Linear immunoglobulin (Ig) A dermatosis is an immune-mediated bullous disease characterized by linear deposits of IgA along the basal membrane. While usually idiopathic, it can occasionally be induced by drug exposure. We report the case of a 60-year-old woman with rheumatoid arthritis being treated with sulfasalazine who developed linear IgA dermatosis and drug rash with eosinophilia and systemic symptoms (DRESS). The dermatosis and associated symptoms resolved following withdrawal of the drug and treatment with systemic corticosteroids for 2 months. This is the first report of sulfasalazine-induced linear IgA dermatosis in association with DRESS and we believe that sulfasalazine should be added to the list of drugs that can cause linear IgA dermatosis.
La dermatosis IgA lineal es una enfermedad ampollosa mediada inmunológicamente que se define por presentar un depósito lineal de IgA a lo largo de la membrana basal. Habitualmente es idiopática y ocasionalmente se asocia con algunos fármacos. Describimos el caso de una mujer de 60 años con artritis reumatoide en tratamiento con sulfasalazina, que desarrolló un cuadro de dermatosis IgA lineal con clínica de DRESS (drug-rash with eosinophilia and systemic symptoms) el cual respondió al suspender el fármaco causal más tratamiento con corticoides sistémicos durante dos meses. Este es el primer caso descrito de dermatosis IgA lineal con clínica de DRESS relacionado con la sulfasalazina. Creemos que es importante tener en cuenta esta asociación para poder incluir a la sulfasalazina en el listado de fármacos que pueden producir dermatosis IgA lineal por fármacos.
Sulfasalazine is a sulfonamide-derived drug with anti-inflammatory properties that is used in the treatment of rheumatoid arthritis and inflammatory bowel disease. Although a maculopapular rash is the most common cutaneous reaction caused by this treatment,1 other potential reactions should not be ignored.
We treated a case of linear IgA dermatosis (LAD) secondary to sulfasalazine treatment which presented as drug-rash with eosinophilia and systemic symptoms (DRESS) in a patient with rheumatoid arthritis.
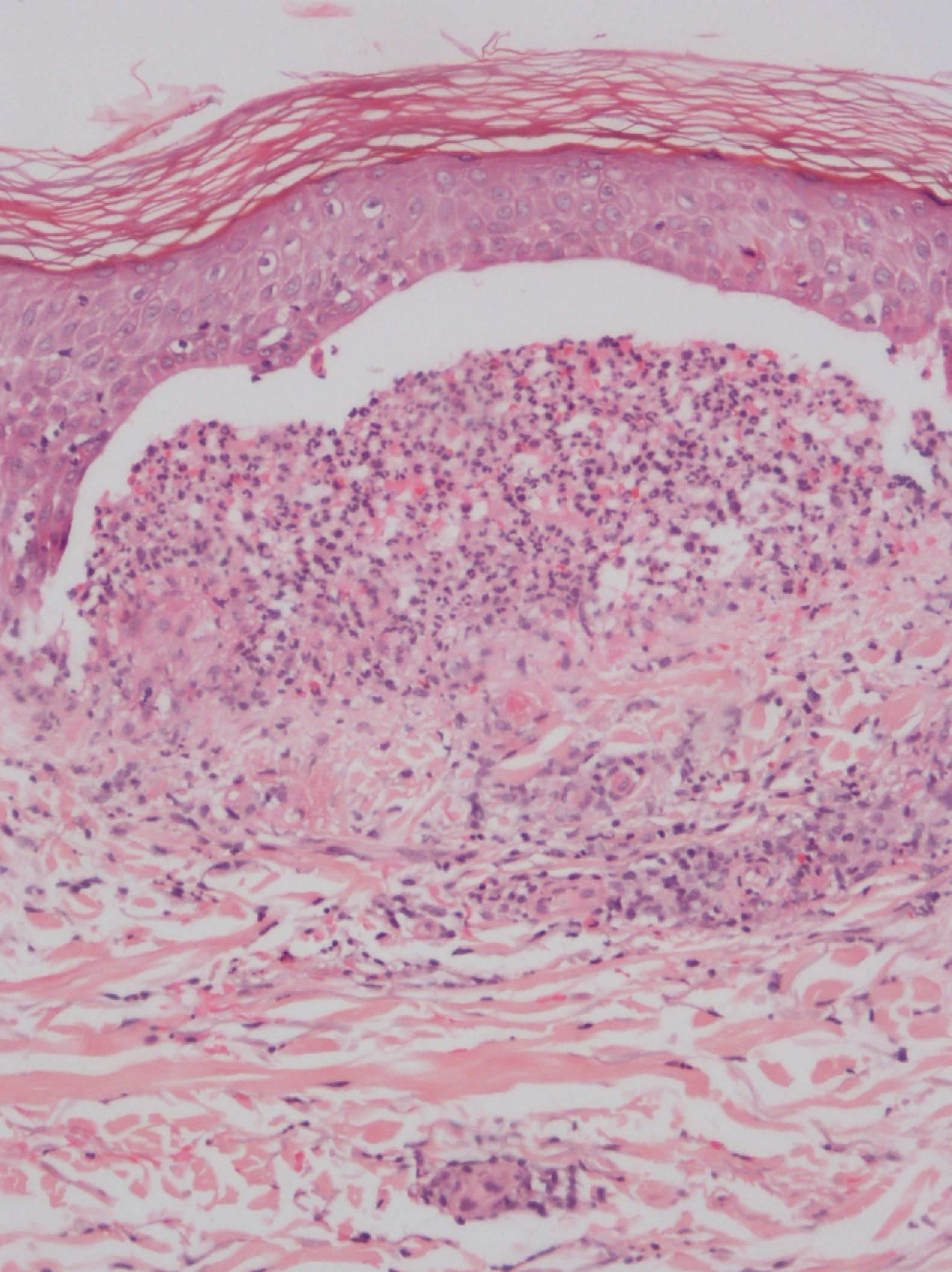
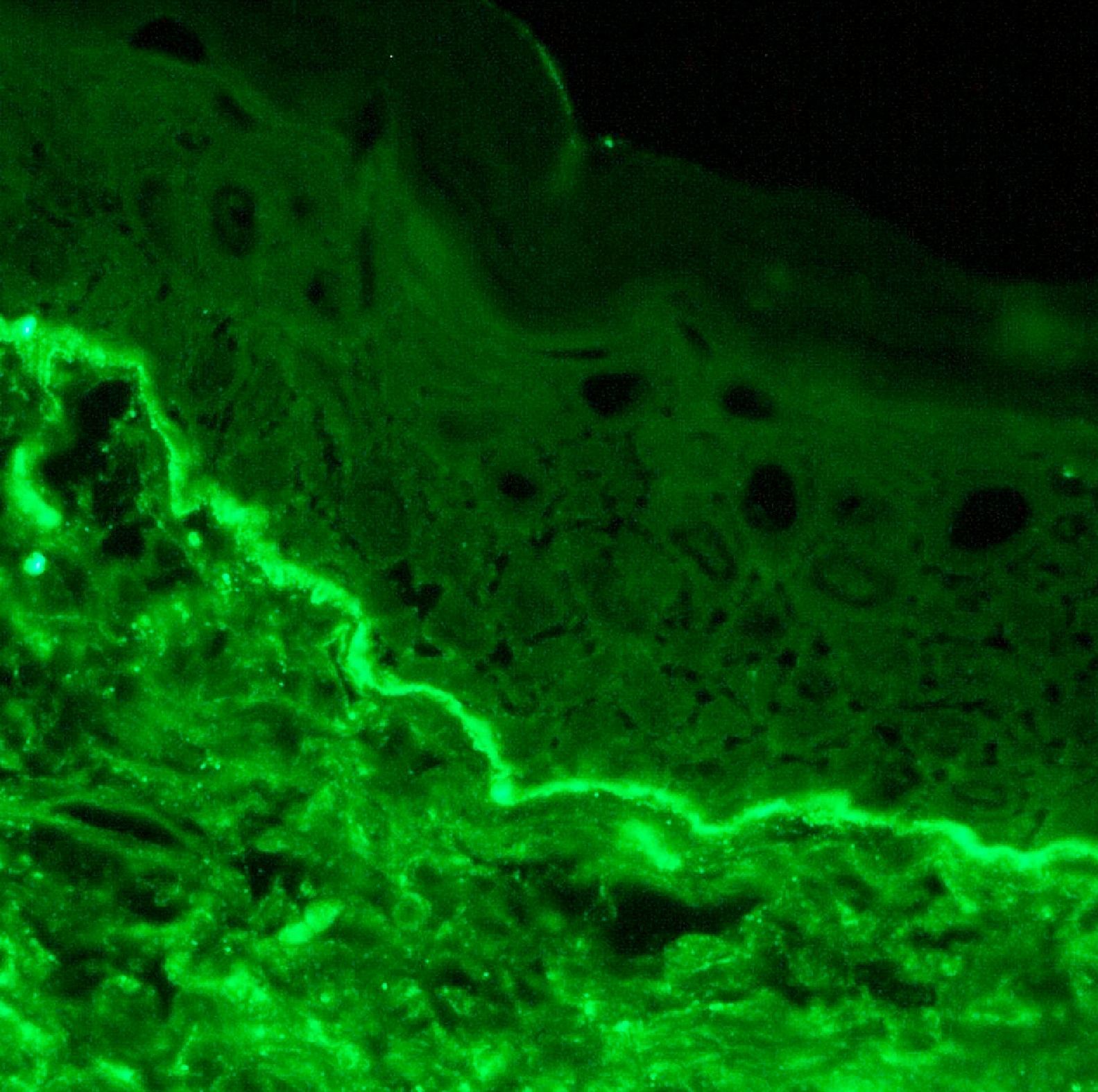
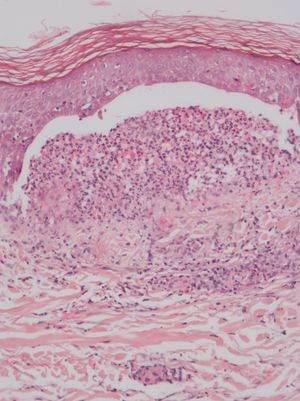
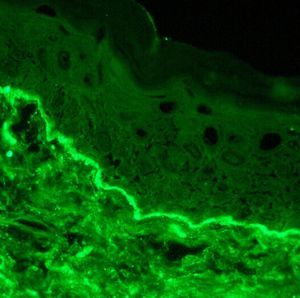
Case DescriptionThe patient was a 60-year-old woman with a history of rheumatoid arthritis, systemic hypertension, and dyslipidemia, who was receiving treatment with deflazacort (18 mg/d), diclofenac (50 mg/d), omeprazole (20 mg/d), and a combination of hydrochlorothiazide and valsartan (150/12.5 mg). She was prescribed treatment with sulfasalazine (2g/d) for joint pain. Three weeks later the patient presented to the emergency department with fever and skin lesions on the trunk and limbs that had appeared 2 weeks previously. Physical examination revealed general malaise, fever, hypotension, and tachycardia. Confluent erythematous macules and papules that formed moderately infiltrated plaques with poorly defined borders affected 70% of the body surface area. Tense blisters filled with a clear fluid were present on both legs and the dorsum of the hands (Figures 1 and 2), but the Nikolsky sign was negative. No mucosal lesions or lymphadenopathy were detected. Blood tests revealed a white blood cell count of 15 700/μL (normal range, 4500-11 000/μL) (54.5% neutrophils [normal range, 40.0%-70.0%] and 8.4% eosinophils [normal range, 0.00%-5.00%]) and eosinophilia of 1320/μL; erythrocyte sedimentation rate, 42mm/h; alanine aminotransferase, 44.5 U/L (normal range, 7-40 U/L); γ-glutamyltransferase, 452.3 U/L (normal range, 12-54 U/L); lactate dehydrogenase, 716.1 U/L (normal range, 230-460 U/L); and C-reactive protein, 9.88mg/dl. Serology for Epstein-Barr virus (EBV) was positive (IgM and IgG) and abdominal ultrasound showed no abnormal findings. Skin biopsy revealed a blister caused by dermoepidermal detachment with a neutrophil-rich infiltrate (Fig. 3) and on direct immunofluorescence there were linear deposits of IgA but not IgG or complement along the basement membrane (Fig. 4).Treatment was initiated with a tapering dose of prednisone, starting at 60mg/d, in conjunction with topical corticosteroids, with a good response. The sulfasalazine treatment was discontinued at the same time and the existing lesions improved and no new lesions were detected. The patient responded favorably with an improvement in her general health and normalization of laboratory parameters. The skin lesions disappeared completely within 2 months. After 3 years of follow-up, the patient is asymptomatic and receiving no treatment.
We report the case of a woman with LAD and DRESS syndrome secondary to sulfasalazine administration. No other changes had been made to the patient's treatment regimen; the initiation of sulfasalazine treatment 3 weeks before the onset of symptoms and the linear deposits of IgA but not of IgG or complement suggest that this drug was the most likely cause. Moreover, fever, hypertension, tachycardia, elevated transaminase levels, and eosinophilia are inclusion criteria for the diagnosis of DRESS in hospitalized patients.2
LAD is an immune-mediated blistering disease, characterized by the presence of linear IgA deposits along the basement membrane. This condition is often idiopathic and is occasionally associated with drug treatment,3,4 inflammatory bowel disease,5 or lymphoid tumors.6 The association of LAD with gluten-sensitive enteropathy7 and rheumatoid arthritis8 has also been described in isolated cases.
Drug-induced LAD can be indistinguishable from the clinical features of classical LAD, as it is characterized by the development of an erythematous plaque surrounded by vesicles or blisters, giving the appearance of a “string of pearls”. However, the skin lesions are generally more polymorphic, and cases of erythema multiforme and toxic epidermal necrolysis with dissemination of bullous lesions and mucosal involvement have been described.3,9 The lesions can be asymptomatic or pruritic and are most commonly found on the trunk, limbs, and acral areas. The symptoms usually appear between 24hours and 15 days after starting treatment with the causative drug, and the formation of new lesions ceases 24 to 72hours after discontinuation of the treatment. Resolution of the lesions occurs on average within 2 months. Mucosal involvement has been reported in approximately 40% of cases, as compared with 80% of cases of classical LAD.4 Direct immunofluorescence in classical LAD reveals linear deposits of IgA along the basement membrane, accompanied by IgG deposits in over 30% of cases. In drug-induced DAL, only linear IgA deposits are observed in the basement membrane, accompanied by complement (C3) in 20% of cases.4 There are no clinical or immunofluorescence patterns to differentiate with certainty between classical and drug-induced LAD.
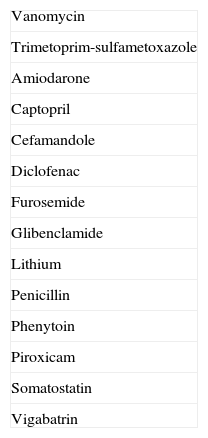
Vancomycin is the drug most commonly associated with LAD secondary to drug administration.3,4,10,11 Other causative antibiotics include second generation cephalosporins, penicillin derivatives, and trimetoprim-sulfametoxazole (Table 1).4,11
In the present case, the patient was receiving chronic treatment with diclofenac/misoprostol, deflazacort, omeprazole, and a combination of hydrochlorothiazide and valsartan; this regimen was maintained after the remission of symptoms.
NSAID-induced LAD has only been described in isolated cases among patients treated with diclofenac12 or piroxicam.13 Although we cannot rule out a link between LAD and the other treatments administered to our patient, sulfasalazine seems the most likely causative drug, based on the chronology of events.
A review of the literature revealed no cases of sulfasalazine-induced LAD, although a link has been reported between LAD and trimetoprim-sulfametoxazole,11,12 another sulfonamide-derived molecule.
Sulfasalazine is a sulfonamide derivative that inhibits the synthesis of dihydrofolic acid by the intestinal flora. In the digestive tract, sulfasalazine is broken down into 2 metabolites: 5-aminosalacyclic acid and sulfapyridine. Sulfapyridine is rapidly absorbed and is hydroxylated and acetylated in the liver, with subsequent excretion in the urine. The rate of acetylation in the liver is genetically determined and slow acetylators are at increased risk of adverse reactions, such as hypersensitivity syndrome.14
DRESS is characterized by skin rash, fever, lymphadenopathy, and systemic involvement. The REGISCAR group has suggested several inclusion criteria for hospitalized patients, including skin rash and at least 3 of 4 systemic symptoms (fever, lymphadenopathy, internal organ involvement, and abnormal complete blood count).2 Reactivation of human herpesvirus type-6 and Epstein-Barr virus has also been associated with DRESS.2,15
It is not known whether rheumatoid arthritis alone can be associated with LAD. Hayakawa et al.8 described the case of a 65-year-old woman with a 6-year history of rheumatoid arthritis who developed LAD, but did not state which drugs were prescribed to treat the patient's arthritis. The authors suggest that the overproduction and increase action of cytokines in arthritis could give rise to immune dysregulation that triggers this condition, but they conclude that this association cannot be confirmed and may have been an incidental finding.
To the best of our knowledge this is the first case reported in the literature of sulfasalazine-induced LAD with clinical features of DRESS. We believe it is important to recognize this association and to include sulfasalazine in the list of drugs that can cause drug-induced LAD.
Conflict of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Hernández N, et al. Dermatosis ampollosa inducida por inmunoglobulina A lineal con clínica de síndrome DRESS por sulfasalazina. Actas Dermosifiliogr. 2013;104:343–6.