This article in the series on safety in dermatologic procedures covers the delivery of basic cardiopulmonary resuscitation (using no devices), instrumental resuscitation (using an automated external defibrillator), and pharmacological resuscitation (using adrenaline). We provide a brief overview of the updated 2021 European Resuscitation Council guidelines and offer an algorithm and visual aids to support recommended practices.
En el presente artículo de la serie «Seguridad en procedimientos dermatológicos» se aborda la reanimación cardiopulmonar básica (sin empleo de ningún dispositivo), instrumentalizada (usando un desfibrilador externo automático) y farmacológica (haciendo uso de adrenalina). Se plantean las recomendaciones actualizadas en 2021 del Consejo Europeo de Resucitación de forma resumida, con material gráfico que las sistematiza de forma estructurada.
Mortality due to cardiac arrest has remained stable for more than 20 years, with survival rates on hospital discharge of 10% (although regional differences exist, with rates ranging from 1% to 25%). It is also a cause of morbidity, as it generates 4.5% of life years adjusted for disability.1–5
In 2021, the European Resuscitation Council issued a set of guidelines called Systems Saving Lives, based on the 2020 International Consensus on Cardiopulmonary Resuscitation Science.6
In this article, we discuss the cardiopulmonary resuscitation (CPR) maneuvers we can apply: Basic CPR, instrumental CPR, and advanced CPR.
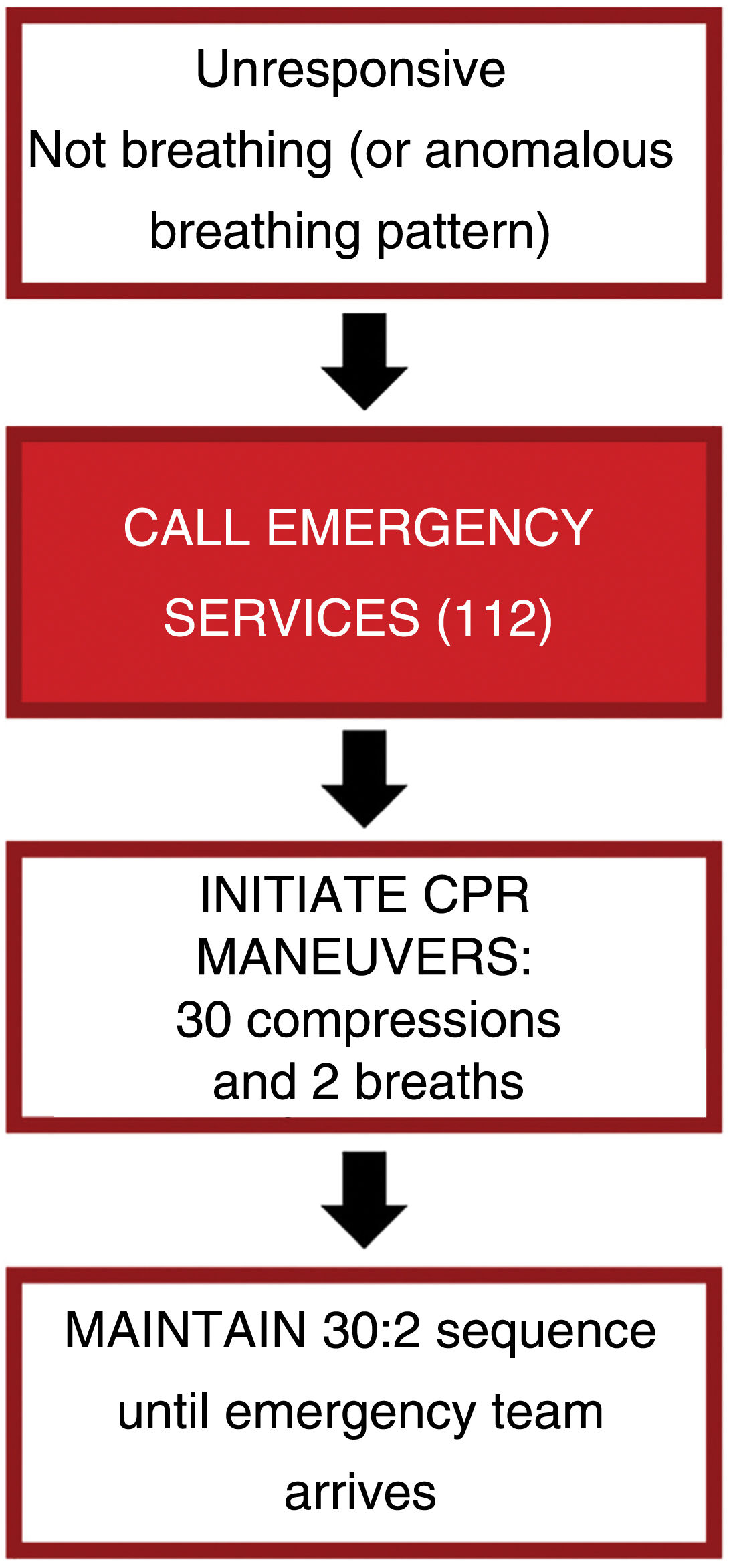
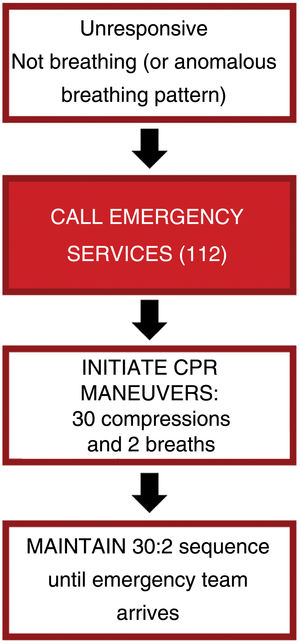
Basic Cardiopulmonary ResuscitationBasic CPR (Fig. 1) should be initiated in any person who “is unresponsive, with absent or abnormal breathing”, and it should be remembered that slow and labored breathing (agonic breathing) must be considered a sign of cardiac arrest. In the case of an unresponsive patient with a breathing pattern that would be considered normal, the patient should be placed on their side in the safety position (regarding pregnant women, always on the left side), remembering to assess breathing continuously.
Once cardiac arrest has been detected, the emergency medical services (EMS) should be notified immediately. Even when we are the only person available to perform resuscitation, this is still the first step we must take before beginning CPR.
We should begin chest compression (preferably on a firm surface):
- •
as soon as possible
- •
on the lower half of the sternum
- •
compressing to a depth of at least 5cm and no more than 6cm
- •
at a rhythm of between 100 and 120 times per minute
- •
with as few interruptions as possible
- •
ensuring that the chest recoils fully after each compression.
After the first 30 compressions, we should perform 2 rescue breaths (using the head-tilt, chin-lift maneuver to open the airway) and then continue with the compressions. If, for any reason, it is not possible to provide the rescue breathing, we must perform continuous chest compressions.
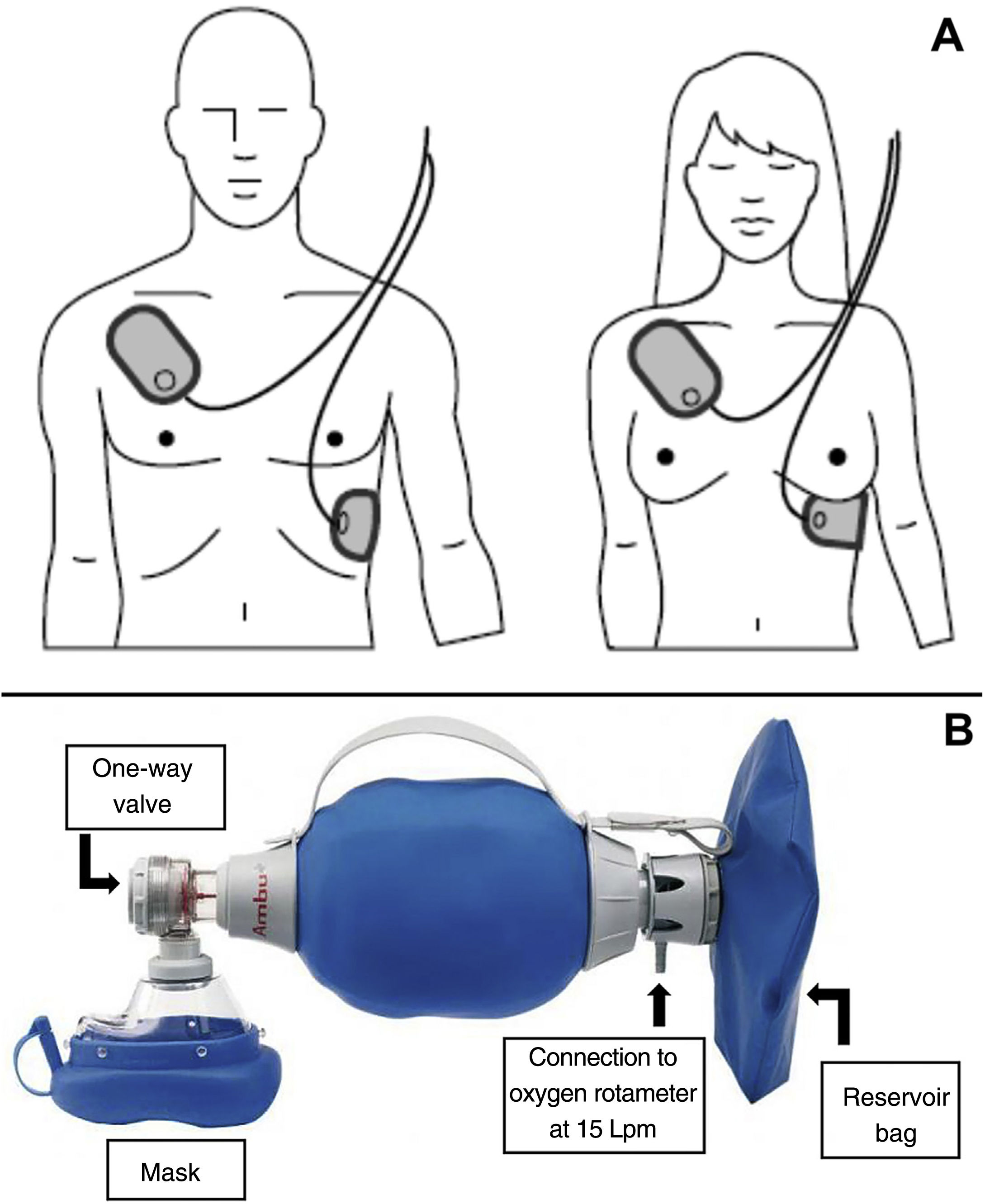
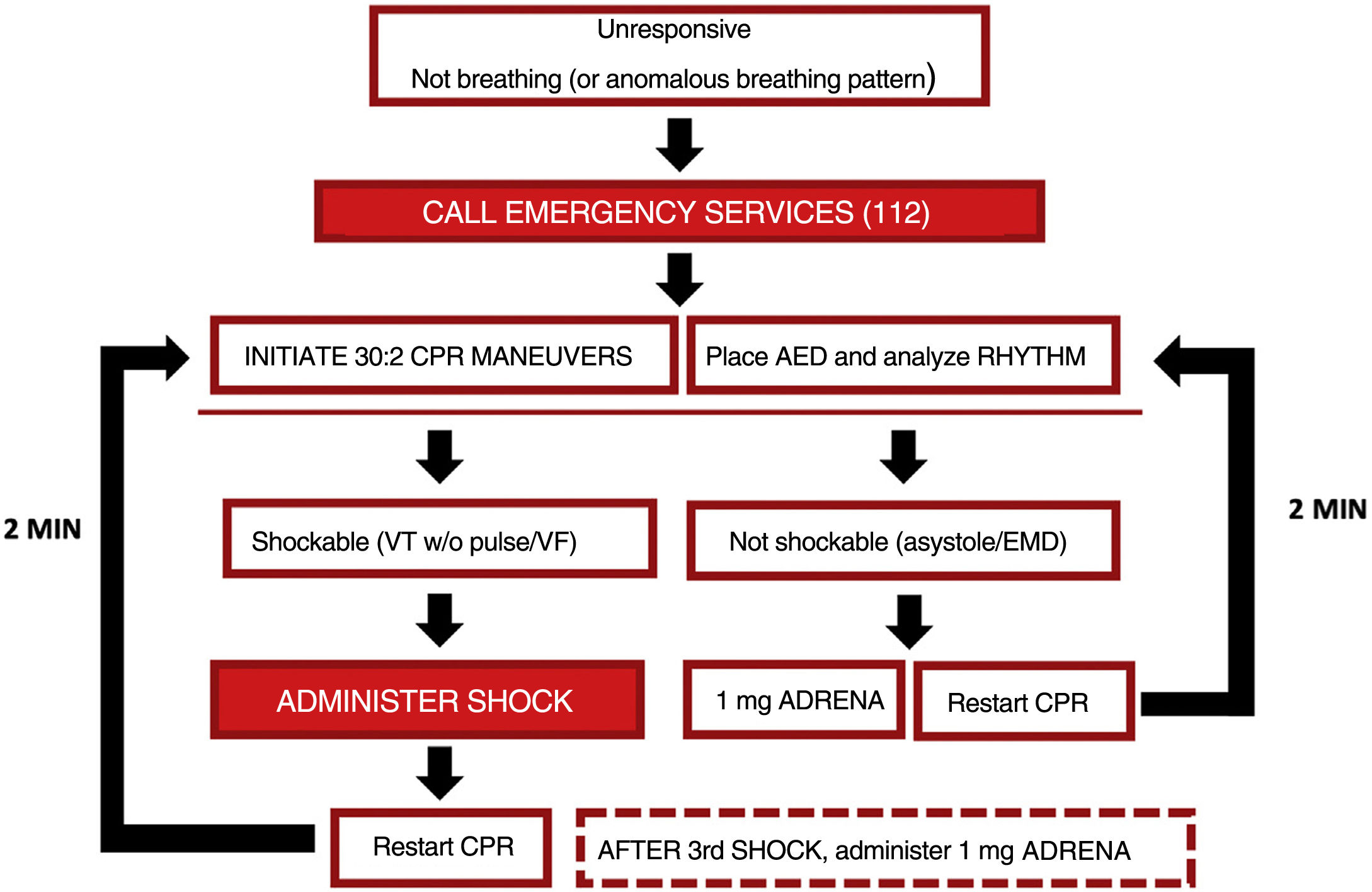
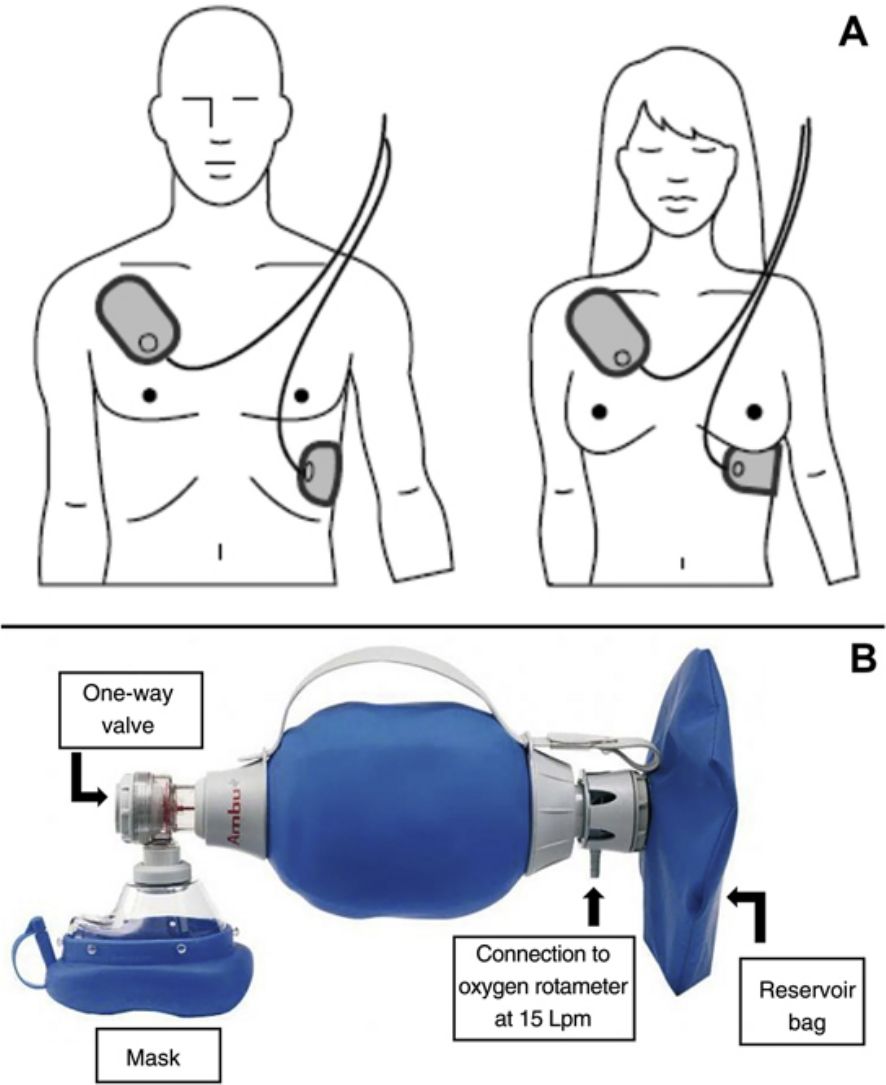
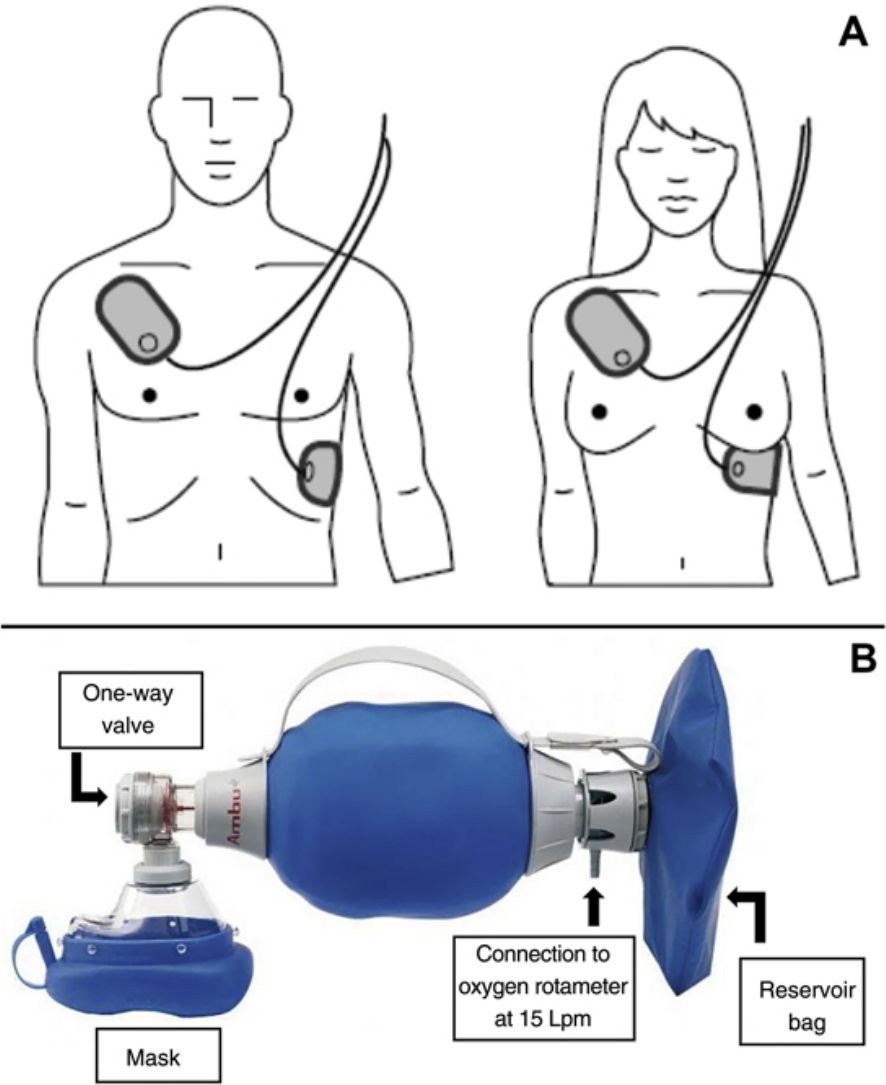
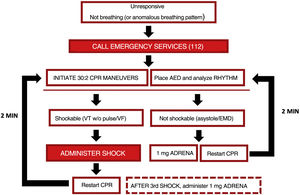
Instrumental Cardiopulmonary ResuscitationIf an automated external defibrillator (AED) is available, once basic CPR has begun, the electrodes must be placed on the patient's chest, in the position indicated on the AED (Fig. 2A), while (if more than one resuscitator is present) CPR continues. Although CPR must be maintained until the AED is connected to the patient and put into operation, defibrillation should not be delayed once the AED is ready.
When turned on, the AED will provide verbal and/or visual indications. When the heart rhythm is being analyzed, it is essential to ensure that nobody is in contact with the patient.
If defibrillation is indicated, we can continue with the CPR maneuvers while the device is being readied. Nobody must be touching the patient at the moment of defibrillation (which requires activation by pressing the button).
If the heart rhythm does not require defibrillation and immediately after the AED has discharged, CPR maneuvers must be restarted immediately, as indicated by the AED. After 2min of CPR, the AED will request another pause to analyze the heart rhythm and determine whether defibrillation is required or not.
If an oxygen source and self-inflating bag (commonly known by its initials AMBU, for air mask bag unit) connected to a face mask is available, respiration should be carried out using that device connected to the oxygen supply with the rotameter set at 15 liters per minute (maximum oxygen) and, if possible, with a reservoir bag (Fig. 2B). Instrumental CPR with a self-inflating bag can be complicated if only one resuscitator is present. If personnel are available, it is recommended that one resuscitator seal the mask with two hands and the other, who is performing the chest compressions, squeeze the bag during the pause for ventilation.
Individualized guidelines have been drawn up for patients with suspected or confirmed acute respiratory syndrome due to SARS-CoV-2. Those recommendations can be consulted at www.erc.edu/covid. In this case, airway management and breathing assessment is different from the steps described above:
- •
Visual assessment of breathing, without opening the airway or approaching the patient's nose or mouth.
- •
Before starting CPR, cover the patient's nose and mouth with a surgical mask or cloth and perform CPR maneuvers while protected with an FFP2/3 mask and/or personal protection equipment (if available).
- •
In the case of CPR in a patient with COVID-19, continuous chest compressions without breathing are indicated, unless a self-inflating bag and mask are available, through which 100% oxygen can be administered (with the placement of a special antiviral filter valve, if available).
The decision algorithm for instrumental CPR and pharmacologic CPR (explained in the following section) is summarized in Fig. 3.
Pharmacologic Cardiopulmonary ResuscitationFinally, if vascular access is available (ideally, intravenous, although intraosseous access may be considered if intravenous access is not possible), administration of 1mg of adrenaline should be considered, as per the following indications:
- •
As soon as possible in adult patients in CPR with a heart rhythm that is not shockable.
- •
After the third defibrillation shock in adult patients in CPR with a shockable rhythm.
- •
Every 3–5min (repeated administration of 1mg of adrenaline) while CPR maneuvers last.
These guidelines, based on the latest guidelines published in 2021, stress several points that we will summarize below:
- •
Encourage the early recognition of patients suffering from cardiac arrest.
- •
Achieve high quality chest compressions with minimal interruption.
- •
Ensure early defibrillation.
- •
Administer adrenaline as soon as possible when the cardiac arrest rhythm is not shockable, and after 3 attempts at defibrillation if the cardiac arrest rhythm is shockable.
The authors declare that they have no conflicts of interest with regard to the content of this article.
The authors would like to thank Dr. José Luis Azpiazu for his excellent presentation at the group of conferences on safety in dermatologic procedures. The authors would also like to thank all the members of the dermatology forum Dermachat.