Mycosis fungoides (MF) is the most common cutaneous T-cell lymphoma, and accounts for more than half of all primary cutaneous T-cell lymphomas. Diagnosis of this condition is based on clinical and histopathological criteria. MF is one of several dermatological conditions that can mimic other diseases; its many clinical presentations include the unilesional form, first described by Jones and Chu.1 Here, we describe 3 different clinical manifestations of unilesional MF: a red scaly plaque, a purpuric lesion, and a tumor of elastic consistency.
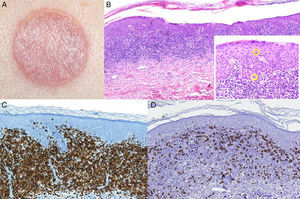
The first patient was a 75-year-old woman with a history of hypothyroidism, endometrial adenocarcinoma, ovarian cyst, hypertension, cataracts, and bipolar disorder. She was being treated with levothyroxine sodium, lamotrigine, venlafaxine, and lithium carbonate. She presented with a round, erythematous plaque of about 5cm in diameter with fine scales. The plaque was located in the interscapular area and had appeared about 6 months previously.
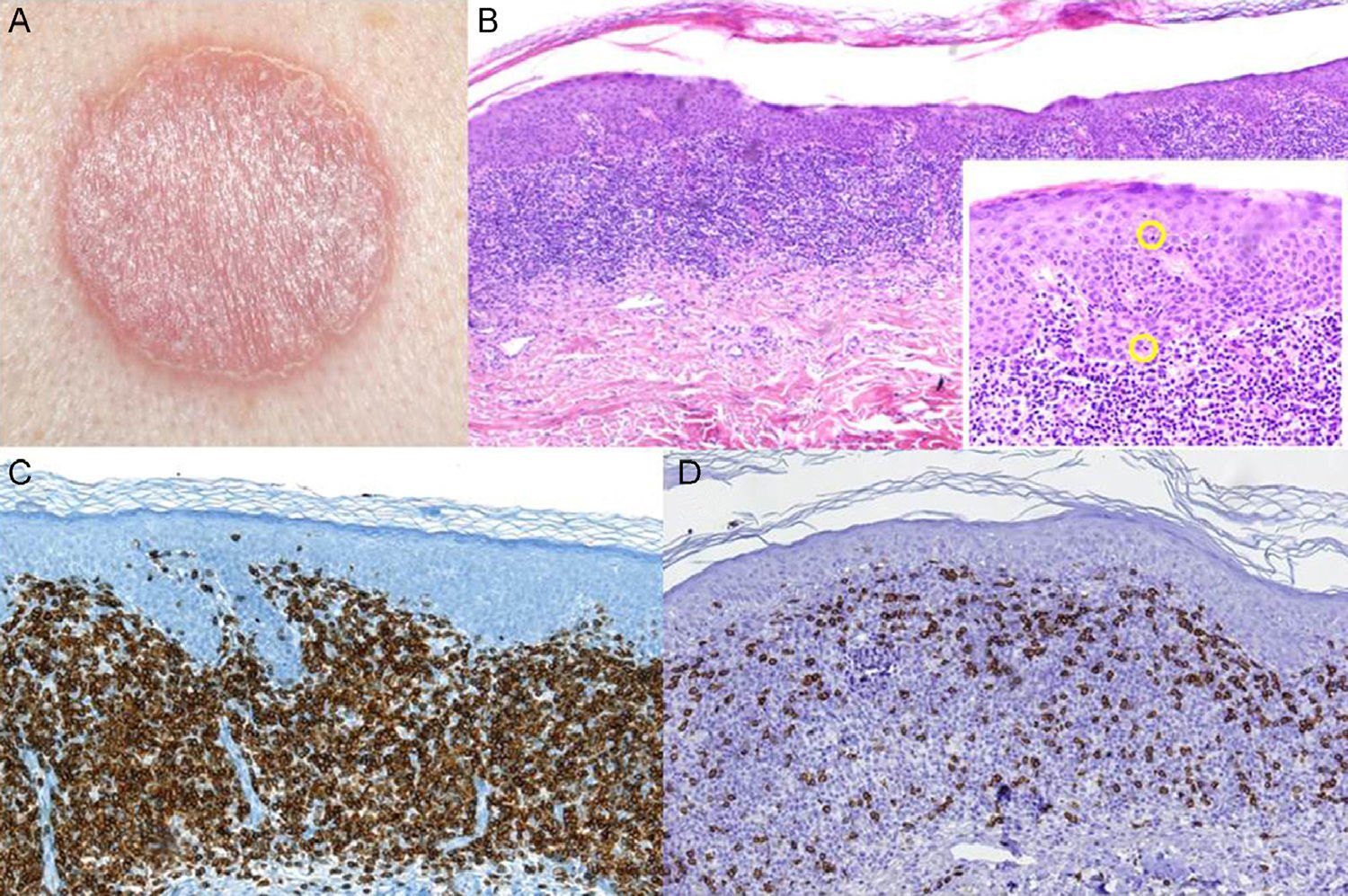
Skin biopsy showed a prominent band-like lymphocytic infiltrate with atypical cells exhibiting marked epidermotropism. Immunohistochemical staining was positive for CD4+ lymphocytes. Gene rearrangement analysis identified monoclonal populations of T-cell receptor (TCR) γ and TCRβ. Analysis of tumor spread by laboratory tests, flow cytometry, and chest x-ray was negative. After diagnosis of unilesional MF it was decided to treat the patient with topical steroids (0.05% clobetasol propionate ointment 2 times per day for 2 months) and phototherapy. Follow-up over 16 months revealed postinflammatory hyperpigmentation with no signs of recurrence (Fig. 1).
A, Erythematous plaque in the interscapular region. B, Skin biopsy revealed a band-like lymphocytic infiltrate with clear epidermotropism (hematoxylin-eosin, original magnification ×4). Lymphocytes with halos can be seen permeating the epidermis (hematoxylin eosin, original magnification ×20). C and D, Immunohistochemical staining demonstrating the predominance of CD4+ T lymphocytes.
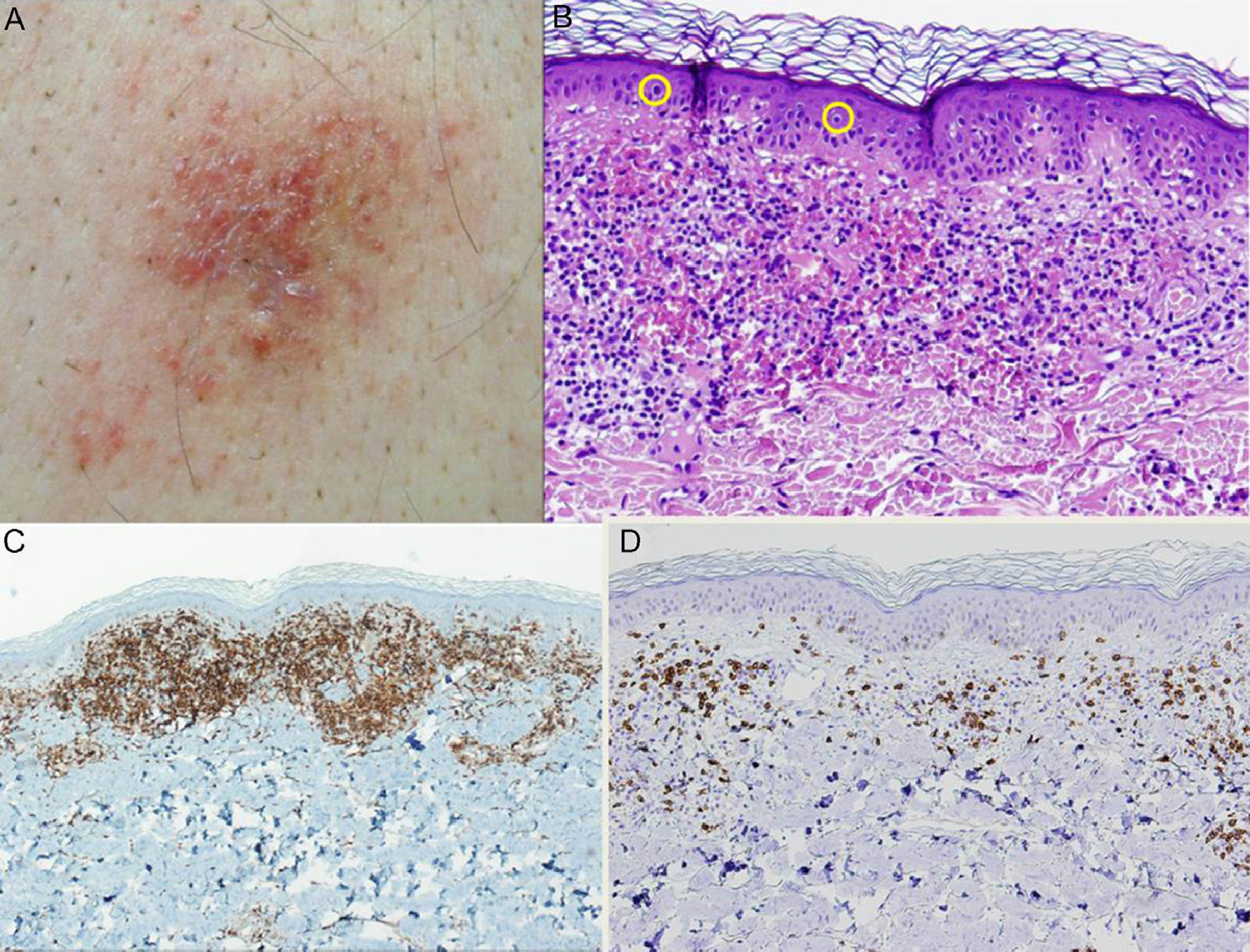
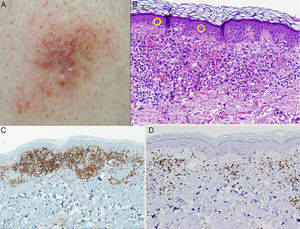
The second patient was a 60-year-old man who was being treated for hypertension with valsartan. The patient presented with an asymptomatic, purpuric plaque measuring 2 × 3cm that had been present in the lumbosacral region for over a year. Skin biopsy showed an atypical lymphocytic infiltrate that was arranged in a band beneath an orthokeratotic epidermis and mixed with abundant extravasated erythrocytes. The infiltrate was clearly epidermotropic; numerous lymphocytes with halos were observed permeating the epidermis. These lymphocytes were identified by immunohistochemistry as CD4+; no loss of other T-cell markers (CD3+, CD5+, CD7+) was observed. As in the previous case, analysis of tumor spread was negative. The patient was diagnosed with unilesional purpuric MF. Clonality analysis was not performed. The patient was prescribed local treatment with 0.05% clobetasol propionate ointment daily for 2 months with subsequent clinical follow-up. The lesion resolved completely with no recurrence detected during 12 months of follow-up (Fig. 2).
A, Purpuric plaque in the lumbrosacral region. B, Staining with hematoxylin-eosin (original magnification ×20) showed significant erythrocyte extravasation and numerous lymphocytes with halos in the epidermis. C, Predominance of CD4+ lymphocytes in the inflammatory infiltrate (original magnification ×10). D, Note the scarcity of CD8+ lymphocytes (original magnification ×10).
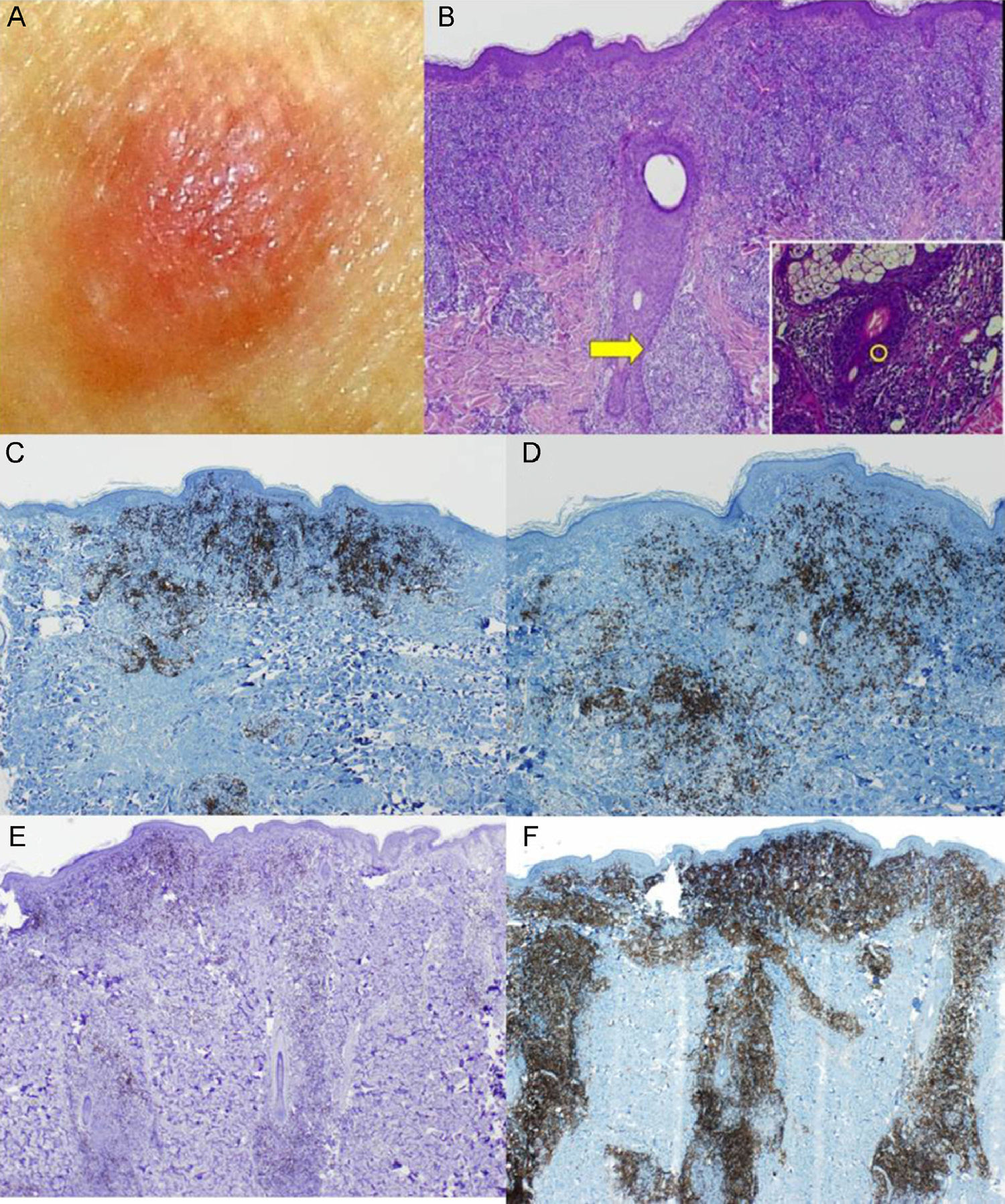
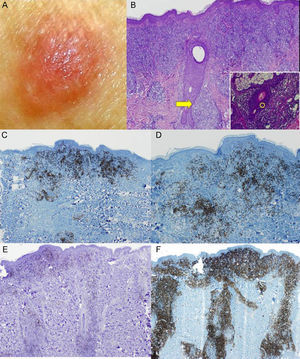
The third patient was a 53-year-old woman with no relevant past medical history. She consulted for an asymptomatic, fleshy tumor with an elastic consistency on her left shoulder. Skin biopsy revealed an infiltrate of atypical lymphocytes along the dermal-epidermal junction and the follicular epithelium, with epidermotropism and folliculotropism. Immunohistochemistry was positive for CD20 and CD4; no loss of other T-cell markers was detected. Analysis of tumor spread confirmed that the disease was localized. The final diagnosis was follicular unilesional MF with intense B-cell infiltration. Gene rearrangement analysis revealed the presence of monoclonal populations of TCRγ and TCRβ cells. Given the poor prognosis of patients with MF and folliculotropism who are treated with topical therapy, it was decided to excise the lesion with margins. No recurrence was observed during 12 months of follow-up (Fig. 3).
A, Fleshy, skin-colored tumor. B, Biopsy showed an epidermal folliculotropic infiltrate (hematoxylin eosin, original magnification ×4) and lymphocytes permeating the follicle (inset: hematoxylin eosin, original magnification ×40). C and D, Immunohistochemical staining showed abundant B cells (CD20+ and CD79+; original magnification ×4). E and F, The lymphocytic infiltrate was composed almost entirely of CD4+ lymphocytes that surrounded the hair follicles.
We have reported 3 cases of unilesional MF, a condition that is well described in the literature but often overlooked in the clinic due to its unremarkable clinical presentation. It is characterized by a single lesion covering less than 5% of the total body surface area2 and its clinical features are as heterogeneous as those of the classical form; the literature describes purpuric, hypopigmented, follicular, and granulomatous forms, and patches of desquamative erythema, among other manifestations.3 However, its histopathological features are comparable with those of the classical form. Prognosis is excellent due to the low tumor burden; only 2 cases of tumor progression are described in the literature, both involving follicular variants.2
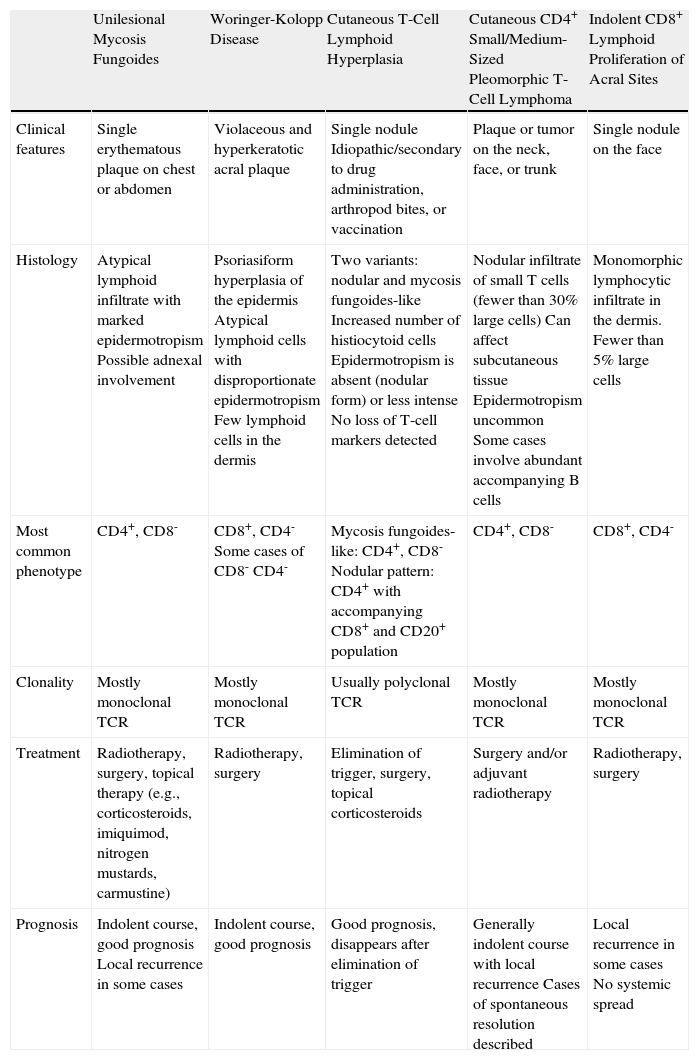
The differential diagnosis should include Kolopp Woringer disease (a variant of MF also known as pagetoid reticulosis), cutaneous lymphoid hyperplasia, cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoma, and the recently described indolent CD8+ lymphoid proliferation of acral sites.4 All are entities that require a close clinicopathologic correlation, and immunohistochemistry is essential (Table 1).
Main Conditions Included in the Differential Diagnoses of Unilesional Mycosis Fungoides.
| Unilesional Mycosis Fungoides | Woringer-Kolopp Disease | Cutaneous T-Cell Lymphoid Hyperplasia | Cutaneous CD4+ Small/Medium-Sized Pleomorphic T-Cell Lymphoma | Indolent CD8+ Lymphoid Proliferation of Acral Sites | |
| Clinical features | Single erythematous plaque on chest or abdomen | Violaceous and hyperkeratotic acral plaque | Single nodule Idiopathic/secondary to drug administration, arthropod bites, or vaccination | Plaque or tumor on the neck, face, or trunk | Single nodule on the face |
| Histology | Atypical lymphoid infiltrate with marked epidermotropism Possible adnexal involvement | Psoriasiform hyperplasia of the epidermis Atypical lymphoid cells with disproportionate epidermotropism Few lymphoid cells in the dermis | Two variants: nodular and mycosis fungoides-like Increased number of histiocytoid cells Epidermotropism is absent (nodular form) or less intense No loss of T-cell markers detected | Nodular infiltrate of small T cells (fewer than 30% large cells) Can affect subcutaneous tissue Epidermotropism uncommon Some cases involve abundant accompanying B cells | Monomorphic lymphocytic infiltrate in the dermis. Fewer than 5% large cells |
| Most common phenotype | CD4+, CD8- | CD8+, CD4- Some cases of CD8- CD4- | Mycosis fungoides-like: CD4+, CD8- Nodular pattern: CD4+ with accompanying CD8+ and CD20+ population | CD4+, CD8- | CD8+, CD4- |
| Clonality | Mostly monoclonal TCR | Mostly monoclonal TCR | Usually polyclonal TCR | Mostly monoclonal TCR | Mostly monoclonal TCR |
| Treatment | Radiotherapy, surgery, topical therapy (e.g., corticosteroids, imiquimod, nitrogen mustards, carmustine) | Radiotherapy, surgery | Elimination of trigger, surgery, topical corticosteroids | Surgery and/or adjuvant radiotherapy | Radiotherapy, surgery |
| Prognosis | Indolent course, good prognosis Local recurrence in some cases | Indolent course, good prognosis | Good prognosis, disappears after elimination of trigger | Generally indolent course with local recurrence Cases of spontaneous resolution described | Local recurrence in some cases No systemic spread |
Abbreviations: TCR, T-cell receptor.
Adapted from Ally et al., 2012.7
In addition to an initial staging examination to rule out minimally symptomatic cutaneous T-cell lymphoma, appropriate clinical follow-up with periodic skin tests is required to assess the possible progression to classic MF.
There are various therapeutic approaches to unilesional MF, all of which target the skin with curative intent. Fractionated radiotherapy is the treatment best supported by the literature, and is well tolerated with few adverse effects.5,6 Surgical excision is a good alternative.7 Topical treatments range from potent corticosteroids to calcineurin inhibitors, imiquimod, carmustine, and nitrogen mustards.
In conclusion, we have presented 3 cases of unilesional MF, a frequently underdiagnosed clinicopathologic entity. Despite the excellent prognosis of this condition, an appropriate tumor staging analysis should be performed and the patient monitored to rule out progression to more extensive forms.
Please cite this article as: Otero Rivas MM, Sánchez Sambucety P, Valladares Narganes LM, Rodríguez Prieto MA. Micosis fungoide unilesional: 3 formas clínicas de presentación. Actas Dermosifiliogr. 2014;105:420–424.