The patient was a 79-year-old woman with a history of rheumatoid arthritis, osteoporosis, and advanced chronic kidney disease managed with renal replacement therapy (hemodialysis). She was referred to the dermatology department of our hospital for assessment of a lesion on her left shoulder that had first appeared several months earlier. The lesion had grown and was occasionally pruritic.
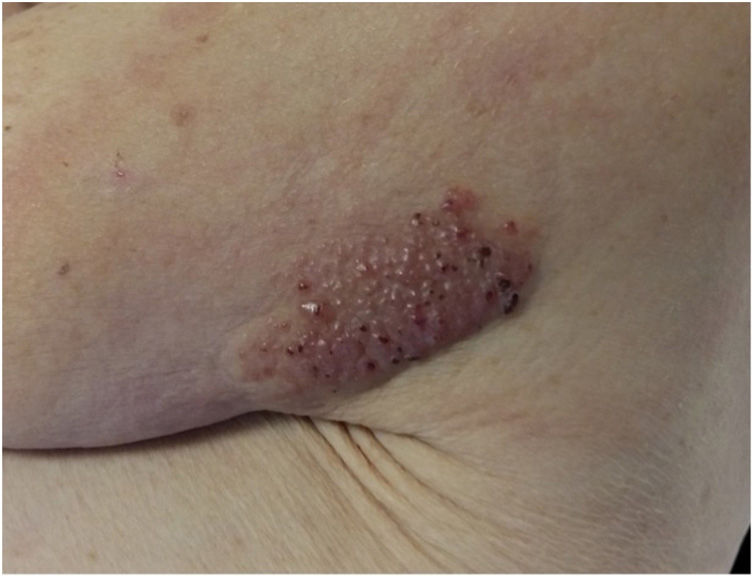
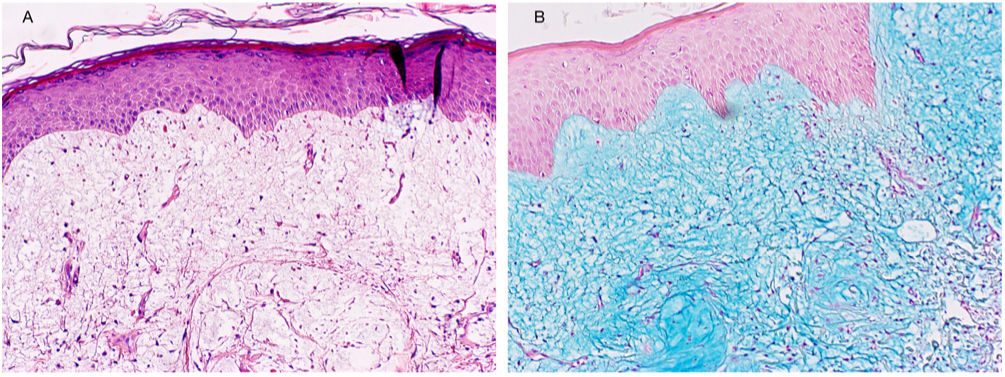
Physical Examination and HistopathologyAt her first visit, we observed a single red-violaceous plaque (8cm×5cm) with a clustered pseudovesicular surface on the posterior aspect of her left shoulder (Fig. 1). Histopathology revealed a preserved epidermis (Fig. 2A). A diffuse mucin deposit was observed in the upper reticular and papillary dermis (positive for Alcian blue staining), together with a slight increase in irregularly distributed fibroblasts and a modest perivascular lymphoplasmocytic infiltrate (Fig. 2B). The elastic fibers were diminished and fragmented. Thin-walled arborizing vessels were visible in the deep dermis.
The lesions began to improve 1 month after the biopsy, with only a pseudovesicular plaque (7mm in diameter) on a residual erythematous-violaceous base remaining (Fig. 3). The lesion had resolved completely at 6 months. Subsequent analysis revealed anemia of chronic disease and increased urea and plasma creatinine (these findings were previously known), with normal thyroid function and absence of paraproteinemia.
What is your diagnosis?
DiagnosisAdult self-healing papular mucinosis.
Discussion and CommentaryCutaneous mucinosis comprises a very diverse and heterogeneous group of diseases, all of which are characterized by abnormal accumulation of mucin in the skin. Mucins are high-molecular-weight proteins composed of glycosaminoglycans. They are synthetized by dermal fibroblasts and act as a key factor in maintaining the hydrosaline balance in the skin.1
According to the most widely accepted classification, which was proposed by Rongioletti and Rebora in 2001, cutaneous mucinosis can be divided into the localized form (papular mucinosis, also known as lichen myxedematosus) and the generalized form (scleromyxedema).2 Mucinosis can also be idiopathic (primary) or secondary to other conditions.2
Self-healing papular mucinosis (SHPM) is an uncommon entity belonging to the group of localized cutaneous mucinoses (lichen myxedematosus). Since it is more common in children, it was initially reported as a pediatric condition (1–15 years) that manifests with multiple lesions and, occasionally, systemic symptoms. However, there have been reports of cases appearing in adulthood and involving localized lesions.3
Unlike generalized cutaneous mucinosis (scleromyxedema), the variants of lichen myxedematosus are not usually associated with systemic diseases, thyroid problems, or paraproteinemia. There have been reports of cases of SHPM in adults with type 2 diabetes mellitus, bacterial pneumonia, and autoimmune diseases such as rheumatoid arthritis.4 However, the etiology-pathogenesis of SHPM is unknown.
Adult SHPM is traditionally characterized by multiple pseudovesicular papules arranged symmetrically and mainly affecting the upper half of the skin (head, neck, shoulders, abdomen). The papules may coalesce to form plaques and/or nodules and may be associated with systemic symptoms (fever, asthenia, joint and muscle pain). Very few cases of adult SHPM with unilateral and asymmetrical involvement have been reported.5 The skin lesions tend to resolve spontaneously over a period of weeks or months. Histology frequently reveals abundant mucinous material in the middle and upper dermis, with a slight increase in the fibroblast count. These findings usually appear alongside a nonspecific inflammatory pattern.
We present a case of adult SHPM that presented asymmetrically and involuted spontaneously. Given the considerable heterogeneity of cutaneous mucinosis, the correlation between disease and symptoms could be key to reaching a correct diagnosis, especially in atypical cases. Lastly, it is important to distinguish between SHPM and self-healing juvenile cutaneous mucinosis, since these are different entities.
Conflicts of InterestThe authors declare that they have no conflicts of interest.