Cartas Científico-Clínicas de interés
More infoThe Spanish National Epidemiology Center/Instituto de Salud Carlos III records the incidence of syphilis and other sexually transmitted infections (STIs) diagnosed in Spain each year. In 2018 (the most recent year for which data were available at the time of writing), a total of 5079 syphilis cases were diagnosed in Spain. This figure is 6.7 times the mean incidence reported between 1996 and 2001.1 Considering the growing number of syphilis cases and the importance of early diagnosis, it is essential to contemplate syphilis in multiple differential diagnoses.2 We present a case of granulomatous secondary syphilis, a rare variant that is clinically and histologically challenging to diagnose. We also illustrate the usefulness of immunohistochemistry in this setting.
A 51-year-old, heterosexual, cisgender woman of Spanish nationality, with no known allergies or other history of interest, was seen at our department for a 15-day history of a mildly pruritic rash that had begun on the abdomen and spread to the proximal limbs. She had not experienced fever or any other systemic symptoms. She did not mention any lesions on the genitalia or oral mucosa and had not taken any drugs before the onset of the rash. She reported being in a closed relationship with a stable partner, a cisgender male at no obvious risk for STIs.
Physical examination revealed a papular, nonscaling rash consisting of dozens of pink spots with a diameter of between 3 and 10mm that were located predominantly on the abdomen (Fig. 1) but also extended to the top of the limbs. The palms and soles were spared. The external genitalia and oral mucosa were also unaffected, and there were no palpable lymph nodes. The entities considered in the clinical differential diagnosis were atypical pityriasis lichenoides, lymphomatoid papulosis, and pityriasis rosea.
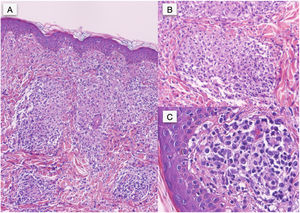
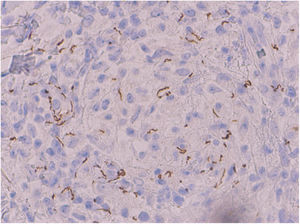
In the histopathologic study, hematoxylin-eosin staining showed a normal epidermis and a predominantly perivascular nodular inflammatory infiltrate in the upper dermis comprising histiocytic cells, several multinucleated giant cells, epithelioid cells, lymphocytes, and abundant plasma cells; there was no evidence of caseous degeneration (Fig. 2A). Clusters of mononuclear cells with abundant plasma cells surrounding small vessels were seen in the mid dermis, with endothelial edema and swelling (Fig. 2B and C). Specific immunohistochemical staining for Treponema pallidum revealed abundant intracellular and extracellular helical structures (Fig. 3).
The enzyme-linked immunosorbent assay and Treponema pallidum hemagglutination test were positive, as was the rapid plasma reagin (RPR) test, with a titer of 1:32. HIV serology was negative. Given the presence of granulomas on histology (these are much more common in late phases of syphilis than in secondary syphilis), 3 doses of benzathine penicillin 2.4 million international units were administered over 3 consecutive weeks (1 dose a week). The skin lesions disappeared several days after the last dose and the subsequent serologic response was adequate (RPR titer of 1:2 at 6 months). The patient's partner (the only other contact reported) was tested and was also positive. He received similar treatment at another center. Since both patients denied any other contacts, wider contact tracing was not possible.
The latest analysis of trends in STIs published by the Spanish National Epidemiology Center shows a significant growth in syphilis cases since 2016.1 We are thus increasingly likely to be faced with any of the multiple manifestations of syphilis in routine care. We have described a case of granulomatous secondary syphilis presenting predominantly as nonscaling papules with sparing of the palms and soles. Granulomatous inflammation in syphilis has been linked to advanced stages of the disease and is very uncommon in secondary syphilis.3–6 A high index of clinical suspicion and early diagnosis are key to clinical and epidemiological control, as early phases of the disease (primary and secondary syphilis) are infectious.7 As occurred in our case, full contact tracing is often not possible.8 Considering that syphilis has clinical and histologic similarities to a broad range of diseases and conditions, it should be contemplated in multiple differential diagnoses.9
The incidence of syphilis continues to grow in Spain. High clinical suspicion and treatment of early phases are essential for achieving clinical and epidemiological control. Considering its multiple clinical and histopathologic variants, syphilis should not be forgotten in the list of differential diagnoses in the dermatology clinic. Immunohistochemical techniques can be very useful in atypical cases.10
Conflicts of InterestThe authors declare that they have no conflicts of interest.