Nodular hidradenoma (NH), also known as solid cystic or clear cell hidradenoma, is an uncommon and benign adnexal tumor. Its clinical heterogeneity can lead it to be confused with other neoplasms, both benign and malignant.1 Although the initial diagnosis is based on histopathology findings, a previous skin ultrasound could prove to be of considerable help. We present a case of NH at an unusual site in an elderly woman and in which ultrasound was very useful for diagnosis.
The patient was an 87-year-old woman with a history of arterial hypertension and carcinoma in situ of the larynx in complete remission who consulted for a painful lesion on her lower back. The lesion had grown gradually, and the patient could not remember when it first appeared.
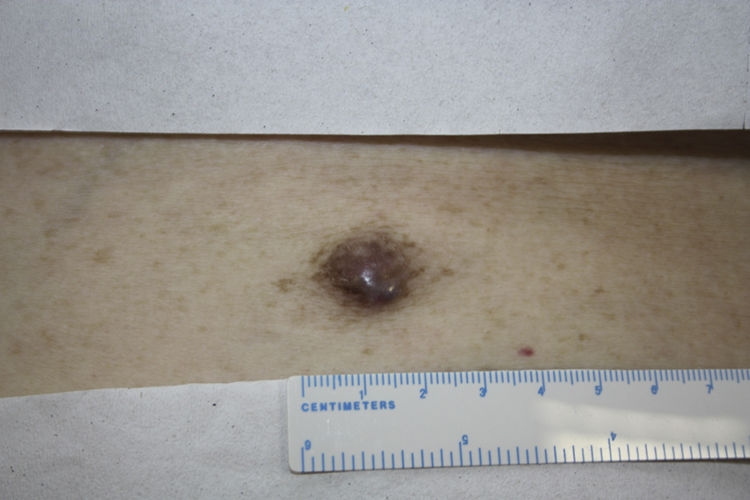
Physical examination revealed a painful subcutaneous lesion measuring 2cm that was erythematous-violaceous in color and of a firm consistency (Fig. 1). The lesion had what appeared to be a dimple sign. The rest of the physical examination was unremarkable.
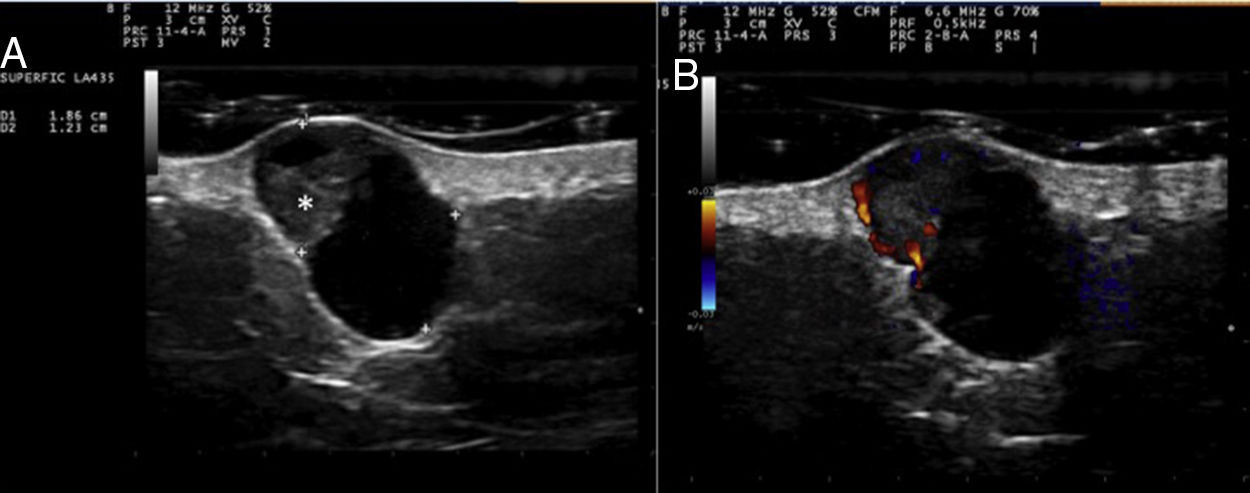
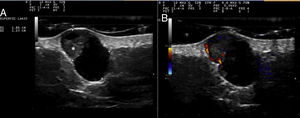
Cutaneous ultrasound (12-18MHz) revealed an oval, well-defined dermal-hypodermal structure measuring 1.85×1.23cm. This lesion was cystic in appearance, with an anechoic interior and posterior enhancement. A triangular hyperechogenic area protruding through the wall was clearly visible in the upper pole (Fig. 2A). Color Doppler mode revealed increased peripheral vascularization, especially in the triangular solid portion (Fig. 2B).
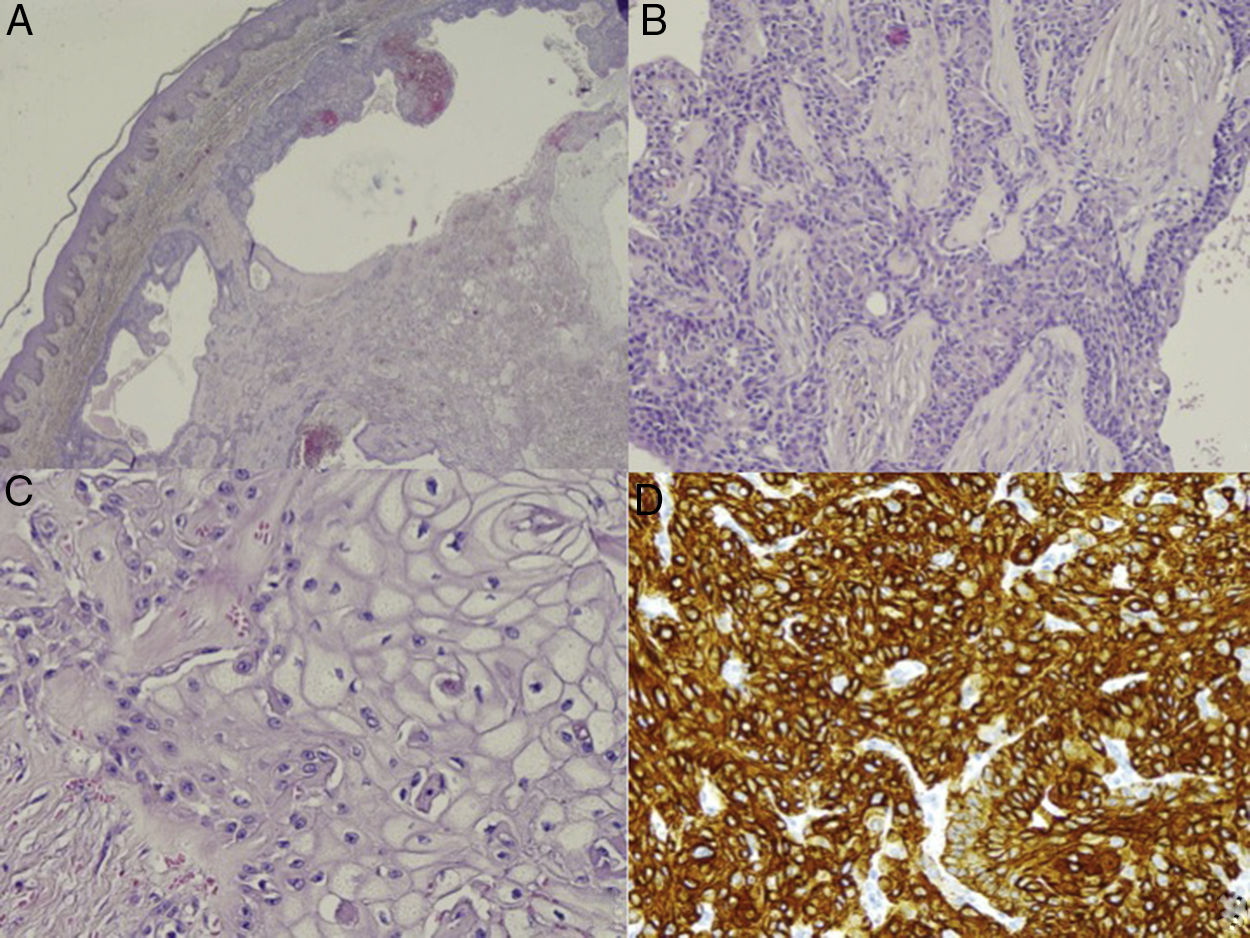
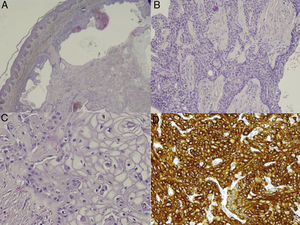
Given the patient's personal history and the fact that the time of onset was unknown, we decided to remove the lesion. Histopathology revealed a well-defined dermal-hypodermal lesion with solid and cystic areas (Fig. 3A). The solid areas were composed of 2 types of cell: cells with a round nuclei, granular chromatin, visible nucleoli, abundant cytoplasm, and eosinophils; and cells with a clear cytoplasm and eccentric nuclei (Fig. 3B-C). There was no cellular atypia, pleomorphism, vascular invasion, or necrosis. Immunohistochemistry revealed positive results for epithelial membrane antigen, cytokeratin (CK) 7, and CK AE1/AE3, and negative results for S100, enolase, melan-A, and D2-40 (Fig. 3D). These findings enabled us to make a diagnosis of NH.
Histopathology. A,Well-defined, nonencapsulated dermal-hypodermal lesion with solid cystic areas (hematoxylin-eosin, original magnification ×10). B and C,Two types of cell can be distinguished in the solid portion of the tumor. Polyhedral cells, with a long vesicular nucleus and eosinophilic cytoplasm (B), and large cells with an eccentric nucleus and abundant clear cytoplasm (C) (hematoxylin-eosin, original magnification, ×20 and ×40). D)Positive immunohistochemistry result for CK-7 (CK-7, ×40).
NH mainly affects women in the fourth and fifth decades of life. It is found on the head and upper limbs. Clinically, it is characterized by a slow-growing, solitary, round lesion measuring 0.5-2cm with a firm consistency. It is usually asymptomatic, although it sometimes bleeds or is painful, as in the case we report. The overlying skin may be thickened, atrophic, or ulcerated and is erythematous-violaceous or brownish in color.1,2
Although NH has traditionally been considered a neoplasm with eccrine differentiation, it is nowadays classified into 2 groups: hidradenoma with eccrine differentiation (poroid hidradenoma) and hidradenoma with apocrine differentiation (NH).1
Few publications report ultrasound findings for NH, although these findings are similar in all of the reports.2–7 In ultrasound terms, NH is defined as a well-demarcated, oval, dermal-hypodermal cystic lesion that has an anechoic or hypoechoic interior. In 7 of the 8 cases reported, the interior of the lesion contains a solid triangular hyperechoic area that protrudes from the wall of the lesion and that usually shows increased vascularization on Doppler.2–7 These ultrasound findings are associated with the solid cystic areas observed in histopathology. Hyperechogenic foci compatible with calcifications can sometimes be observed.4
The clinical differential diagnosis includes dermatofibroma, epidermal cyst, blue nevus, and basal cell carcinoma; the main histopathologic differential diagnosis is with apocrine mixed tumor.1
In ultrasound, the differential diagnosis should be made first with other benign adnexal tumors, such as the following: hidrocistoma,8 a hypoechoic dermal-hypodermal lesion with no posterior enhancement or vascularization; eccrine spiradenoma,9 a heteroechoic lobulated dermal lesion with posterior enhancement and vascularization (both central and peripheral); and poroid hidradenoma,10 a hypoechoic hypodermal lesion with hyperechogenic areas, posterior enhancement, and a lateral acoustic shadow.
Other benign subcutaneous lesions that should also be ruled out include the following: epidermal cyst, a hypoechoic lesion with posterior enhancement, lateral acoustic shadow, and dermal-hypodermal tract or punctum; pilomatrixoma, a well-defined heteroechoic lesion that usually presents peripheral vascularization and calcifications in the interior; dermatofibroma, a poorly defined dermal-hypodermal lesion with no vascularization and that could present hypoechoic lines on the periphery. Finally, given the history of cancer, we should rule out cutaneous metastasis, which is characterized on ultrasound as intensely vascularized and as hypoechoic nodules with increased acoustic transmission in the subcutaneous cellular tissue.11
Despite being a benign neoplasm, NH usually recurs after incomplete removal. There have been reports of isolated cases of malignant transformation, which should be suspected in the case of a rapidly growing tumor with an invasive pattern, pleomorphism, high mitotic index, and angiolymphatic invasion in histopathology.
Therefore, NH may prove difficult to differentiate clinically from other skin lesions. Application of a rapid, inexpensive, noninvasive technique such as cutaneous ultrasound can guide the presurgical diagnosis of NH. The presence of a cystic anechoic lesion with a vascularized hyperechogenic triangular area protruding through the wall are ultrasound findings that should point us to a diagnosis of NH.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vázquez-Osorio I, Gonzalvo-Rodríguez P, Rodríguez-Díaz E. Diagnóstico ecográfico del hidradenoma nodular. Actas Dermosifiliogr. 2018;109:453–455.