To the Editor:
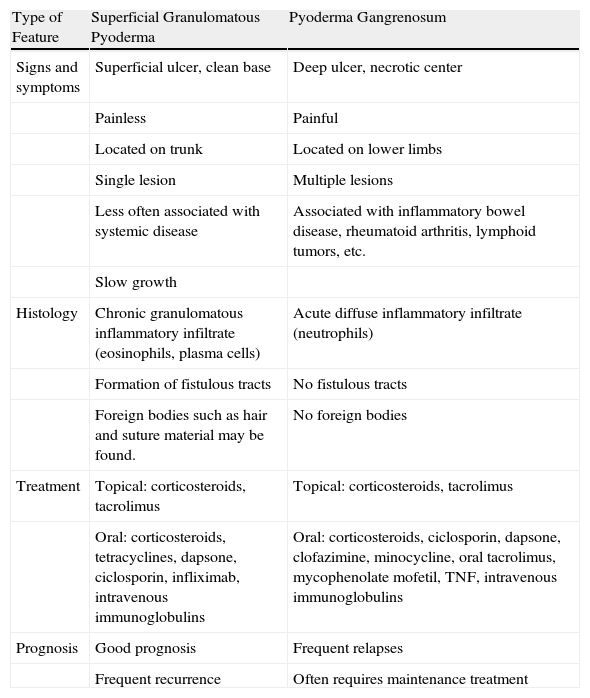
Superficial granulomatous pyoderma (SGP) or pyoderma vegetans is a rare inflammatory disease first described by Wilson-Jones and Winkelmann in 1988.1 Although considered a superficial, vegetative variant of pyoderma gangrenosum (PG), SGP has distinguishing features such as a chronic and slowly progressive course, lack of association with other diseases, shallower ulcers, the presence on histology of characteristic 3-layered granulomas,2 and better response to treatment (Table 1).
Differential Characteristics of Superficial Granulomatous Pyoderma and Pyoderma Gangrenosum.
| Type of Feature | Superficial Granulomatous Pyoderma | Pyoderma Gangrenosum |
| Signs and symptoms | Superficial ulcer, clean base | Deep ulcer, necrotic center |
| Painless | Painful | |
| Located on trunk | Located on lower limbs | |
| Single lesion | Multiple lesions | |
| Less often associated with systemic disease | Associated with inflammatory bowel disease, rheumatoid arthritis, lymphoid tumors, etc. | |
| Slow growth | ||
| Histology | Chronic granulomatous inflammatory infiltrate (eosinophils, plasma cells) | Acute diffuse inflammatory infiltrate (neutrophils) |
| Formation of fistulous tracts | No fistulous tracts | |
| Foreign bodies such as hair and suture material may be found. | No foreign bodies | |
| Treatment | Topical: corticosteroids, tacrolimus | Topical: corticosteroids, tacrolimus |
| Oral: corticosteroids, tetracyclines, dapsone, ciclosporin, infliximab, intravenous immunoglobulins | Oral: corticosteroids, ciclosporin, dapsone, clofazimine, minocycline, oral tacrolimus, mycophenolate mofetil, TNF, intravenous immunoglobulins | |
| Prognosis | Good prognosis | Frequent relapses |
| Frequent recurrence | Often requires maintenance treatment |
We present 2 cases of SGP that were successfully treated with topical tacrolimus, with no recurrence after 5 years.
Case 1A 77-year-old man with a history of hypertension and type 2 diabetes mellitus presented in July 2003 with erosive papular lesions, some of them with follicular dominance. The lesions coalesced to form plaques prone to ulceration and the formation of crusts on the buttocks and scalp (Fig. 1A). On the upper back he had a horseshoe-shaped ulcer measuring 7×10cm with an atrophic center and erythematous-violaceous borders (Fig. 1B). The lesions had first appeared several months earlier and had been treated with topical antibiotics and oral cephalosporins. No improvement was observed. Cultures for bacteria, fungi, and mycobacteria were negative. Skin biopsy revealed an acute and chronic inflammatory infiltrate that was predominantly follicular, with rupture of the follicular epithelium and a granulomatous reaction with giant cells (Fig. 1C). Results of laboratory tests were within the normal range. The patient received successive treatments with corticosteroids and topical antibiotics, oral tetracyclines, trimethoprim-sulfamethoxazole, colchicine, and isotretinoin, but little improvement was noted. Finally, after 6 months of treatment with topical tacrolimus 0.1% the lesions healed, leaving cribriform scars (Fig. 1D and 1E).
A, Plaques with ulcers on the buttocks. B, Horseshoe-shaped ulcer measuring 7×10cm with an atrophic center and erythematous-violaceous borders on the upper back. C, Predominantly follicular inflammatory infiltrate with rupture of the follicular epithelium and granulomatous reaction with giant cells (hematoxylin-eosin, original magnification ×100). D, Residual scars on the buttocks. E, cribriform scars on the back.
A 33-year-old woman with a history of schizophrenia came to our clinic with lesions on the right breast that had appeared a year earlier. She reported a history of right breast abscess that had required drainage by her gynecologist. Since then she had had erosive lesions with erythematous-violaceous borders on the upper outer quadrant of the breast that had not improved with topical antibiotics (Fig. 2A). Cultures for bacteria, fungi, and mycobacteria were negative. A biopsy revealed a dense, mixed dermal infiltrate of plasma cells and suppurative granulomas (Fig. 2B). No microorganisms or foreign bodies were observed. Laboratory tests revealed only subclinical hypothyroidism. Following application of tacrolimus 0.1% ointment twice daily for 12 months, the lesions resolved.
SGP is a rare condition for which we found some 60 references in the literature. It usually presents on the trunk as a slow-growing, painless superficial ulcer with vegetative borders, although SGP lesions have been reported on the face, the limbs, and even the scrotum.3,4 When SGP is located on the face it is important to consider a diagnosis of Wegener disease.3 Although SGP has a more indolent course than PG and usually responds better to treatment, chronicity and recurrence are common.
SGP rarely accompanies systemic diseases, although isolated cases have been associated with chronic lymphatic leukemia, polymyalgia rheumatica, IgA paraproteinemia, sarcoidosis, rheumatoid arthritis, and ulcerative colitis.5
Histology characteristically reveals a superficial dermal abscess or ulcer which tends to form granulomas in 3 layers: a central zone with neutrophils, cellular debris, and evidence of bleeding; a surrounding layer of histiocytes and giant cells; and an outer layer of plasma cells and eosinophils.2 Although not all cases have this characteristic histology, granulomatous inflammation is a consistent finding. The presence of eosinophils, plasma cells, and granulomas and the lack of involvement of the hypodermis help differentiate SGP from PG.6 Moreover, sinus tracts and foreign bodies such as hair, suture material, and vegetable matter are usually observed in SGP but not in PG.1
In both PG and SGP, definitive diagnosis is by exclusion. Differential diagnosis should include mycobacterial and fungal infections, ulcerative sarcoidosis, foreign body granuloma, and halogenoderma.
The pathogenesis is unknown. Characteristics supporting the hypothesis that SGP has a different etiology to PG are the presence of foreign bodies and the inflammatory infiltrate composed of giant cells, plasma cells, and eosinophils, in addition to neutrophils. SGP therefore seems to be a local response of the skin to an as yet unidentified element or to a normal tissue that the disordered immune response identifies as foreign.1
The treatment of SGP is different to that of PG.7 Spontaneous healing is not unusual, although recurrence is common. SGP located on the face is more refractory to treatment.8 As in PG, surgical removal of SGP is not recommended because of the risk of pathergy. Since SGP has a more indolent clinical course than PG, aggressive treatments are not usually required in principle (Table 1). The response to topical corticosteroids is usually good, though slow.9 Good responses to topical tacrolimus have also been reported.5,10 Our positive experience with tacrolimus in 2 patients leads us to think it could be considered a first-line treatment.
In conclusion, we have presented 2 cases of SGP, an uncommon diagnosis. We emphasize the favorable response to topical tacrolimus, although complete cure took several months to achieve.
Please cite this article as: Ormaechea-Pérez N, et al. Pioderma granulomatoso superficial. Presentación de 2 casos tratados con tacrolimus tópico. Actas Dermosifiliogr. 2013;104:721–4.