Scleromyxedema is a potentially serious disease that can have various systemic complications. One of the most frequent forms of central nervous system involvement is dermato-neuro syndrome. High-dose intravenous immunoglobulins are among the drug treatments that have been used for this syndrome. We describe 2 patients with scleromyxedema, one of whom developed dermato-neuro syndrome. Both patients responded well to treatment with high-dose intravenous immunoglobulins. We suggest this therapy as a suitable first-line treatment for scleromyxedema and for its neurological complications.
El escleromixedema es una enfermedad potencialmente grave que puede asociarse a complicaciones sistémicas diversas, entre las que se encuentran las que involucran al sistema nervioso central, siendo el síndrome dermato-neuro una de las más infrecuentes. Se han utilizado para su tratamiento fármacos variados, entre ellos, altas dosis de inmunoglobulinas endovenosas. Se describen dos casos de escleromixedema, uno de los cuales desarrolló un síndrome dermato-neuro, ambos con una excelente respuesta al tratamiento con inmunoglobulinas endovenosas. El uso de altas dosis de inmunoglobulinas endovenosas en el tratamiento de esta enfermedad y sus complicaciones neurológicas se perfila como un tratamiento de primera línea.
Scleromyxedema is an uncommon disease characterized by mucin deposits, fibrosis, and proliferation of fibroblasts in the dermis. It is often associated with paraproteinemia and very varied systemic manifestations,1-3 the most notable of which—because of its rarity—is the so-called dermato-neuro syndrome.4 Response to the treatment of this disease and its complications is often disappointing, although favorable results have been achieved in recent years with intravenous immunoglobulin (IVIG).
We report on 2 patients with scleromyxedema, one of whom developed neurocutaneous syndrome. Both patients had an excellent response to IVIG.
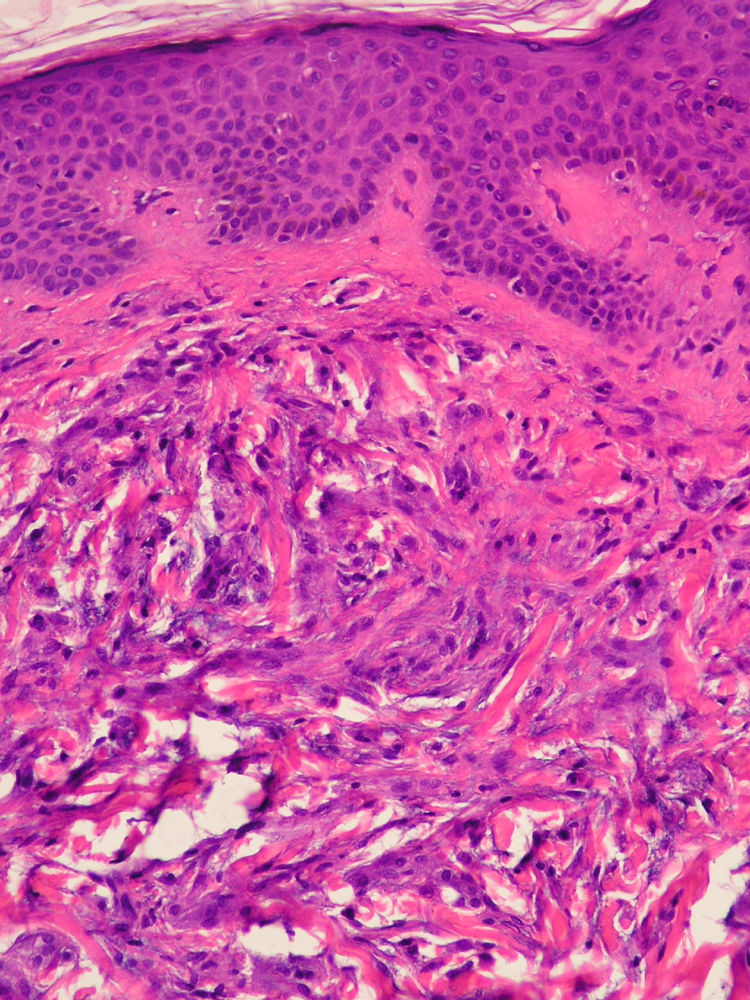
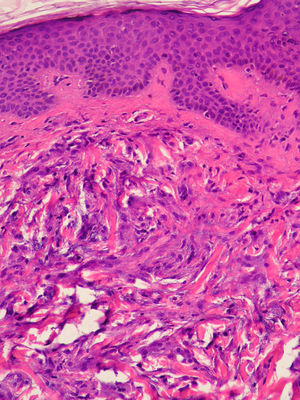
Case DescriptionsPatient 1A 72-year-old man with a diagnosis of scleromyxedema was referred to our department in 2005 for follow-up and treatment. Physical examination revealed firm, waxy papules (2-3mm) arranged close together on the auricle of the ear, the face, and the dorsum of the hands. In addition, the skin was hard and thick to the touch at these sites and on the neck, chest, and arms (Figs. 1 and 2). Microscopy revealed an irregularly distributed proliferation of fibroblasts in the dermis, together with increased collagen fibers and diffuse mucin deposits in the middle reticular and papillary dermis (Fig. 3). Protein electrophoresis revealed a monoclonal band of immunoglobulin (Ig) Gλ; bone marrow aspirate was normal. Echocardiography revealed mild asymptomatic pulmonary hypertension. The patient received various treatments over the following years, including melphalan, retinoids, corticosteroids, thalidomide, and photochemotherapy; however, the response was poor. In March 2008, the patient began treatment with IVIG (2g/kg/mo) and initially experienced a notable improvement (skin less thickened, greater mobility of the limbs, and increased mouth opening) that did not continue during the following months. IVIG was, therefore, stopped after 7 cycles. The patient then received chlorambucil for 4 months, with no improvement. In April 2009, following placement of a partially tunneled central catheter, extracorporeal photopheresis was started. After the second session of the first cycle, the patient went to the emergency department complaining of fever (38°C) that had started 24hours earlier with no accompanying symptoms. The laboratory workup showed neutrophilia (90%) with no leukocytosis. Blood cultures were positive for Streptococcus lugdunensis, although this entity was not detected in the catheter culture. The patient's initial progress with antibiogram-guided antibiotic therapy was good; however, on the fifth day of admission he presented 2 episodes of tonic-clonic seizures preceded by high fever (39°C) and hypertension in less than 24hours. The second episode was followed by diminished level of consciousness and stupor. The patient went into coma and was intubated for mechanical ventilation. His condition did not improve despite therapy with anticonvulsants. Two new blood cultures and a catheter tip culture were negative. No abnormal findings were detected in electroencephalography, lumbar puncture, cranial computed tomography, magnetic resonance imaging, or magnetic resonance angiography. On suspicion of dermato-neuro syndrome associated with scleromyxedema, treatment with IVIG (2g/kg) and methylprednisolone (100mg/d) was started for 2 days and then tapered. The neurological symptoms gradually improved, and the patient gradually recovered consciousness. Progress was good, and no neurological sequelae were observed. One year and 9 months later, the patient continues to receive IVIG, which is administered once monthly. He has not experienced seizures or any further episodes of reduced consciousness. The monoclonal band persisted despite treatment.
A 52-year-old woman with hypothyroidism and dyslipidemia consulted with a 6-month history of skin lesions that had first appeared on the dorsum of the hands and gradually extended to the arms, legs, face, and auricle of the ears. The patient also reported paresthesia in her hands, which she found difficult to close. No other symptoms were recorded. The lesions took the form of skin-colored papules (1 to 3mm) that coalesced in some areas, with mild erythema and induration of the skin (Figs. 4 and 5). One biopsy specimen was taken from the dorsum of the hand and another from the arm. The changes observed were characteristic of scleromyxedema. Additional investigations revealed bilateral carpal tunnel syndrome, and protein electrophoresis revealed a monoclonal band of IgGλ, with no evidence of myeloma. Treatment was started with IVIG (2g/kg/mo) and prednisone (0.5mg/kg/d [30mg/d]). Symptoms improved notably after 2 months, with increased mobility in the hands and reduced infiltration of the skin. Prednisone was tapered from this point and discontinued 2 months later. After 1 year of uninterrupted treatment with IVIG and no systemic corticosteroids, the patient remains stable with no complications, although the monoclonal band has persisted.
Scleromyxedema is a chronic, unpredictable, and occasionally fatal systemic disease, and no consensus has been reached on its treatment.
The 2 cases we report presented unequivocal manifestations of scleromyxedema. Two findings are of particular interest, namely, the development in 1 patient of dermato-neuro syndrome and the favorable response to IVIG,initially combined with systemic corticosteroids.
One of the most unusual neurologic complications, affecting less than 10% of patients with scleromyxedema,5 is dermato-neuro syndrome, which involves a combination of fever, seizures, and coma that is often preceded by flu-like symptoms.6 Some 10 cases have been reported.7 The first of our patients developed the symptoms of this syndrome 6 months after discontinuing IVIG and after 2 sessions of his first cycle of extracorporeal photopheresis. Although fever has been described as a side effect of extracorporeal photopheresis, a relationship between this procedure and other more severe manifestations (eg, seizures and coma) seems unlikely. Therefore, after ruling out other possible causes, we reached a diagnosis of dermato-neuro syndrome.
The mechanism responsible for dermato-neuro syndrome remains unknown. Paraproteinemia is thought to increase blood viscosity or favor the formation of neutrophil aggregates that alter microcirculation. Increased levels of endogenous benzodiazepines have also been postulated.6 The syndrome has been associated with increased intervals between IVIG infusions7 and reduced doses of immunoglobulins.8,9 In our case, the onset of this complication coincided with the discontinuation of IVIG.
The very low incidence of scleromyxedema and our poor understanding of its pathogenesis explain why no consensus has been reached on treatment and randomized clinical trials are lacking. Given the presence of paraproteinemia, and following the approach used to treat myeloma, drugs such as melphalan, thalidomide, and corticosteroids, both alone and in combination, have proven successful in specific cases.2,10,11 However, the toxicity of long-term melphalan2 and the risk of peripheral neuropathy with thalidomide limit the use of these drugs over extended periods. Treatment of severe and disfiguring disease with hematopoietic stem cell transplantation12,13 and high-dose IVIG has proven increasingly successful in the last 10 years. In patient 1, we achieved no response whatsoever with melphalan, thalidomide, or photochemotherapy; consequently, and given the considerable progression of the disease, we successfully administered high-dose IVIG, which was followed by a rapid initial response and reversal of dermato-neuro syndrome. Our previous experience meant that our first option for patient 2 was IVIG, which was also successful.
Treatment schedules for dermato-neuro syndrome are not clear, and the outcome of plasmapheresis14 and corticosteroids,15 both alone and in combination,7 has varied. IVIG combined with corticosteroids, as in our patient 1, has been used in only 1 case.8 The mechanism by which scleromyxedema and its complications respond to IVIG is unknown; however, the drug is thought to reduce fibrosis by blocking an as yet unidentified circulating fibroblast-stimulating factor.8
To conclude, the growing number of cases of scleromyxedema with dermato-neuro syndrome seems to confirm the syndrome as a potentially fatal complication of the disease. Furthermore, IVIG combined with corticosteroids during the early stages of the disease is seen as a relatively safe first-line option, although it is not free of side effects.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Bielsa I, et al. Escleromixedema y syndrome dermato-neuro: Buena respuesta al tratamiento con glucocorticoides e inmunoglobulinas endovenosas. Actas Dermosifiliogr.2012;103:317-20.