Digital dermoscopy (DD) has been found to improve the accuracy of melanoma diagnosis in high-risk patients. A 2-step approach combining DD and total-body photography (TBP) can facilitate the detection of new lesions or early macroscopic changes in existing lesions.
ObjectivesThe aim of this study was to determine the number of biopsies needed to diagnose melanoma and to describe the clinical and dermoscopic characteristics of melanoma diagnosed in patients with pigmented lesions under follow-up with DD and TBP.
Patients and methodsRetrospective study of 152 patients with a high risk of melanoma who were followed using a 2-step digital approach at Hospital del Mar in Barcelona, Spain, between 2002 and 2016. We analyzed the characteristics of pigmented lesions excised after macroscopic changes were detected by periodic DD and TBD.
ResultsBiopsy results of 99 lesions (84 dysplastic nevi, 13 melanomas, and 2 compound melanocytic nevi) showed a ratio of benign melanocytic lesions to melanomas of 1:6.6. The mean Breslow thickness was 0.19mm. Macroscopic changes were significantly more common in melanomas than in melanocytic nevi (P = .018). Dermoscopic findings associated with melanoma were asymmetric growth and focal structural changes (P < .001). The specific features associated with a diagnosis of melanoma were asymmetry (P < .001), a reverse pigment network (P = .011), atypical globules (P = .011), and polymorphous vessels (P = .045).
ConclusionsTBP follow-up is a useful tool for the early diagnosis of melanoma. In our series, 50% of melanomas diagnosed during digital follow-up were detected by observation of a new lesion via TBP mapping or macroscopic changes in an existing lesion. Dermoscopic follow-up is essential in patients at high risk for melanoma as both melanocytic nevi and melanoma show a range of specific dermoscopic features, and a diagnosis of melanoma can only be based on a record of changes in the appearance of lesions during follow-up.
La dermatoscopia digitalizada (DD) ha demostrado mejorar la precisión en el diagnóstico del melanoma (MM) en pacientes de alto riesgo. La combinación de DD y fotografía corporal total (FCT) puede facilitar la detección de nuevas lesiones o la aparición de cambios macroscópicos precoces en lesiones previamente registradas.
ObjetivosEl objetivo del presente estudio fue determinar el número de biopsias necesarias para diagnosticar un MM y, las características clínicas y dermatoscópicas asociadas al diagnóstico de melanoma en pacientes en seguimiento, mediante DD y FCT, de lesiones pigmentadas.
Pacientes y MétodosSe realizó un estudio retrospectivo de 152 pacientes con elevado riesgo de sufrir MM, en seguimiento digitalizado entre 2002 y 2016, en el Hospital del Mar de Barcelona. Se estudiaron y analizaron las lesiones pigmentadas extirpadas a partir de los cambios observados tras controles periódicos con DD y FCT.
ResultadosSe analizaron un total de 99 biopsias (84 nevus displásicos, 13MM, 2 nevus melanocíticos junturales/compuestos) con una ratio lesión melanocítica benigna: MM de 6,6. El índice Breslow promedio fue de 0,19mm. Las lesiones malignas presentaron con mayor frecuencia cambios macroscópicos respecto a los nevus melanocíticos (p=0,018). En el análisis dermatoscópico, el crecimiento asimétrico y los cambios focales en estructuras se asociaron a MM (p<0,001). Los parámetros de dermatoscopia individuales relacionados con el diagnóstico de MM fueron la asimetría ((p<0,001), retículo pigmentado invertido (p=0,011), glóbulos atípicos (p=0,011) y vasos polimorfos (p=0,045).
ConclusionesEl seguimiento mediante FCT resulta una herramienta útil en el diagnóstico precoz de MM. Un 50% de los melanomas detectados mediante el seguimiento digitalizado se diagnosticaron por la aparición de una lesión nueva en los mapas corporales o por la detección de cambios macroscópicos de una lesión preexistente. El seguimiento dermatoscópico resulta fundamental, ya que un elevado número de hallazgos dermatoscópicos individuales pueden observarse tanto en nevus melanocíticos como en un melanoma maligno, y el diagnóstico de malignidad sólo se puede establecer a partir de los cambios en el registro de dermatoscopia durante el seguimiento.
Early diagnosis is the most effective intervention in improving the outcome of patients with malignant melanoma (MM). The distinction between MM and different benign pigmented lesions can be a challenge for specialists, as they may occasionally show similar clinical and dermoscopic findings.1 Digital follow-up of melanocytic lesions by means of digital dermoscopy (DD) devices makes it possible to detect subtle changes that are not clinically obvious. This method makes it possible to identify early-stage melanoma without the more specific macroscopic characteristics of malignant lesions.2–4 Photographic monitoring of different body regions (total body photography, TBP) facilitates the identification of new lesions and the detection of changes in previously identified lesions by comparing current images with those taken previously.5,6
Patients with multiple melanocytic nevi and with a high risk of MM are a particularly complex group in which to diagnose malignant melanocytic lesions. In this group, 2-step digital follow-up combining TBP and DD allows for a more specific diagnosis than by using each of the 2 strategies separately.7 This 2-step follow-up is a more sensitive screening strategy, as it makes it possible to identify both dermoscopic and macroscopic changes and to detect the appearance of new, previously unidentified lesions.
The main objective of this study is to determine the number of biopsies required to diagnose MM in high-risk patients in follow-up with TBP and DD. A secondary objective was to define the clinical and dermoscopic characteristics that led to excision of the lesions and to identify the distinctive traits of MM compared to benign melanocytic lesions.
Patients and MethodsWe reviewed the images of the patients in digital follow-up (TBP and DD) of pigmented lesions from consultations for pigmented lesions in the dermatology department of Hospital del Mar, Barcelona, and who had been enrolled in the program from March 2002 to March 2016. The program enrols patients with more than 50 melanocytic nevi and at least 1 risk factor for developing melanoma (personal and/or family history of MM, major actinic damage, or Fitzpatrick skin type I or II). Of these patients, we selected those with more than 50 melanocytic nevi, whose follow-up images met the following criteria: a) at least 4 anatomical areas recorded, one of which is the back, and b) at least 2 follow-up images using DD and TBP.
The images were obtained using the Molemax (Derma Medical, Vienna, Austria) standardized digital system for follow-up of pigmented lesions. Macroscopic images were taken of all anatomical body areas (front, back, and sides) and of the clinically and/or dermoscopically atypical lesions. Those lesions suspected to be malignant due to clinical or dermoscopic changes were excised to perform a histopathology study, as per the standard clinical-practice protocol.
The patients’ clinical data included in the study were obtained from their medical records. We recorded epidemiologic characteristics (sex, age, personal and family past history of melanoma), clinical characteristics (Fitzpatrick skin type, number of lesions, number of images recorded per patient, and follow-up time), and number of biopsies performed in each patient. Clinical changes (new lesion, changes in growth and in pigmentation) and dermoscopic changes (growth, focal changes in pigmentation, structure, and regression structures) in the lesions that had been excised during follow-up and that led to excision were analyzed retrospectively. Furthermore, the number of colors, symmetry, number of dermoscopic structures, total dermoscopy score (TDS), 7-point checklist, and location, size, and Breslow index were recorded in cases of MM. The following findings were recorded from the dermoscopic perspective: atypical reticulum, inverted reticulum, polymorphous vessels, atypical globules, blotches, and pseudopods.
Clinical and epidemiological variables were determined by 2 independent observers. The dermoscopic variables and clinical and dermoscopic changes in the lesions were recorded by 2 observers by common agreement.
Version 21 of the IBM SPSS statistical package was used to perform the statistical analysis. The X2 test was used to compare qualitative variables and Fisher’s exact test was applied to the x2 tables. The t test for independent samples was used to compare quantitative variables (age, number of images recorded, nevi per patient, and follow-up time). The Mann-Whitney U test was used for the quantitative variables TDS and 7-point checklist, as the distribution was non-normal. Differences were considered statistically significant for values of P<.05.
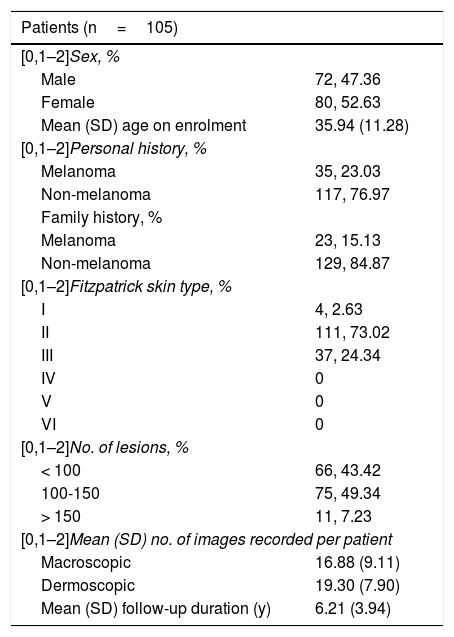
ResultsA total of 152 patients were studied, with a mean (SD) age of 36 (11.28) years on enrolment in the study; 47.36% of the patients were men. Of all the patients, 35 (23.03%) reported a personal history and 23 (15.13%) a family history of melanoma on enrolment in the study. Of the patients enrolled, 73.02% had Fitzpatrick skin type II, 24.34% had Fitzpatrick skin type III, and 2.63% had Fitzpatrick skin type I. With regard to the number of lesions, 56.57% had > 100 melanocytic nevi and 43.42% had < 100. A total of 2566 body images (16.88 [9.11] per patient) and 2934 dermoscopic images (19.30 [7.90] per patient) were recorded. The mean follow-up per patient was 6.2 (3.94) months. Of all the enrolled patients, 10 (15.2%) developed a melanoma during follow-up and, of these, half of cases (3.2%) were a second melanoma (Table 1).
Descriptive Data of the Patients in Follow-Up
| Patients (n=105) | |
|---|---|
| [0,1–2]Sex, % | |
| Male | 72, 47.36 |
| Female | 80, 52.63 |
| Mean (SD) age on enrolment | 35.94 (11.28) |
| [0,1–2]Personal history, % | |
| Melanoma | 35, 23.03 |
| Non-melanoma | 117, 76.97 |
| Family history, % | |
| Melanoma | 23, 15.13 |
| Non-melanoma | 129, 84.87 |
| [0,1–2]Fitzpatrick skin type, % | |
| I | 4, 2.63 |
| II | 111, 73.02 |
| III | 37, 24.34 |
| IV | 0 |
| V | 0 |
| VI | 0 |
| [0,1–2]No. of lesions, % | |
| < 100 | 66, 43.42 |
| 100-150 | 75, 49.34 |
| > 150 | 11, 7.23 |
| [0,1–2]Mean (SD) no. of images recorded per patient | |
| Macroscopic | 16.88 (9.11) |
| Dermoscopic | 19.30 (7.90) |
| Mean (SD) follow-up duration (y) | 6.21 (3.94) |
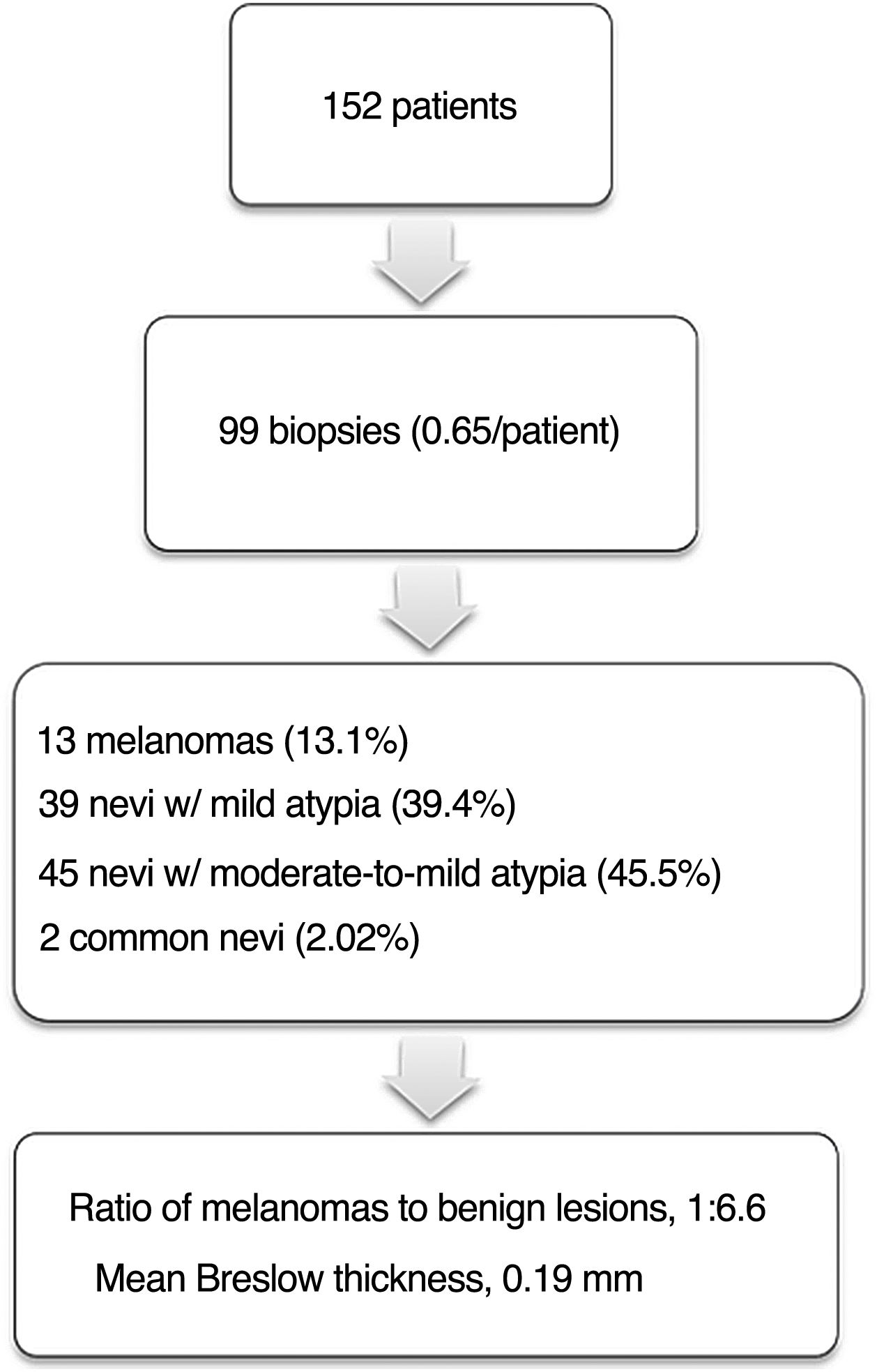
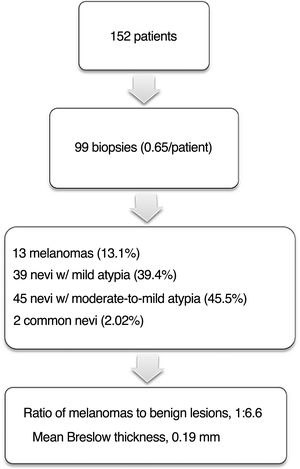
A total of 99 biopsies were performed during follow-up, with a mean of 0.65 biopsies per patient. Of all the excisions, 13 (13.3%) were MM, 39 (39.8%) were melanocytic nevi with mild atypia, 45 (45.5%) were melanocytic nevi with moderate-to-severe atypia, and 2 (2.0%) were conventional compound melanocytic nevi. With regard to the 13 melanomas, the mean Breslow thickness was 0.19mm and the mean (SD) time to diagnosis was 4.7 (3.7) years. In the cohort studied, the ratio of MM to benign excised lesion was 1:6.61 (Fig. 1).
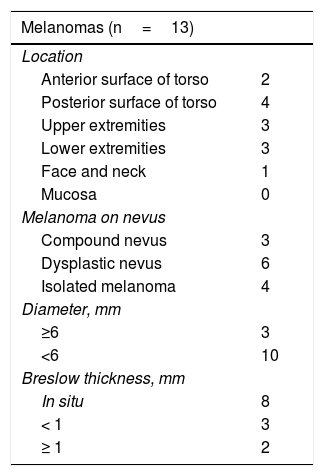
Of the 13MM diagnosed, 6 were located on the torso, 3 on the upper extremities, 3 on the lower extremities, and 1 on the face. The mean (SD) size of the melanomas was 6.15 (2.45) mm. Histopathology showed that 9MM had developed on a melanocytic nevus (3 on a compound melanocytic nevus and 6 on a dysplastic nevus), whereas 4 were de novo melanomas. Of these melanomas, 8 were in situ MM and 5 were invasive, 3 of which had a Breslow thickness of > 0.8mm (Table 2).
Descriptive Characteristics of Excised Melanomas
| Melanomas (n=13) | |
|---|---|
| Location | |
| Anterior surface of torso | 2 |
| Posterior surface of torso | 4 |
| Upper extremities | 3 |
| Lower extremities | 3 |
| Face and neck | 1 |
| Mucosa | 0 |
| Melanoma on nevus | |
| Compound nevus | 3 |
| Dysplastic nevus | 6 |
| Isolated melanoma | 4 |
| Diameter, mm | |
| ≥6 | 3 |
| <6 | 10 |
| Breslow thickness, mm | |
| In situ | 8 |
| < 1 | 3 |
| ≥ 1 | 2 |
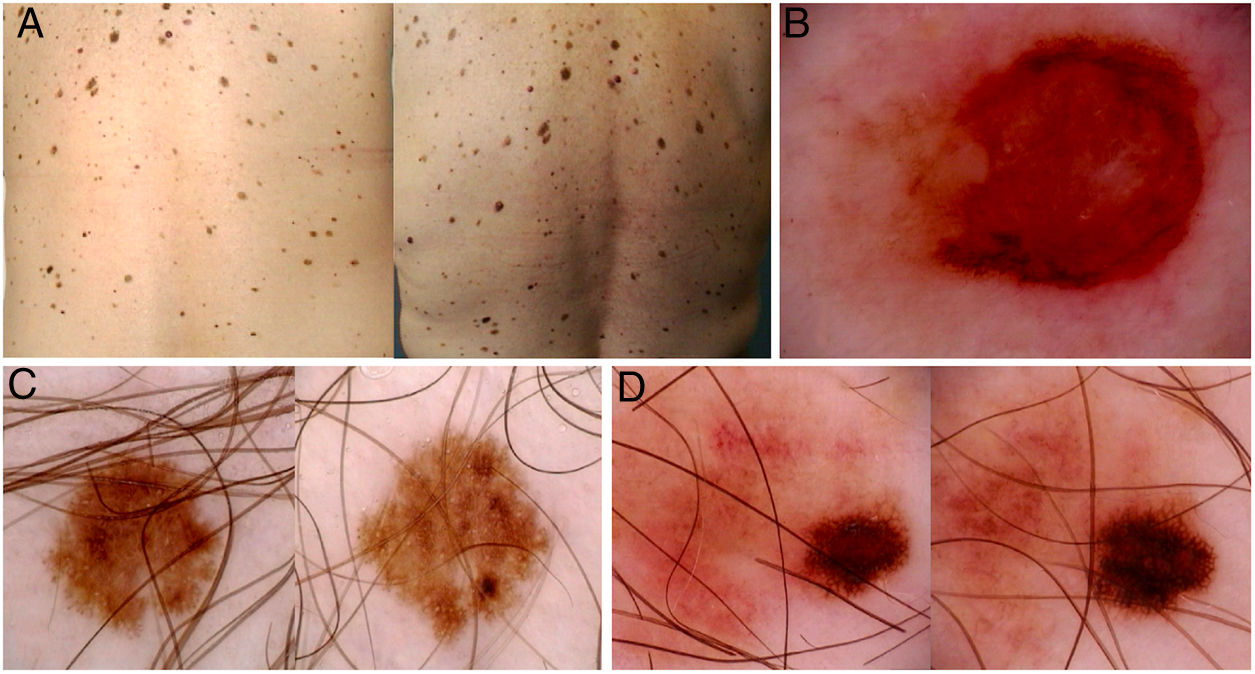
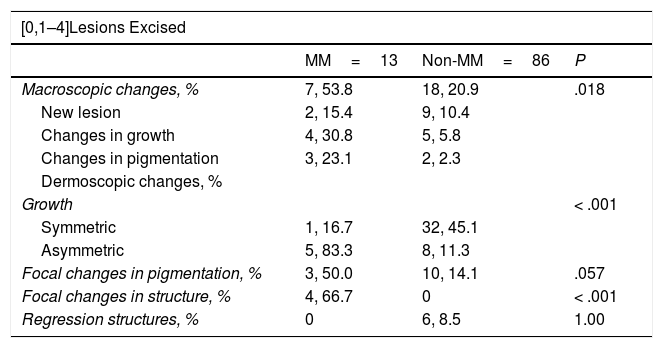
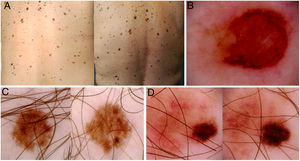
All of the melanomas were excised due to changes during digital follow-up. Seven MM were excised because changes had been detected in the body images (appearance of a new lesion or growth of a pre-existing lesion), whereas in the remaining 6MM, excision was performed due to changes in the dermoscopic image. The most common dermoscopic change was asymmetric growth (5 cases), followed by focal changes in pigmentation (3 cases) and focal changes in structure (3 cases) (Table 3). The melanomas showed changes in the macroscopic images more frequently than the melanocytic nevi (P=.018), and a greater proportion were palpable (P<.007) (Table 4) (Fig. 2). In the dermoscopy analysis, asymmetric growth and focal changes in structure were associated with a diagnosis of MM (P<.001), whereas no statistically significant differences were found with respect to focal changes in pigmentation and the presence of regression structures (P=.057 and P=1.0, respectively) (Table 3) (Fig. 2).
Macroscopic Changes and Growth
| [0,1–4]Lesions Excised | |||
|---|---|---|---|
| MM=13 | Non-MM=86 | P | |
| Macroscopic changes, % | 7, 53.8 | 18, 20.9 | .018 |
| New lesion | 2, 15.4 | 9, 10.4 | |
| Changes in growth | 4, 30.8 | 5, 5.8 | |
| Changes in pigmentation | 3, 23.1 | 2, 2.3 | |
| Dermoscopic changes, % | |||
| Growth | < .001 | ||
| Symmetric | 1, 16.7 | 32, 45.1 | |
| Asymmetric | 5, 83.3 | 8, 11.3 | |
| Focal changes in pigmentation, % | 3, 50.0 | 10, 14.1 | .057 |
| Focal changes in structure, % | 4, 66.7 | 0 | < .001 |
| Regression structures, % | 0 | 6, 8.5 | 1.00 |
Abbreviation: MM indicates melanoma.
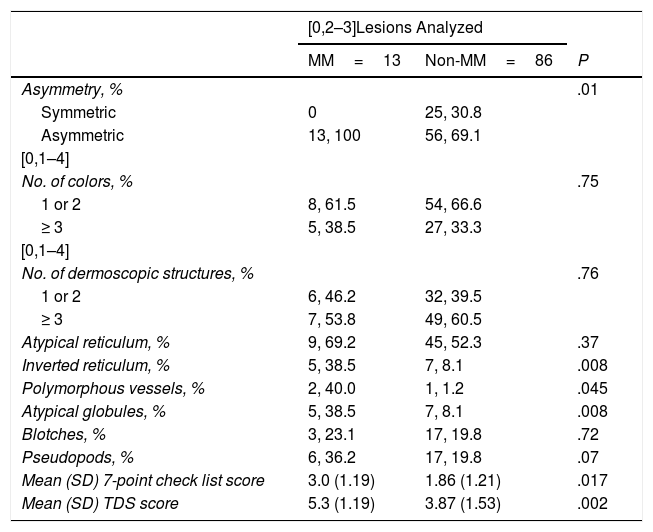
Asymmetry, Number of Colors, and Number of Dermoscopic Structures
| [0,2–3]Lesions Analyzed | |||
|---|---|---|---|
| MM=13 | Non-MM=86 | P | |
| Asymmetry, % | .01 | ||
| Symmetric | 0 | 25, 30.8 | |
| Asymmetric | 13, 100 | 56, 69.1 | |
| [0,1–4] | |||
| No. of colors, % | .75 | ||
| 1 or 2 | 8, 61.5 | 54, 66.6 | |
| ≥ 3 | 5, 38.5 | 27, 33.3 | |
| [0,1–4] | |||
| No. of dermoscopic structures, % | .76 | ||
| 1 or 2 | 6, 46.2 | 32, 39.5 | |
| ≥ 3 | 7, 53.8 | 49, 60.5 | |
| Atypical reticulum, % | 9, 69.2 | 45, 52.3 | .37 |
| Inverted reticulum, % | 5, 38.5 | 7, 8.1 | .008 |
| Polymorphous vessels, % | 2, 40.0 | 1, 1.2 | .045 |
| Atypical globules, % | 5, 38.5 | 7, 8.1 | .008 |
| Blotches, % | 3, 23.1 | 17, 19.8 | .72 |
| Pseudopods, % | 6, 36.2 | 17, 19.8 | .07 |
| Mean (SD) 7-point check list score | 3.0 (1.19) | 1.86 (1.21) | .017 |
| Mean (SD) TDS score | 5.3 (1.19) | 3.87 (1.53) | .002 |
Abbreviations: TDS indicates total dermoscopy score; MM, melanoma.
Images of total body maps and dermoscopy images of 3 patients enrolled in the study. A, Appearance of a palpable de novo pigmented lesion in the left lumbar region (circle). B, Dermoscopy of the lesion, showing structural asymmetry, polychromatic appearance, atypical reticulum, and central area with no structure. Histopathology showed a melanoma with a Breslow thickness of 1.4mm. C and D, In situ melanomas diagnosed due to dermoscopic changes in digital follow-up (asymmetric growth, focal changes in pigmentation, focal changes in structure).
With regard to the dermoscopic characteristics of the melanomas, the 13MM presented at least 1 axis of asymmetry and 2 or more colors (8MM≥3 colors). In terms of dermoscopic structures, all cases, with the exception of 1 melanoma, presented at least 2 dermoscopic structures, the most common of which was a multicomponent pattern (3 or more structures) (7 cases). The most common dermoscopic structure was atypical pigmented reticulum (9 cases), followed by pseudopods (6 cases), inverted reticulum (5 cases), atypical globules (5 cases), pigment blotches (3 cases), and atypical vascularization and polymorphous vessels (2 cases). Asymmetry (P=.01), inverted pigmented reticulum (P=.008), atypical globules (P=.008), and polymorphous vessels (P=.045) were associated with MM if compared with melanocytic nevi. According to the TDS, 3 of the MM were benign, 8 malignant, and 2 suspicious lesions. According to the 7-point checklist, 7 were classified as malignant and 6 benign. The mean TDS was 3.9 and 5.3 in melanocytic nevi and melanomas, respectively (P=.003), whereas the mean score on the 7-point checklist was 1.86 and 3.0 (P=.017) (Table 4).
DiscussionTwo-step follow-up combining DD and TBP is indicated in patients with a high risk of developing MM. This strategy makes it possible to detect dermoscopic and macroscopic changes and the appearance of new lesions, and increases the accuracy of diagnosis, thereby reducing excision of benign lesions.6,8–10
In this study, the predominant Fitzpatrick skin type of the patients was II (73.02%) and III (24.34%), which contrasts with the most common Fitzpatrick skin types in our setting, where III is the most common.11 This may be explained by the inclusion in the study only of patients with a high risk of developing melanoma. Moreover, Fitzpatrick skin type I or II is a factor for inclusion in the digital follow-up program, thus leading to inclusion bias.
In our study, less than 1 lesion per patient was excised during a mean follow-up period of 6.2 years. The ratio of MM to benign melanocytic lesions was 1:6.61, with a rate of 13.30% of MM diagnosed out of all the excised lesions. In the study by Salerni et al,8 2-step digital follow-up showed a ratio of MM to benign lesions of 1:10.7. In other studies, in which follow-up was exclusively by means of DD, the ratios were 1:15.5,12 1:8.5,13 and 1:53.14 Although a tendency toward improvement of the ratio of MM to benign melanocytic lesions appears to exist with the 2-step follow-up of melanocytic lesions, the heterogeneity in terms of the patients enrolled in the study makes it difficult to compare the different series.
Digital follow-up of patients at high risk of developing MM not only makes it possible to increase accuracy in the diagnosis of malignant pigmented lesions but also facilitates early diagnosis.15 In the studies by Haenssle et al13 and Salerni et al,16 the mean Breslow thicknesses of the MM diagnosed by means of dermoscopic follow-up were 0.43mm and 0.52mm, respectively. In our study, the mean Breslow thickness was 0.19mm, which appears to indicate earlier detection and diagnosis of MM using the 2-step method combining DD and TBP.
A study carried out by Argenziano et al9 found that MM can grow slowly over time, thus requiring follow-up for long periods. In our patients, the mean time to diagnosis of MM was 4.7 years, which justifies continuous long-term follow-up of patients deemed to be high-risk.
Histopathology revealed that 69.2% of MM were associated with a pre-existing proliferation of nevus cells. This finding contrasts with different studies that found that only 30% of melanomas developed on a melanocytic nevus.17 Patients with many clinically atypical nevi or dysplastic nevi, such as those in our study, may have a greater predisposition to developing MM not only on previously existing melanocytic lesions but also de novo MM.
Follow-up by means of TBP makes it possible to identify recent lesions that may go unnoticed when using dermoscopy.5,6 Our results show that the melanomas presented statistically significant changes in the macroscopic images more frequently than the melanocytic nevi. This finding reinforces the utility of 2-step digital follow-up for diagnosing malignant melanocytic lesions. According to previous digital dermoscopy studies,15 focal changes in pigmentation and in structure were more frequent in MM, but only the latter showed statistically significant differences. Furthermore, our study found a statistically significant association between asymmetric growth and a diagnosis of MM.
In the comparative study of the excised lesions (MM vs melanocytic nevus), only asymmetry and 3 of the dermoscopic structures analyzed (atypical globules, inverted pigmented reticulum, and polymorphous vessels) were statistically associated with MM. In terms of the scores used to diagnose the MM, both the TDS and the 7-point checklist showed differences between malignant and benign lesions. Nevertheless, the mean TDS values were in the range of suspicious lesion (4.75 to 5.45) and the values of the 7-point checklist were at the limit of malignancy (≥ 3), making it difficult to make a decision without considering the changes observed in the lesion over time.
All of the foregoing highlights the importance of follow-up of pigmented lesions in high-risk patients using digital dermoscopy, as these are atypical lesions where the clinical and dermoscopic characteristic of incipient malignant lesions and benign melanocytic lesions may be similar at a certain point.
We must point out some limitations of this study. First, it is a retrospective study, in which dermoscopic assessment was performed after the results of the histopathology study of the lesions was known. Moreover, given the small sample size, a multivariate study was not performed, which may introduce confounding factors. Further studies with larger sample sizes and blind assessment of the results will most likely be needed to determine the specific characteristics of MM more accurately.
This study illustrates the importance of performing thorough, long-term follow-up of patients with a higher risk of developing MM. The results highlight the use of 2-step follow-up in routine clinical practice.
In conclusion, 2-step follow-up combining DD and TBP in patients with a high risk of developing MM makes it possible to detect more superficial melanomas with fewer biopsies. TBP is essential, as macroscopic (and not just dermoscopic) changes are associated with a diagnosis of MM. Follow-Up by means of DD is also important, as many of the dermoscopic characteristics of MM are no different from those sometimes observed in benign melanocytic lesions.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Porcar Saura S, March Rodríguez Á, María Pujol R, Segura Tigell S. Seguimiento digitalizado combinado en población con alto riesgo de desarrollar un melanoma maligno: análisis retrospectivo de 152 pacientes. Actas Dermosifiliogr. 2021;112:250–256.