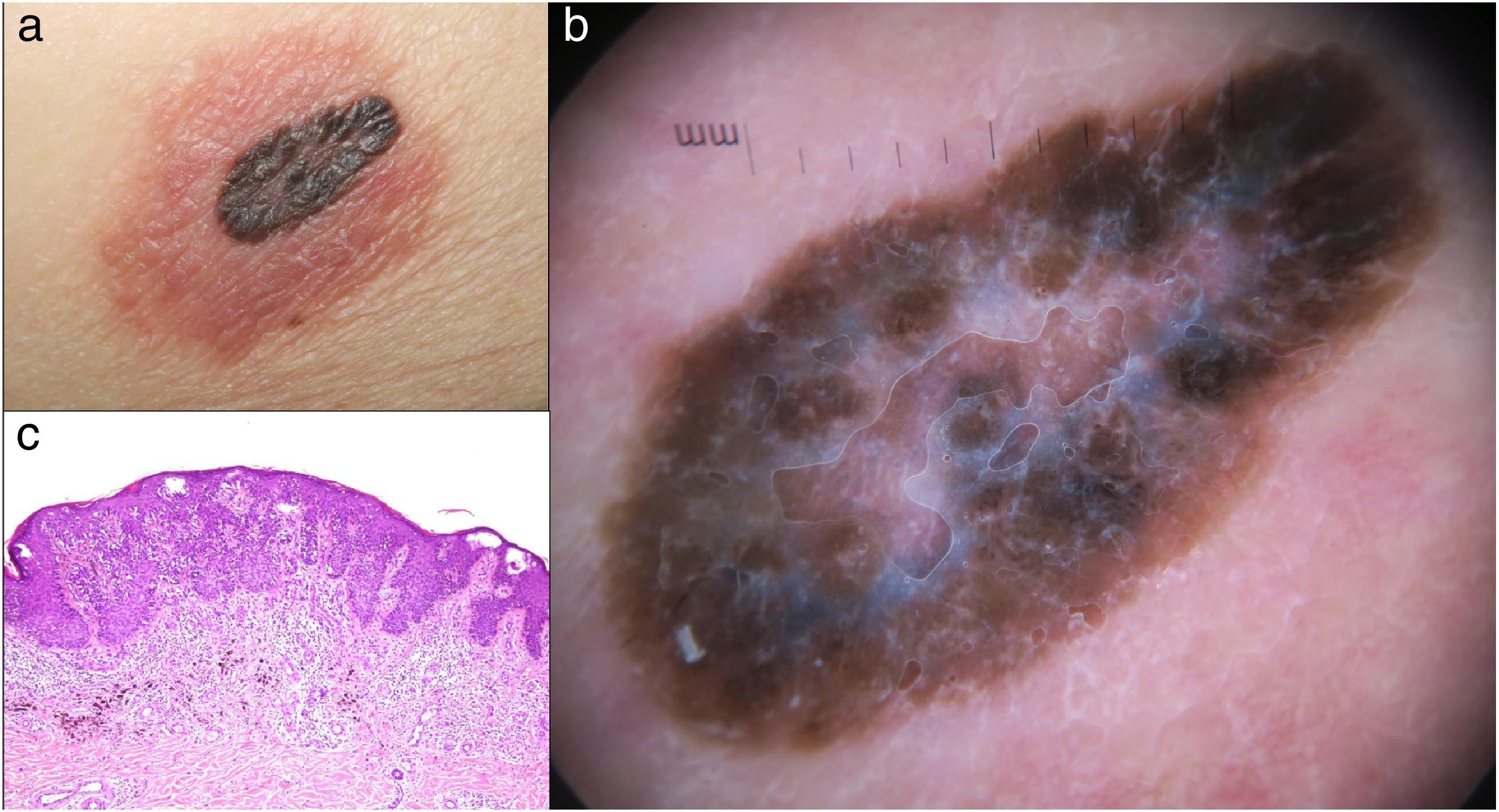
A 65-year-old woman was referred to our Department of Dermatology for a pruriginous lesion on her abdomen that failed to show improvement after 1-month of topical corticosteroid treatment. She presented with a congenital nevus, that 2 months prior consultation developed a red, scaly and pruritic halo. Physical examination showed a pigmented brown-black, 1.6 cm, slightly elevated lesion on the left flank surrounded by an erythematous scaly halo (Fig. 1(a)). Dermoscopic appearance revealed an atypical, pigmented, dark brown-black irregular lesion with a blue-white veil in the center surrounded by erythema and scarce dotted vessels within the halo (Fig.1(b)). Histopathological analysis demonstrated a superficial spreading melanoma with radial and vertical growth phase, Clark Level IV, Breslow depth of 0,98 mm. An acanthotic epidermis with discrete spongiosis and intense chronic inflammatory component was also observed (Fig.1(c)). After the initial excision, the eczematous halo was soon resolved. Further imaging studies failed to show signs of metastasic disease, followed by a 1-cm surgical margin and selective sentinel lymph node biopsy that resulted negative.
(a) Central pigmented lesion and surrounding eczematous halo. (b) Dermoscopy revealing central pigmented dark brown-black atypical and irregular lesion with a blue-white veil in the center surrounded by erythema and scarce dotted vessels within the halo. (c) Histopathologic appearance of Meyerson phenomenon within a melanoma. Intraepidermal atypical, confluent melanocytic proliferation. Mild spongiosis, epidermal acantosis and chronic inflammatory cell infiltrate. (Hematoxylin-eosin stain; original magnification: ×20).
Clinical, dermoscopic and histological correlation established the diagnosis of malignant melanoma with Meyerson phenomenon.
CommentaryMeyerson phenomenon (MP) refers to a localized eczematous eruption classically associated with benign melanocytic nevi, hence the denomination Meyerson nevus.1 Considered rare, but possibly underdiagnosed, MP has generally reflected a sign of banal lesions2 including dermatofibromas,3 seborrheic keratosis,3 keratosis stucco3 and angiokeratoma,4 among others. However, dysplasic nevi, and few cases of basal cell and squamous carcinomas have also been described.2 Only anecdotal reports of melanoma in situ have been reported in medical literature.5 Our case particularly reveals an invasive malignant melanoma.
Our case highlights that lesions targeted by the MP are not necessarily benign and thus careful dermoscopic examination is warranted to prevent overlooking malignant melanocytic lesions.
Please cite this article as: Calderón-Castrat X, Conde-Ferreirós A, Yuste-Chaves M, Santos-Briz A. La bandera roja: fenómeno de Meyerson en el melanoma maligno. Actas Dermosifiliogr. 2021;112:259–260.