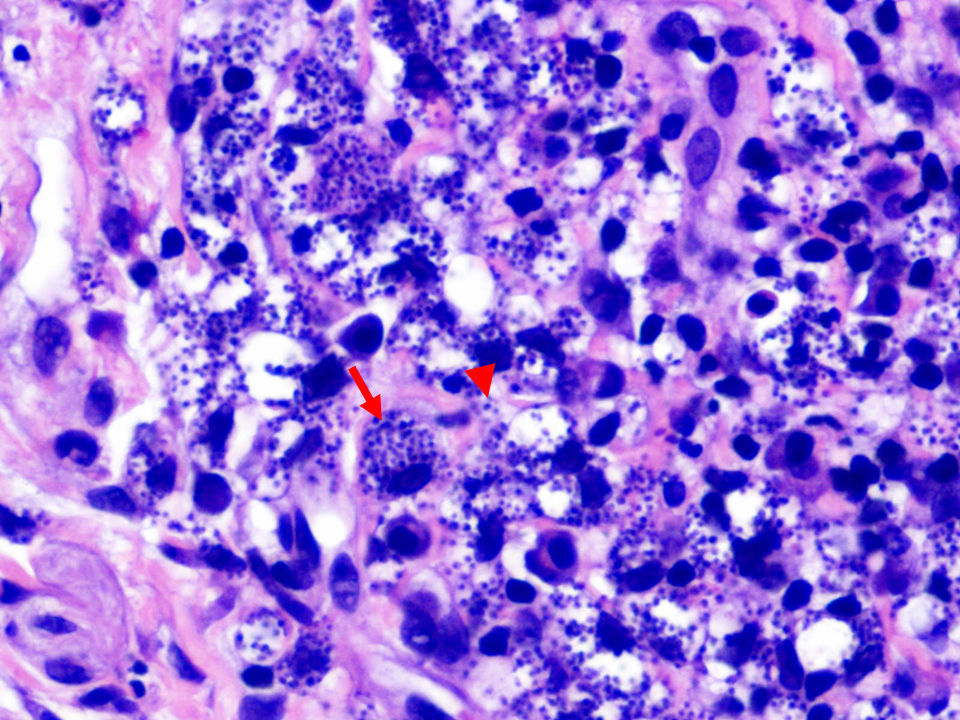
Histopathology revealed marked epidermal acanthosis, pleomorphic keratinocytes, and the presence of atypical mitotic figures, confirming the suspected clinical diagnosis of squamous cell carcinoma (Fig. 2). In the dermis, numerous amastigotes of the genus Leishmania were observed both inside the macrophages and in the intercellular matrix (Fig. 3). In situ hybridization for high-risk human papillomavirus (HPV) revealed strong, punctate, nuclear staining. Immunohistochemistry was positive for p16 in neoplastic areas.
Extensive, predominantly lymphocytic inflammatory infiltrate and abundant macrophages; round or oval basophilic structures can be seen both inside the cytoplasm (arrow) and in the intercellular matrix (arrowhead), consistent with Leishmania amastigotes (hematoxylin-eosin, original magnification ×400).
On elicitation of additional history, the patient reported that his dog had died of leishmaniasis 4 years earlier and that he frequently traveled from his home in Valencia to Morocco on business.
Blood tests revealed a CD4 cell count of 90/μL, an undetectable HIV load (<20 copies/mL), and an erythrocyte sedimentation rate of 116mm/h. The total white blood cell count and platelet count were normal and the patient was only slightly anemic (hemoglobin 11.9g/dL).
The patient refused to undergo bone marrow sampling, so the infectious diseases department started empiric treatment with meglumine antimoniate (20mg/kg of a pentavalent antimony compound once daily for 28 days). The patient was also scheduled for excision of the tumor. Histologic examination of the excised tissue confirmed the presence of Leishmania organisms, despite completion of the antimonial treatment. The patient then agreed to a bone marrow procedure; involvement of the marrow was detected, confirming the diagnosis of visceral leishmaniasis. In view of these findings, the patient was prescribed treatment with liposomal amphotericin B. Because his CD4 cell count remained below 200/μL, on completion of treatment he began secondary chemoprophylaxis with monthly administration of liposomal amphotericin B. After 9 months, no clinical or analytical signs of visceral leishmaniasis were evident. He currently attends regular follow-up visits at the infectious diseases department.
DiscussionLeishmaniasis is caused by infection with protozoa of the genus Leishmania, which are spread by female sandflies of the genera Phlebotomus and Lutzomyia. The Leishmania protozoa parasitize the monocyte-macrophage system in the form of amastigotes. In Spain, dogs are the main reservoir of the causative species,3Leishmania infantum.4
Immunocompromised patients bitten by an infected vector are at high risk of developing visceral leishmaniasis.3 Most cases of visceral leishmaniasis were once found in children, but at present 70% occur in adults, and 50% of such cases are in HIV-positive individuals.4,5 Spain and the rest of southwestern Europe have the world's highest prevalence of coinfection, and intravenous drug users are at the greatest risk.1-6
HIV/Leishmania organism coinfection favors the progression of both infections. CD4+ type 1 helper T cells, which are depleted in HIV-infected patients, play a fundamental role in the immune response to the parasite. HIV infection therefore increases the risk of developing visceral leishmaniasis by a factor of 100 to 2300, worsens prognosis, and decreases the likelihood of therapeutic response.4,6 Furthermore, the presence of Leishmania amastigotes has been shown to increase HIV replication, diminish immune status, and hasten progression to AIDS.6
Visceral leishmaniasis spreads to the skin more frequently in HIV-infected patients than in immunocompetent patients2 and manifests as lesions spanning a wide clinical spectrum.1,4,7 In addition, the presence of Leishmania organisms has been observed in biopsy specimens from patients with skin conditions not caused by the parasite, such as Kaposi sarcoma, dermatofibromas, psoriasis, aphthous ulcers, herpes simplex, herpes zoster, bacillary angiomatosis, tattoos, and rheumatoid nodules.1,2
In our patient, the disease was detected incidentally on biopsy of a perianal squamous cell carcinoma. To our knowledge, this association has not been previously reported. The patient's epithelioma does not appear to have been caused by the parasite; had it been, it would suggest a relationship with chronic HPV infection. The growth was probably caused by massive dissemination of the parasite in this severely immunocompromised patient. Local inflammation caused by growth of the carcinoma, accompanied by an abundance of histiocytes in a heavily parasitized mononuclear phagocyte system, would explain findings of abundant amastigotes.1,4,8 This finding in our patient led to further tests though which previously unsuspected visceral involvement was detected. Appropriate systemic treatment, as described elsewhere,2 was then prescribed.
This is the first report of an association between Leishmania parasites and squamous cell carcinoma. In HIV-positive patients in whom skin biopsy reveals evidence of Leishmania parasites, underlying visceral leishmaniasis should be suspected. Bone marrow sampling would seem to be indicated, as the results will guide treatment choice and ultimately influence prognosis.2,4
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Armengot-Carbó M, et al. Leishmaniasis visceral insospechada infiltrando un carcinoma epidermoide. Actas Dermosifiliogr.2012;103:321-323.