Biologic therapies have revolutionized the management of psoriasis and atopic dermatitis. Traditionally, it has been understood that the pathogenic mechanisms of both diseases are different (mediated by Th1 lymphocytes in psoriasis and Th2 lymphocytes in atopic dermatitis). However, some patients exhibit both conditions concomitantly, usually in mild forms, being severe forms exceptional and difficult to treat.1–3 We present 2 cases with this exceptionally rare association and their progression with 2 biologic therapies.
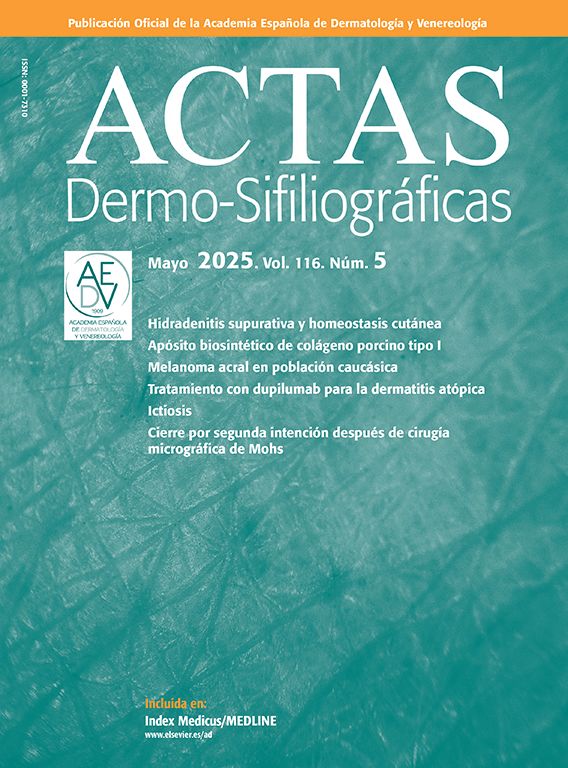
Patient #1 is a 50-year-old man with a family history of psoriasis (father), and a personal history of rhinitis, asthma, and schizophrenia, which remained under control with carbamazepine, clonazepam, and risperidone. He also had a 30-year history of severe atopic dermatitis (figure 1a). Over the years, he had been on multiple treatments, both topical (corticosteroids and tacrolimus), and systemic (oral prednisone, phototherapy, methotrexate, and cyclosporine) for his dermatitis with partial atopical symptom relief. Before starting dupilumab, he had a SCORAD score of 59. Three years before starting the dual treatment, he was prescribed dupilumab at standard doses, which significantly improved his skin lesions. One year later, following a decompensation of his psychiatric condition, his diagnosis was changed to bipolar disorder, and he was put lithium therapy. Coinciding with the initiation of this drug, the patient started developing extensive psoriatic lesions primarily affecting his face, neck, and upper limbs, with a PASI score of 16 and a BSA of 13 (figure 1b). After ruling out drug interactions, cyclosporine was added to the dupilumab therapy, resulting in significant improvement, but also relapses of psoriasis each time the dose of cyclosporine would be down-titrated. After 18 months on this treatment, cyclosporine was discontinued, and guselkumab was initiated to keep psoriasis under control, with a good response to the new drug. After more than a year on combined biologic therapy (guselkumab+dupilumab), the patient is now free of active lesions from both conditions and no adverse events have been reported (Figure 1c and d).
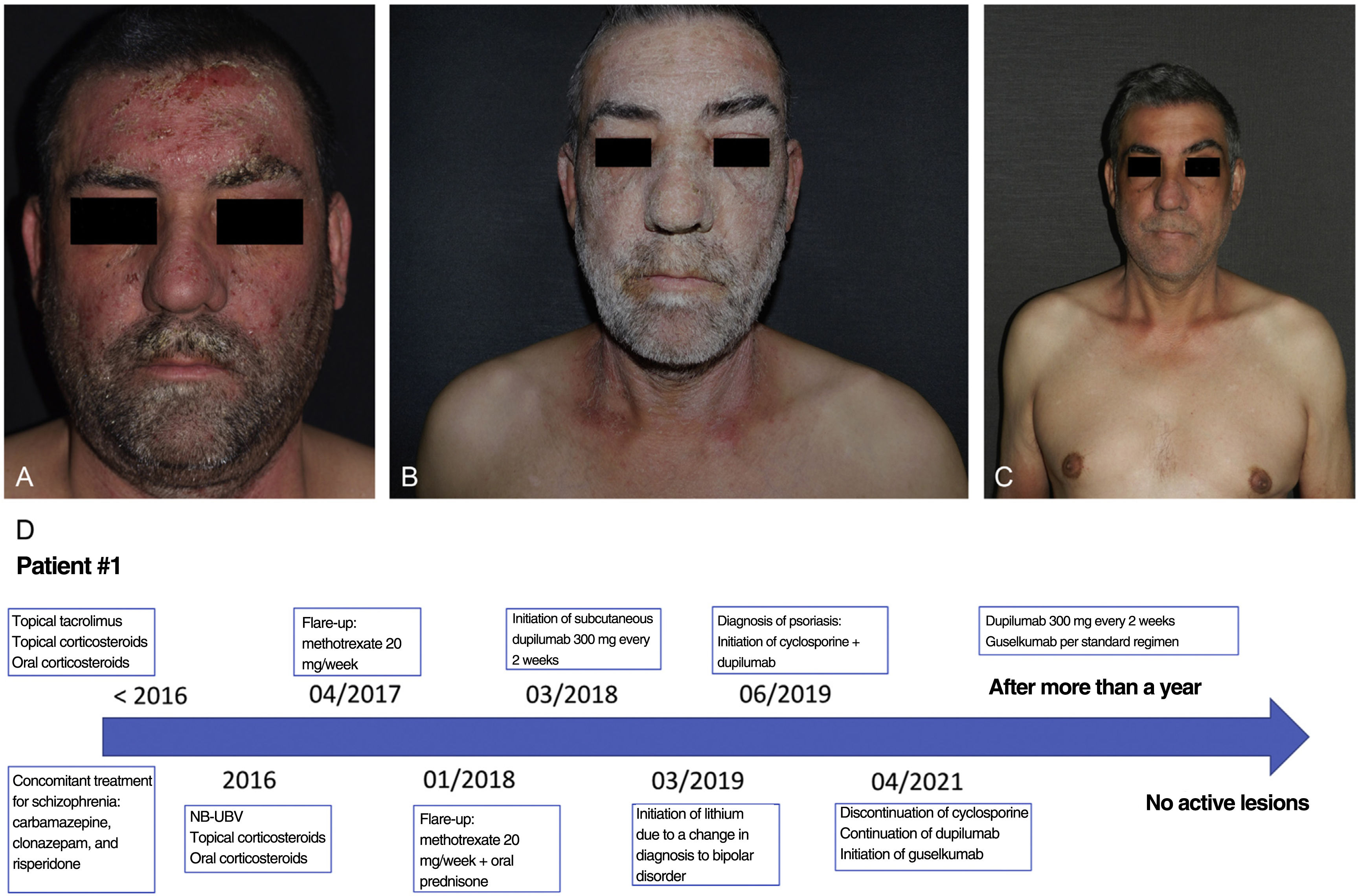
Patient #2 is a 41-year-old man with severe psoriasis since adolescence and a 7-year history of severe atopic dermatitis as confirmed by biopsy. He also had morbid obesity (170kg with a BMI of 58) as a comorbidity. He had been treated with topical and systemic corticosteroids, methotrexate, azathioprine, cyclosporine, and phototherapy, without achieving good control of either disease (figure 2a). Four years before starting the dual therapy, he experienced a new psoriasis flare-up, mostly psoriasiform in nature, with a PASI of 35, a BSA of 84, and a SCORAD score of 23. He started therapy with ustekinumab, which initially improved the psoriasis component but later lost its effectiveness. Subsequently, he was treated with ixekizumab and then with guselkumab plus azathioprine, achieving good psoriasis control but poor atopic dermatitis control. Azathioprine was discontinued, and he was put on dupilumab. After 10 months of combined biologic therapy (guselkumab+dupilumab), the patient's psoriasis remains under control (PASI 7 and BSA 7), unlike his atopic dermatitis (SCORAD 85 and NRS 8) (Figure 2b and c).
Psoriasis and atopic dermatitis are 2 highly prevalent inflammatory skin diseases.2,4 Recent publications suggest that there are common pathogenic pathways in both diseases mediated by Th1 and Th17 lymphocytes.1 Very few articles have been published on the management of severe psoriasis and atopic dermatitis. In fact, we only found 1 report on a series of 6 patients with both conditions treated with 2 biologic drugs (dupilumab and guselkumab) simultaneously. In this review, 1 patient had no active lesions, 4 had improved both of their conditions, and only 1 had improved the atopic component with this therapy. No significant adverse events were reported in any of these patients.5 Following the publication of this review, we decided to initiate combined treatment with dupilumab and guselkumab in these 2 patients. In addition, a literature search was conducted on the efficacy of JAK inhibitors in the management of these conditions as a possible therapeutic target that interferes with the pathogenic pathways of both diseases. The use of these drugs was discarded due to their limited effectiveness in the management of severe psoriasis.6,7 We presented our own experience with a dual biologic therapy in 2 patients with an exceptionally rare association of severe psoriasis and atopic dermatitis. In our cases, patient #1 achieved control of both conditions at the 12-month follow-up, remaining asymptomatic and without adverse events. At the 10-month follow-up, patient #2 achieved good control of the psoriasiform component, but poor control of the atopic one, possibly due to his obesity, without any adverse events being reported. The main limitation of this clinical note is that the diagnosis of psoriasis in patient #1 was clinical and was established without lesion biopsy. Due to the limited published literature in this area, long-term monitoring of these patients is needed to assess the safety and efficacy of the combination of both drugs.
Conflicts of interestNone declared.