White sponge nevus (WSN) is a rare and benign disease that usually affects the oral mucosa and manifests as white spongy plaques. Because it is usually clinically asymptomatic, treatment of WSN is focused on improving the aesthetics and texture of the mucosa.1 Given the low prevalence of this condition, description of the available therapeutic options is limited to isolated clinical case reports and short cases series.
A 46-year-old male non-smoker with no relevant personal history was seen for oral lesions that had been present since childhood. Clinical examination revealed bilateral, whitish, soft plaques that were located on the buccal mucosa and the lateral aspects of the tongue and remained adhered after scraping (Fig. 1A and B). The patient had no similar lesions in other locations and reported no relevant family history. Although the lesions were asymptomatic, they had a significant aesthetic impact on the patient. A biopsy of one of the lesions on the buccal mucosa revealed epithelial hyperplasia, edema, and discrete cytoplasmic clearance in squamous cells. Taken together with the clinical context, these findings were compatible with WSN.
Treatment for 2 months with topical triamcinolone acetonide (0.1%) and retinoic acid (0.1%) in oral adhesive excipient resulted in no clinical improvement, and it was decided to begin treatment with oral doxycycline (100 mg/d) for 6 weeks. The extension and texture of the lesions improved by the end of the treatment cycle, providing an acceptable aesthetic result, and the patient remained stable for the next 6 months (Fig. 1C and D).
WSN is a rare, autosomal dominant disease with incomplete penetrance, despite isolated reports of cases with no family history.1,2 It was first described by Hyde in 1909.1 Clinically, it is characterized by bilateral, well-defined, villous white plaques with a spongy texture, usually located on the oral mucosa, often with involvement of the bite line and the anterior third of the buccal mucosa.1,3 It usually manifests during childhood or adolescence, with no sexual predisposition, and the lesions tend to remain stable throughout life. Histology shows acanthosis with intercellular edema and vacuolization, as well as parakeratotic or orthokeratotic hyperkeratosis in the superficial layers.4,5 Diagnosis is based on clinical–pathological correlation and, where possible, analysis of mutations in keratin 4 (KRT4) and keratin 13 (KRT13), genes responsible for epithelial keratinization.1 The differential diagnosis should primarily include oral candidiasis, frictional leukokeratosis, leukoedema, leukoplakia, and lichen planus.1,2
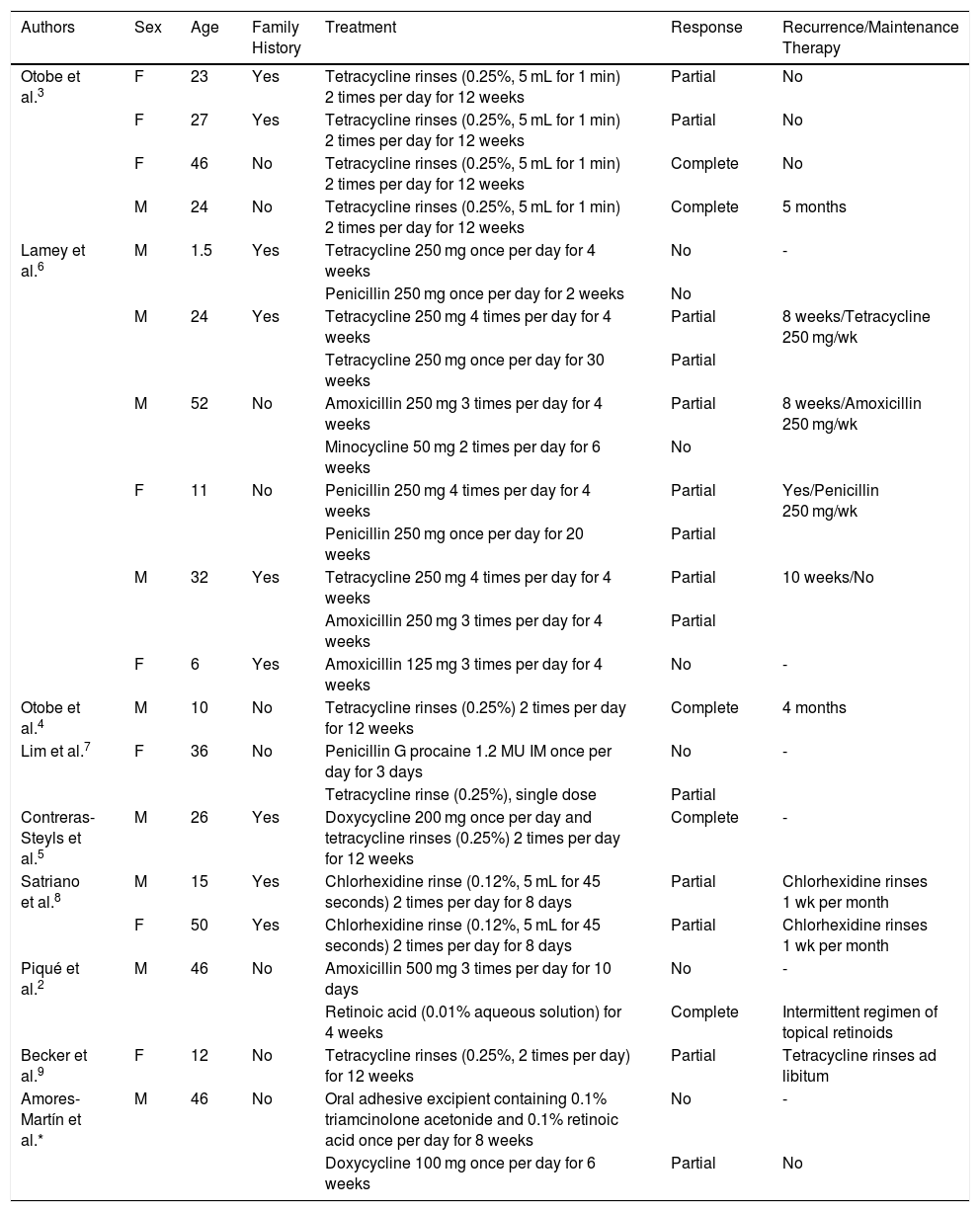
Although WSN is a benign and asymptomatic disease, its effects on mucosa texture and aesthetics are a source of discomfort for many patients. Multiple treatments have been tested for WSN (Table 1). Some have proven of little benefit, producing variable results, and there is no well-defined therapeutic protocol.
Published Cases of White Sponge Nevus: Therapeutic Guidelines, Clinical Responses, and Recurrences
| Authors | Sex | Age | Family History | Treatment | Response | Recurrence/Maintenance Therapy |
|---|---|---|---|---|---|---|
| Otobe et al.3 | F | 23 | Yes | Tetracycline rinses (0.25%, 5 mL for 1 min) 2 times per day for 12 weeks | Partial | No |
| F | 27 | Yes | Tetracycline rinses (0.25%, 5 mL for 1 min) 2 times per day for 12 weeks | Partial | No | |
| F | 46 | No | Tetracycline rinses (0.25%, 5 mL for 1 min) 2 times per day for 12 weeks | Complete | No | |
| M | 24 | No | Tetracycline rinses (0.25%, 5 mL for 1 min) 2 times per day for 12 weeks | Complete | 5 months | |
| Lamey et al.6 | M | 1.5 | Yes | Tetracycline 250 mg once per day for 4 weeks | No | - |
| Penicillin 250 mg once per day for 2 weeks | No | |||||
| M | 24 | Yes | Tetracycline 250 mg 4 times per day for 4 weeks | Partial | 8 weeks/Tetracycline 250 mg/wk | |
| Tetracycline 250 mg once per day for 30 weeks | Partial | |||||
| M | 52 | No | Amoxicillin 250 mg 3 times per day for 4 weeks | Partial | 8 weeks/Amoxicillin 250 mg/wk | |
| Minocycline 50 mg 2 times per day for 6 weeks | No | |||||
| F | 11 | No | Penicillin 250 mg 4 times per day for 4 weeks | Partial | Yes/Penicillin 250 mg/wk | |
| Penicillin 250 mg once per day for 20 weeks | Partial | |||||
| M | 32 | Yes | Tetracycline 250 mg 4 times per day for 4 weeks | Partial | 10 weeks/No | |
| Amoxicillin 250 mg 3 times per day for 4 weeks | Partial | |||||
| F | 6 | Yes | Amoxicillin 125 mg 3 times per day for 4 weeks | No | - | |
| Otobe et al.4 | M | 10 | No | Tetracycline rinses (0.25%) 2 times per day for 12 weeks | Complete | 4 months |
| Lim et al.7 | F | 36 | No | Penicillin G procaine 1.2 MU IM once per day for 3 days | No | - |
| Tetracycline rinse (0.25%), single dose | Partial | |||||
| Contreras-Steyls et al.5 | M | 26 | Yes | Doxycycline 200 mg once per day and tetracycline rinses (0.25%) 2 times per day for 12 weeks | Complete | - |
| Satriano et al.8 | M | 15 | Yes | Chlorhexidine rinse (0.12%, 5 mL for 45 seconds) 2 times per day for 8 days | Partial | Chlorhexidine rinses 1 wk per month |
| F | 50 | Yes | Chlorhexidine rinse (0.12%, 5 mL for 45 seconds) 2 times per day for 8 days | Partial | Chlorhexidine rinses 1 wk per month | |
| Piqué et al.2 | M | 46 | No | Amoxicillin 500 mg 3 times per day for 10 days | No | - |
| Retinoic acid (0.01% aqueous solution) for 4 weeks | Complete | Intermittent regimen of topical retinoids | ||||
| Becker et al.9 | F | 12 | No | Tetracycline rinses (0.25%, 2 times per day) for 12 weeks | Partial | Tetracycline rinses ad libitum |
| Amores-Martín et al.* | M | 46 | No | Oral adhesive excipient containing 0.1% triamcinolone acetonide and 0.1% retinoic acid once per day for 8 weeks | No | - |
| Doxycycline 100 mg once per day for 6 weeks | Partial | No |
Abbreviations: F, female; IM, intramuscular; MU, million units; M, male.
Partial and complete responses have been described in patients treated with topical tetracyclines. The best results have been described in patients treated with 0.025% tetracycline rinses 2 times per day for 12 weeks. However, good responses have been reported in 2 cases treated with oral tetracyclines, in line with our findings. The paucity of publications makes it difficult to establish the best route of tetracycline administration. In WSN, the beneficial effect of second-generation tetracyclines such as doxycycline and minocycline can be attributed both to their anti-inflammatory effects and their modulation of epithelial keratinization.1 These properties constitute an advantage over tetracycline.10
Although WSN is not considered of microbiological origin, most of the treatments for which good outcomes have been reported to date are antimicrobial therapies, including oral and topical antibiotics and antiseptics such as chlorhexidine.8 This suggests that certain microorganisms may play a role in disease expression in genetically predisposed individuals. However, further evidence is required to support this hypothesis.
Analysis of therapeutic response as a function of a family history of WSN suggests that the absence of a family history does not greatly increase the likelihood of a response to treatment, but is associated with a greater clinical response.
The new WSN case presented here, in which the patient showed a satisfactory clinical response to oral doxycycline (100 mg/d for 6 weeks), provides additional data on the use of oral tetracyclines to treat this condition. We believe it is important to have a knowledge of the clinical evidence supporting the different treatments used to date to ensure selection of the most appropriate therapies for these patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Amores-Martín E, Melé-Ninot G, Del Alcázar Viladomiu E, Fernández-Figueras MT. Tratamiento del nevus blanco esponjoso. Aportación de un caso con respuesta a doxiciclina oral y revisión de la literatura. Actas Dermosifiliogr. 2021;112:463–466.