A 66-year-old man was seen in March 2020 for a slow-growing asymptomatic lesion on the right leg that had appeared several years earlier. Physical examination revealed a shiny, erythematous, violaceous plaque with poorly defined borders, and the absence of other similar lesions elsewhere on the body (Fig. 1). The patient did not recall any prior bite or trauma in the affected area. He had a history of high blood pressure, for which he had been treated for several years with manidipine and losartan/hydrochlorothiazide, and was in dermatological follow-up for chronic actinic damage, for which he had been undergoing photodynamic therapy since 2016.
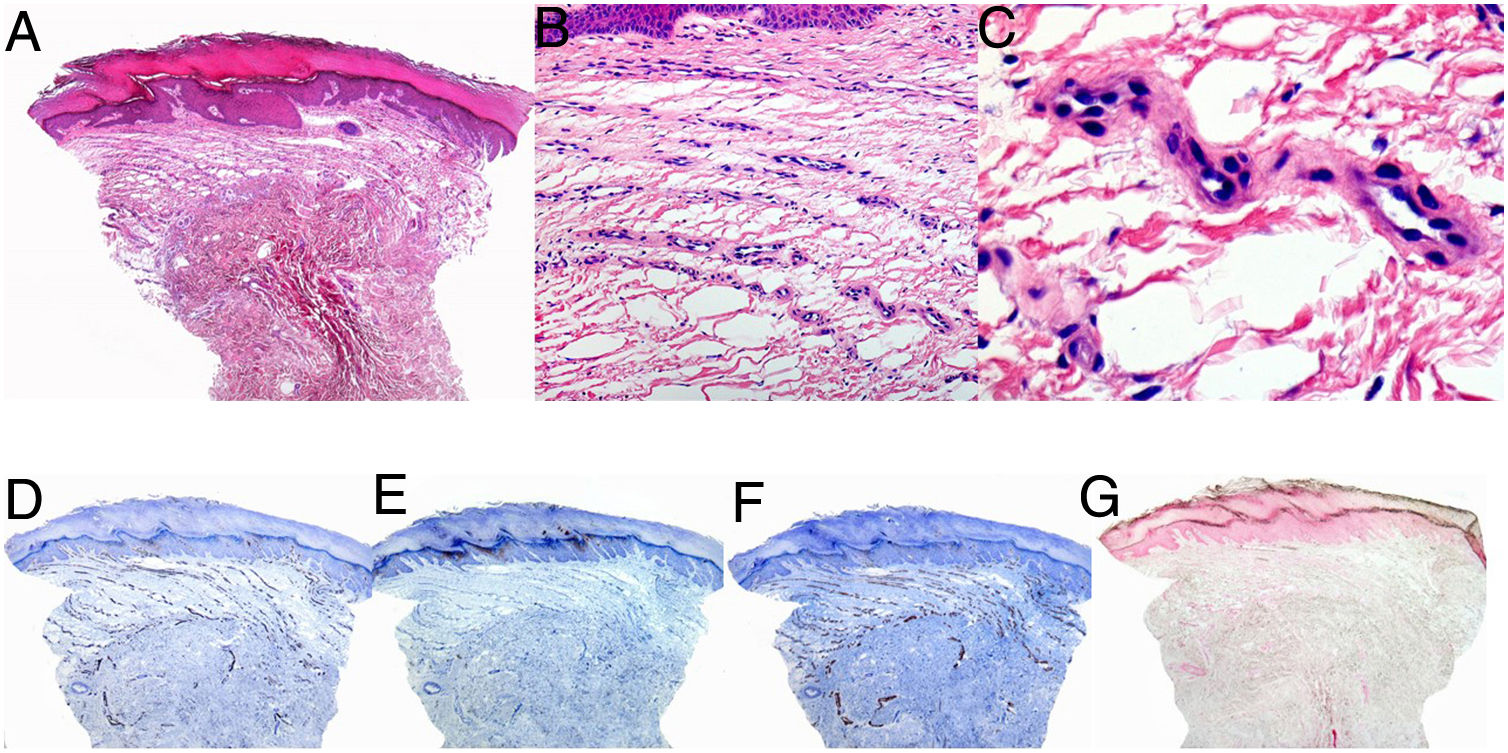
A biopsy was performed based on a suspected diagnosis of mycosis fungoides. Histology showed hyperkeratosis of the epidermis with irregular hyperplasia and edema, proliferation of small caliber vessels, and discreet fibrosis in the dermis. No evidence of malignancy was observed in the examined sample. Immunohistochemistry confirmed that the vessels within the lesion were positive for CD31 and small muscle actin (SMA), and negative for D2-40 and Perls blue (Fig. 2).
Histological images showing hyperkeratosis and irregular hyperplasia of the epidermis and blood vessel proliferation in a band-like pattern in the superficial dermis. A–C, Hematoxylin eosin, panoramic view (A), original magnification ×20 (B), original magnification ×40 (c). D, CD31. E, Small muscle actin. F, D2-40. G, Perls blue.
What is your Diagnosis?
DiagnosisPoikilodermatous plaque-like hemangioma.
Clinical Course and CommentBased on the clinical and pathological findings it was possible to establish a diagnosis of poikilodermatous plaque-like hemangioma, for which the patient began treatment with clobetasol propionate and pimecrolimus on alternate days for 2 months. No improvement was observed, and treatment was consequently discontinued.
Poikilodermatous plaque-like hemangioma is an entity recently described in a series of 16 patients by Semkova et al.,1 and subsequently in an additional case report.2 This lesion occurs more frequently in males aged 50 years and above, manifesting as a single erythematous or violaceous plaque, generally located on the lower extremities, as in the present case. Follow-up of cases described to date (maximum follow-up duration, 6 y) indicates a benign course (i.e. stable, without malignant transformation). However, given that this is a recently described pathology, it is advisable to be attentive to any changes or progression.
Histology of this lesion is characteristic, revealing a band-like pattern of proliferating thin-walled vessels with features of postcapillary veins in the superficial dermis. Changes such as hyperplasia and spongiosis can be observed in the epidermis. Strikingly, epidermal atrophy is absent, despite the clinical appearance of the lesions. Fibrotic changes in the dermis are occasionally described.
The main differential diagnosis is solitary plaque mycosis fungoides,3 owing to the clinical presentation and location of the lesions. In contrast to plaque mycosis fungoides, this lesion features a more reddish–violet coloration and thin atrophic skin without scaling, findings that can help orient the diagnosis. Other conditions to be considered in the differential diagnosis include fixed drug eruption, chronic atrophic acrodermatitis, chronic pigmentary purpura, and acquired elastotic hemangioma (D2-40+).
While the etiology is unknown, authors who have described this entity have highlighted a cluster of cases in northern England, suggesting a potential common external or infectious agent. Our patient reported no recent trips to England.
It should be noted that for the diagnosis of vascular anomalies most dermatologists rely on the International Society for the Study of Vascular Anomalies (ISSVA) classification,4 which was most recently updated in 2018 but does not include all entities seen by dermatologists on a daily basis, such as lobular capillary hemangiomas, intramuscular hemangiomas,5 or poikilodermatous plaque-like hemangioma.
In conclusion, we describe a case of poikilodermatous plaque-like hemangioma, a condition we believe should be considered in patients with corresponding clinical signs.
Conflicts of InterestThe authors declare that they have no conflicts of interest.