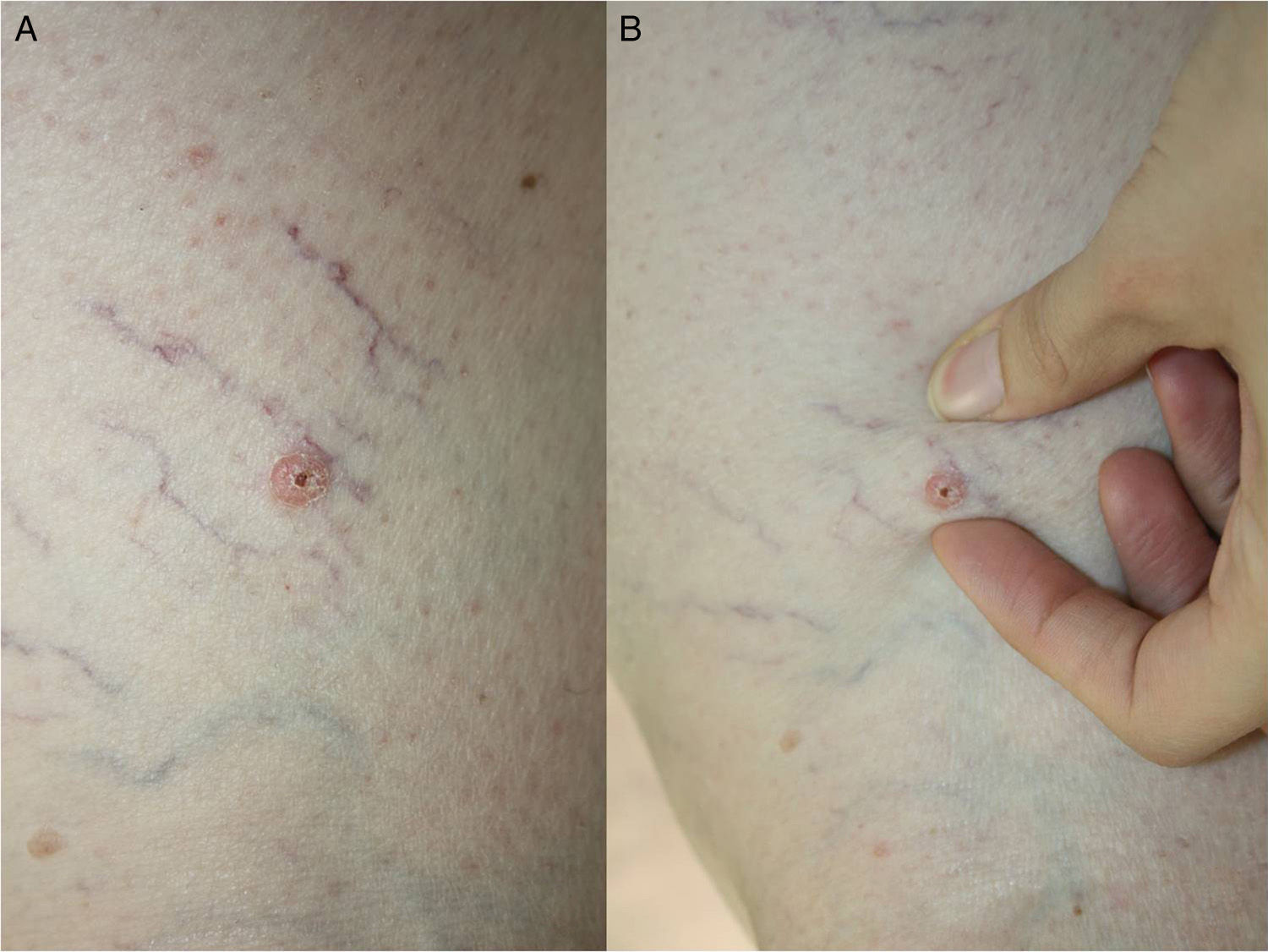
We present the case of a 57-year-old woman with allergy to codeine and a history of osteoporosis, systemic hypertension, allergic rhinitis, and anxiety. She was on treatment with metamizole, enalapril plus hydrochlorothiazide, ebastine, and alprazolam. She consulted for a stable, asymptomatic lesion that had arise approximately 4 years earlier on the right thigh and that had never been treated. Physical examination revealed a 7-mm–diameter, erythematous, desquamating papule with a central blood-stained scab (Fig. 1A) on the lateral surface of the distal right thigh. Deep to the papule was a lesion of rubbery consistency measuring 15mm in diameter (Fig. 1B).
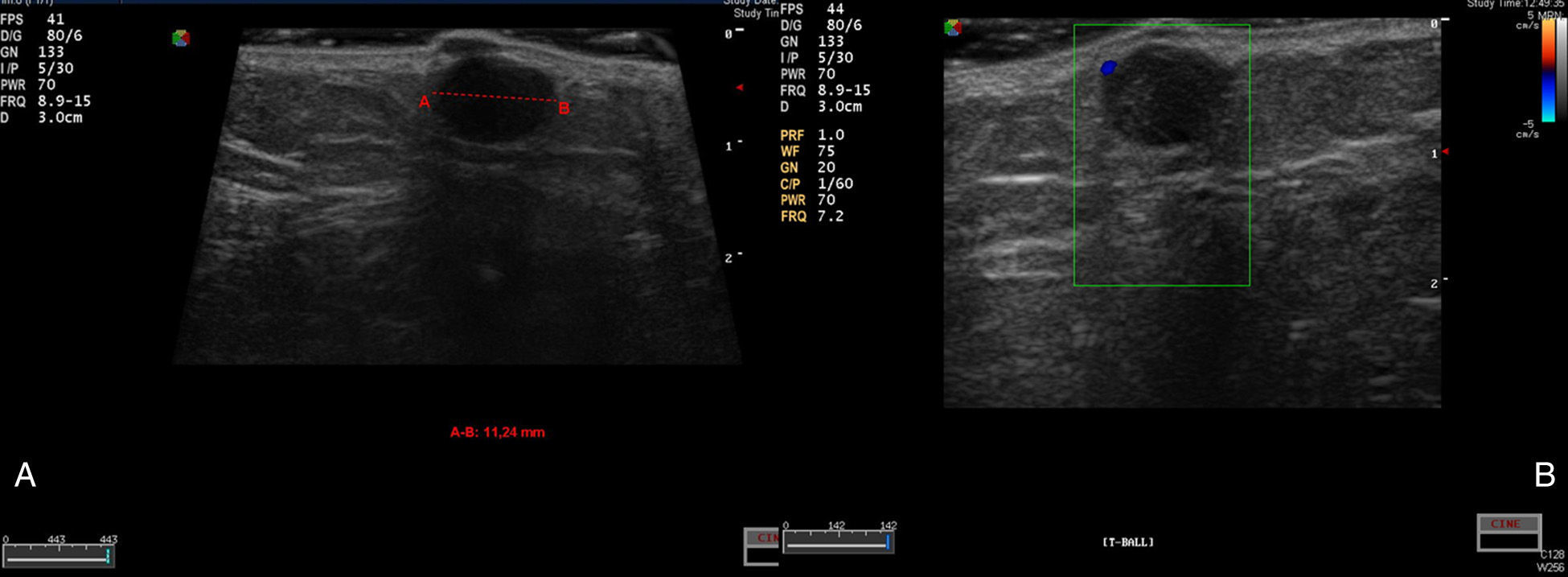
High-frequency skin ultrasound (15MHz) was performed to determine whether this was a single lesion or 2 independent lesions (Fig. 2A). B-mode ultrasound showed a well-defined, hypoechoic lesion in the subcutaneous cellular tissue; the lesion had a cystic appearance with a slightly more echogenic area on its right side. Immediately superficial to this cystic lesion, and in contact with it, was a well-defined, hypoechoic, exophytic dermal lesion. The epidermis was thickened. Doppler examination showed vessels at the periphery of the lesion, but not within it (Fig. 2B). These findings supported the clinical suspicion of a single lesion, and it was excised en bloc.
A, Skin ultrasound shows a well-defined hypoechoic lesion. On the right side of the image there is a more hyperechoic area, which could correspond to the histologic image in Figure3A. The lesion, located in the subcutaneous cellular tissue, had a cystic appearance and measured 11.24mm. It showed posterior acoustic enhancement and oblique lateral shadows. B, Echo Doppler. Blood vessels are visible at the periphery of the lesion, but not within it.
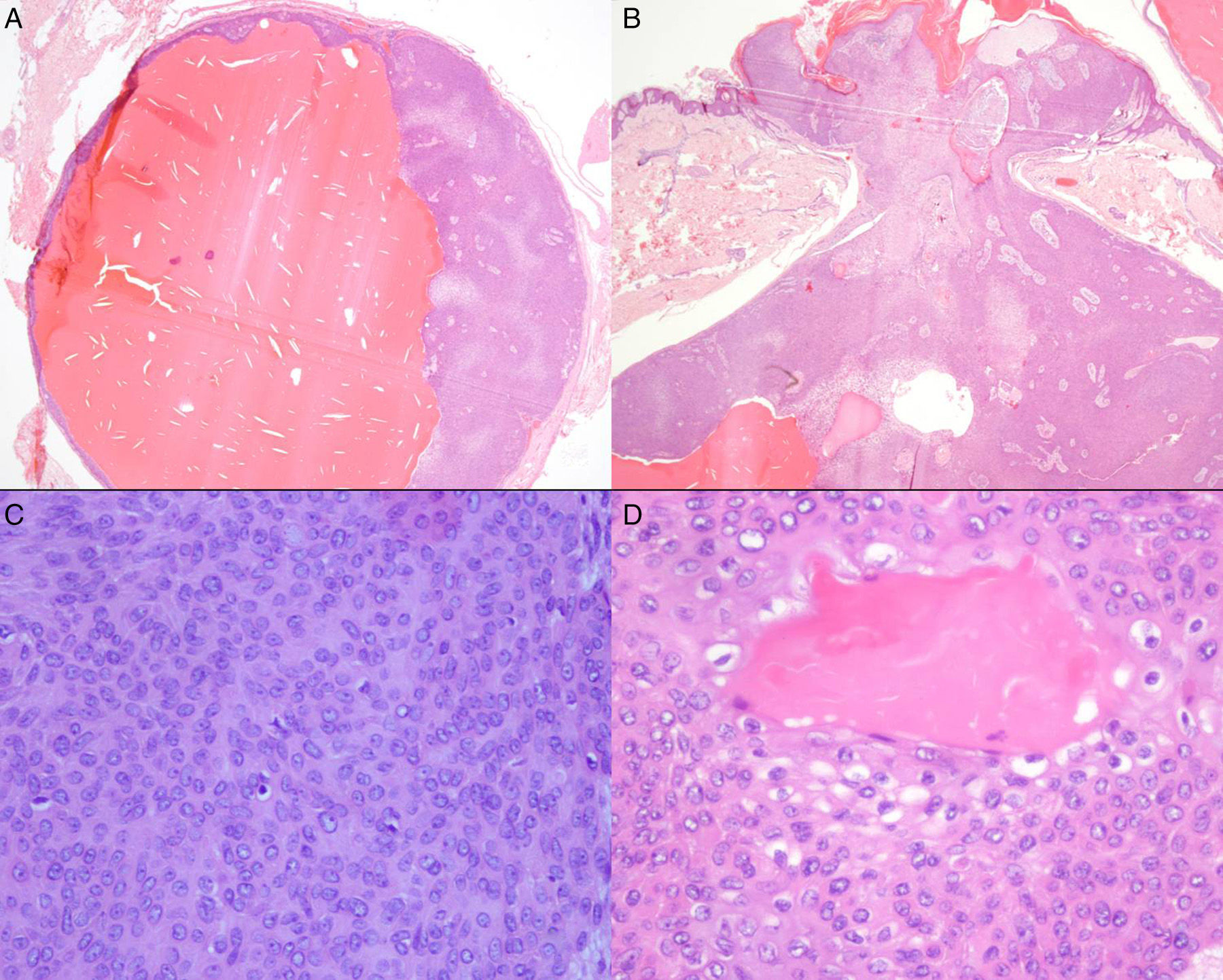
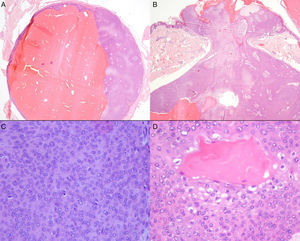
Histopathology showed a mixed solid-cystic, nodular dermal lesion (Fig. 3A) that focally made contact with the epidermis (Fig. 3B). The nodule was formed of poroid cells with round or oval nuclei, small nucleoli, and scant cytoplasm (Fig. 3C). Between the poroid cells were occasional larger cuticular cells that frequently lined ductal lumens (Fig. 3D). There was no evidence of atypia, mitoses, or necrosis. Based on these findings we made a diagnosis of poroid hidradenoma.
Histopathology: A, A solid-cystic lesion in the dermis. Hematoxylin and eosin (H&E), original magnification×20). B, Image showing the focal connection with the overlying epidermis. H&E, original magnification×20). C, Poroid cells with scant cytoplasm, round or oval nuclei, and small nucleoli. H&E, original magnification×400. D, Cuticular cells with abundant eosinophilic cytoplasm lining a duct lumen. H&E, original magnification×400.
Poroid hidradenoma is a variant of eccrine poroma, which belongs to the group of poroid tumors described in 1990 by Abenoza and Ackerman.1 Those authors described the 4 histological variants of eccrine poroma: hidroacanthoma simplex, classic poroma, dermal duct tumor, and poroid hidradenoma, which was the tumor in our patient.
To date, around 50 cases of poroid hidradenoma have been reported. Patient age varies between 13 and 86 years, with a peak in the sixth and seventh decades of life,2,3 and a slight female predominance.
The tumor presents clinically as a solitary lesion, with no preferential anatomic site, though it has not been reported on the palms or soles. Clinical descriptions describe nonspecific cutaneous or subcutaneous lesions, polypoid nodules, or cysts of 1 to 2cm diameter. The lesions are erythematous, reddish, or bluish in color and may be ulcerated.2
Histopathology reveals structural elements of hidradenoma (solid-cystic areas), and cytologic features of poroma (poroid and cuticular cells, the latter cells showing ductal differentiation).4
In the literature reviewed, we have found no reports that describe the skin ultrasound features of poroid hidradenoma or of lesions with a similar appearance, with a cystic component with a more superficial papular component. In our case, ultrasound and histopathology findings were concordant: a cystic lesion connected to the overlying epidermis, suggesting this was a single lesion.
The prognosis is excellent and no cases of malignant change have been reported.
As this is a neoplasm that arises in the dermis,5 the recommended treatment is complete radical excision of the lesion. En bloc surgical excision including the overlying epidermis and the surrounding adipose tissue, as was performed in our patient, prevents recurrence.
The benefit of performing ultrasound in our patient was the correlation between the clinical and histopathological findings: confirmation of the clinical suspicion of a dermal lesion connected to the epidermis and of benign appearance (peripheral vascularization on ultrasound) allowed us to plan en bloc surgical excision without margins.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez-Morán C, Khedaoui R, Echeverría-García B, Borbujo J. Imagen ecográfica del hidroadenoma poroide. Actas Dermosifiliogr. 2016;107:350–352.