Aquagenic pruritus (AP) is characterized by the onset of pruritus after contact with water, with no evident skin lesions unlike aquagenic urticaria. It is an uncommon condition in Spain, but it can affect up to 20% of young adults in African countries.1 The disease may have a major negative impact on quality of life1 and management is difficult.2,3 One of the most effective treatments is phototherapy, but relapses are frequent and maintenance therapy is required.4 Cases have been reported in which an annual cycle of UVA and narrow-band UVB combination therapy (UVA/NB-UVB CT) achieved good outcomes.5,6 Our objective was to assess response to annual cycles of UVA/NB-UVB CT in patients with AP refractory to antihistamine agents.
Long-term clinical response was retrospectively analyzed in patients with AP refractory to high doses of antihistamine agents treated with UVA/NB-UVB CT in a reference hospital in Barcelona, Spain, between January 2010 and January 2019. Two women aged 52 and 31 years were identified. The case of patient 1 had been reported previously6; her mother also had AP. Patient 2 had celiac disease. In both cases, symptoms had presented more than 5 years previously and the patients had received multiple treatments (Table 1). Laboratory tests (hemogram, erythrocyte sedimentation rate, creatinine levels, liver and lipid profile) were normal in both patients, except for a small increase in IgE. They were treated with UVA/NB-UVB CT 3 times a week (17–34 sessions a year). The starting doses were 4 J/cm2 (UVA) and 200 mJ/cm2 (NB-UVB). The maximum doses were 9 J/cm2 (UVA) and 1.2 J/cm2 (NB-UVB) (Table 1). Patient 1 presented complete and prolonged response, remaining free of symptoms for more than 5 years with an annual cycle of UVA/NB-UVB CT (17–26 sessions before the beginning of the summer, 4 cycles in total). The second patient completed 36 sessions of UVA/NB-UVB CT during the first year, with no clinical improvement, and so phototherapy was discontinued.
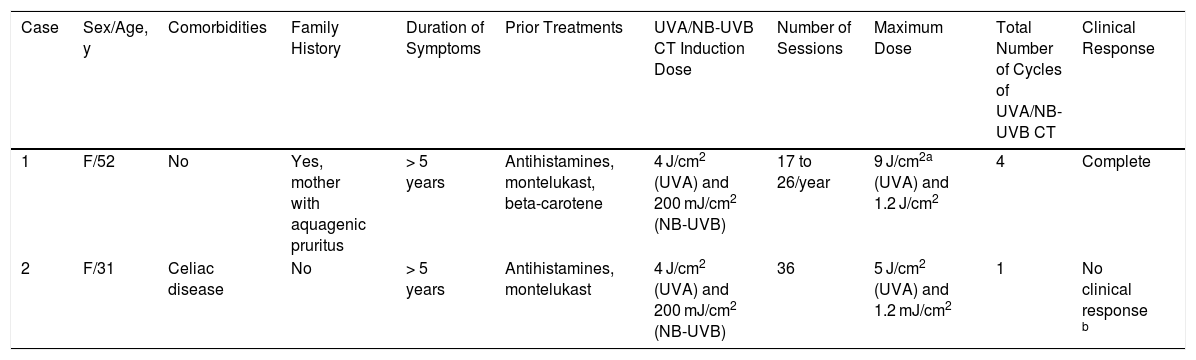
Clinical and Epidemiological Characteristics and Therapeutic Response of Patients With Aquagenic Pruritus in UVA and Narrow-Band UVB Combination Therapy.
| Case | Sex/Age, y | Comorbidities | Family History | Duration of Symptoms | Prior Treatments | UVA/NB-UVB CT Induction Dose | Number of Sessions | Maximum Dose | Total Number of Cycles of UVA/NB-UVB CT | Clinical Response |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F/52 | No | Yes, mother with aquagenic pruritus | > 5 years | Antihistamines, montelukast, beta-carotene | 4 J/cm2 (UVA) and 200 mJ/cm2 (NB-UVB) | 17 to 26/year | 9 J/cm2a (UVA) and 1.2 J/cm2 | 4 | Complete |
| 2 | F/31 | Celiac disease | No | > 5 years | Antihistamines, montelukast | 4 J/cm2 (UVA) and 200 mJ/cm2 (NB-UVB) | 36 | 5 J/cm2 (UVA) and 1.2 mJ/cm2 | 1 | No clinical response b |
Abbreviations: F, female; NB UVB, narrow-band UVB; UVA/NB-UVB CT, UVA/narrow-band UVB combined therapy.
AP is generally idiopathic, although up to 30% of cases have been associated with hematological conditions such as polycythemia vera or myelodysplasia,2 and 25% of cases may be associated with lactose intolerance. Other known associations include neoplasms, hepatitis C, and drugs such as bupropion and antimalarial agents.2 Idiopathic AP occurs more frequently in young women and has a longer duration than AP with a known cause.2 AP may seriously impact activities of daily living; it has been reported that up to 8% of patients may develop phobia of washing.1 One of our patients avoided getting her legs wet for fear of triggering pruritus and burning sensation. The pathophysiology of AP is not fully understood, although it is thought there is increased skin innervation with dysfunctional and hyperexcitable C-nerve fibers, probably caused by defective sodium channels.7 The role of histamine is minimal, thus explaining the limited response to antihistamine agents. Treatment of AP is complex and, often, outcomes are disappointing for both the physician and the patient.2 Different topical treatments have been used such as increasing the pH of water with sodium bicarbonate, capsaicin, and glycerol trinitrate. Oral drugs such as antihistamine agents, pregabalin, acetylsalicylic acid, beta blockers (propranolol, atenolol), and antidepressant drugs, among others have been tried (Table 2).2,3 There have also been reports of patients treated with interferon and omalizumab.8 Phototherapy is one of the most effective treatment modalities, including psoralene plus UVA (PUVA) and UVB. However, this is not curative and requires maintenance therapy to achieve symptomatic remission.9 This can be problematic with PUVA, given its carcinogenic potential. NB-UVB has a better safety profile, but evidence for its use in AP is very limited, with only 3 case reports available. In all cases, it was effective in inducing remission. In 2 patients, a weekly dose was required to maintain clinical response for 4 and 6 months, respectively.4 This regimen is associated with substantial logistic issues and expense. The third patient relapsed after suspending phototherapy and this was discontinued; propranolol was initiated with good response.3 Including our patients, there are 3 cases reported of treatment with UVA/NB-UVB CT in which an annual cycle is used as maintenance therapy, with excellent response in 2 of them5,6 while 1 case was refractory. Phototherapy probably acts as a neuromodulator, reducing the density of skin nerve fibers and levels of neural growth factors,10 in addition to its well-established immunomodulatory effect.
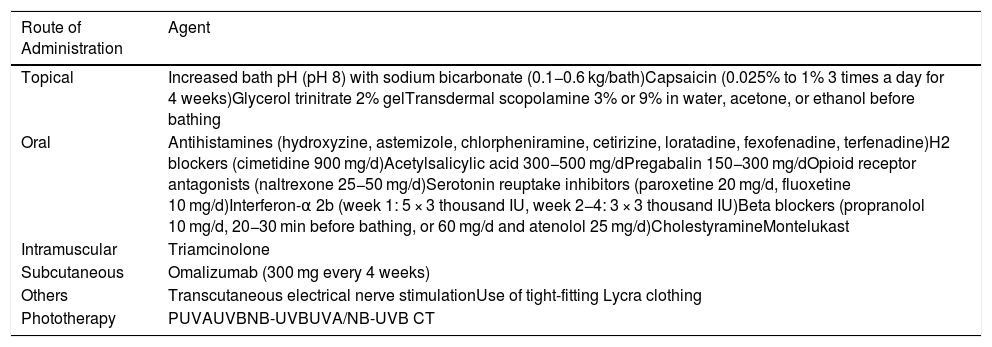
Drugs and Different Agents Used in the Treatment of Aquagenic Pruritus.
| Route of Administration | Agent |
|---|---|
| Topical | Increased bath pH (pH 8) with sodium bicarbonate (0.1−0.6 kg/bath)Capsaicin (0.025% to 1% 3 times a day for 4 weeks)Glycerol trinitrate 2% gelTransdermal scopolamine 3% or 9% in water, acetone, or ethanol before bathing |
| Oral | Antihistamines (hydroxyzine, astemizole, chlorpheniramine, cetirizine, loratadine, fexofenadine, terfenadine)H2 blockers (cimetidine 900 mg/d)Acetylsalicylic acid 300−500 mg/dPregabalin 150−300 mg/dOpioid receptor antagonists (naltrexone 25−50 mg/d)Serotonin reuptake inhibitors (paroxetine 20 mg/d, fluoxetine 10 mg/d)Interferon-α 2b (week 1: 5 × 3 thousand IU, week 2−4: 3 × 3 thousand IU)Beta blockers (propranolol 10 mg/d, 20−30 min before bathing, or 60 mg/d and atenolol 25 mg/d)CholestyramineMontelukast |
| Intramuscular | Triamcinolone |
| Subcutaneous | Omalizumab (300 mg every 4 weeks) |
| Others | Transcutaneous electrical nerve stimulationUse of tight-fitting Lycra clothing |
| Phototherapy | PUVAUVBNB-UVBUVA/NB-UVB CT |
Abbreviations: UVA/NB-UVB CT, UVA/narrow-band UVB combined therapy; NB UVB, narrow band UVB; PUVA, psoralene with UVA.
Treatment of AP is difficult. We have reported a new case of treatment with UVA/NB-UVB CT, without clinical response, and long-term follow-up of a female patient treated for more than 5 years (4 cycles of UVA/NB-UVB CT) with complete remission of symptoms. Cycles of UVA/NB-UVB CT once a year may be a good alternative for long-term management of some patients with refractory AP.
FundingThis study did not receive any funding.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morgado-Carrasco D, Riera-Monroig J, Feola H, Aguilera P. Tratamiento de 2 pacientes con prurito acuagénico con ciclos de terapia combinada UVA/UVB de banda estrecha una vez por año. Actas Dermosifiliogr. 2020;111:889–892.