Genital leiomyomas are the least common type of leiomyomas and those located on the nipple or areola are extremely rare.1–4 To date, their treatment with carbon dioxide (CO2) laser has not been reported in the literature.
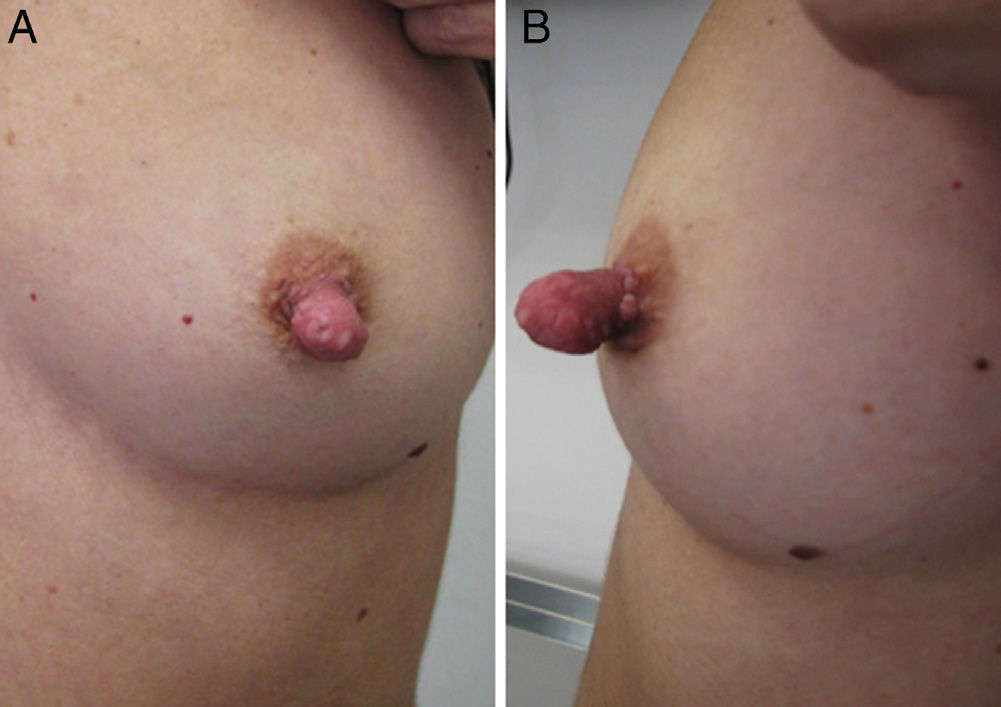
We describe the case of a 33-year-old woman with no relevant past medical history who presented with a skin lesion on the left nipple; the lesion had been stable since its appearance in adolescence. The patient reported mild tenderness and great impact on personal appearance as the reasons for seeking treatment. The examination revealed elongation of the left nipple secondary to the presence of a well-defined, firm nodular lesion that was the same color as the nipple and about 15mm in diameter; there were no signs of nipple retraction (Fig. 1). The rest of the left breast and the right breast revealed no significant findings.
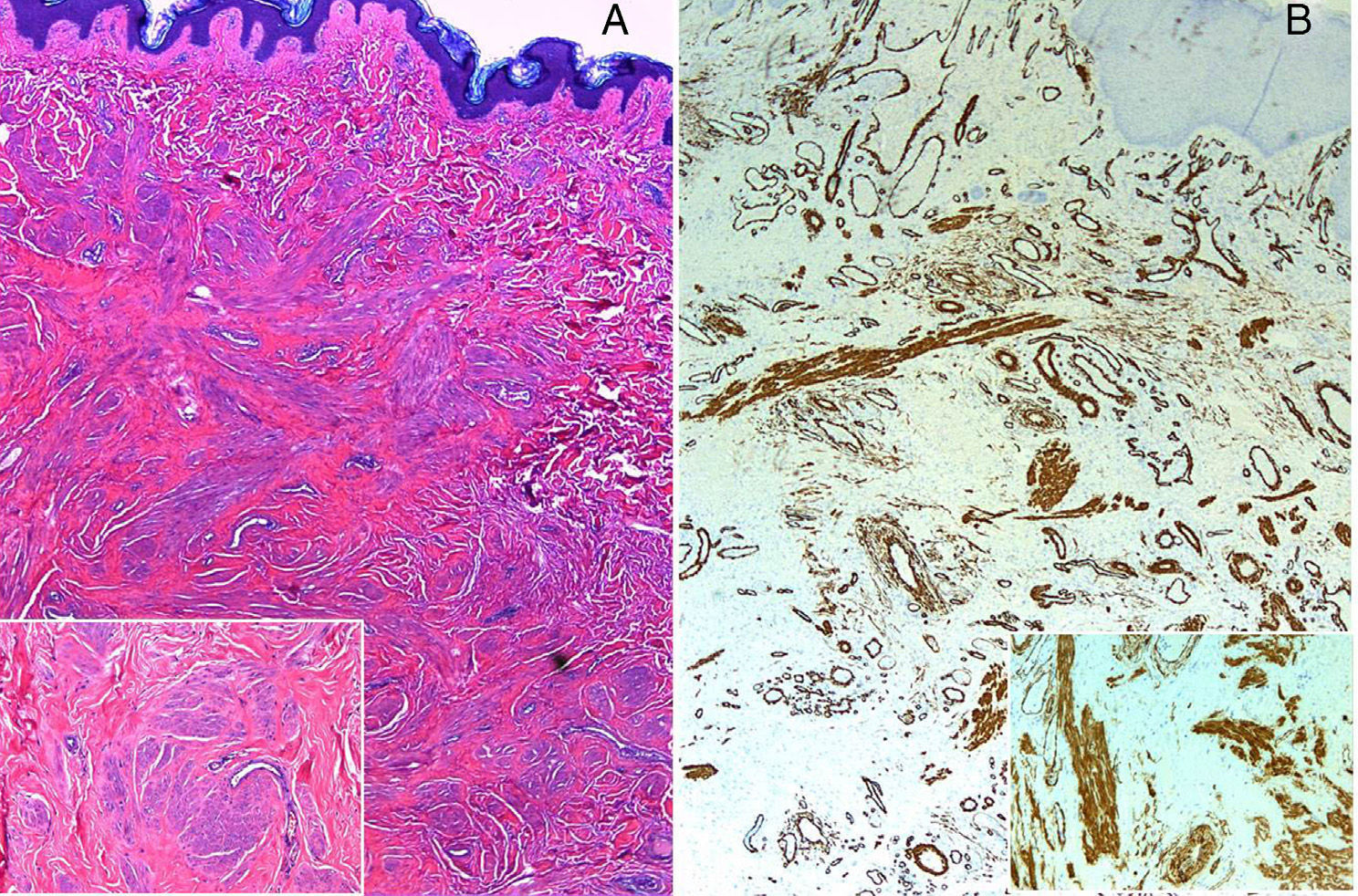
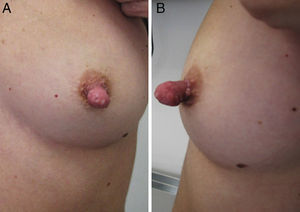
Histopathology of the lesion revealed a hyperkeratotic epidermis with increased pigmentation of the basal layer and, in the dermis, the presence of a poorly defined, unencapsulated tumor composed of multiple interwoven bundles of smooth muscle formed by cells with ovoid nuclei and eosinophilic cytoplasm (Fig. 2A). No atypical cells or mitoses were observed. Staining for smooth muscle actin was positive (Fig. 2B). In view of these clinical and histologic findings, the lesions was diagnosed as a genital leiomyoma. Under local anesthesia with mepivacaine 2%, the rest of the lesion was removed with a Sharplan CO2 laser in unfocused mode with an irradiance of 55W/cm2 and a spot size of 3mm. The lesion was treated in a single session with 5 to 8 passes; between each pass the coagulated tissue was removed until there was no visible sign of the leiomyoma. After 1 treatment session much of the lesion had been removed with good cosmetic and functional results. No recurrence was detected 20 months after treatment (Fig. 3).
A, Hyperkeratotic epidermis under which there is an unencapsulated dermal tumor composed of interwoven bundles of eosinophilic spindle cells (hematoxylin-eosin, original magnification ×100; inset, further magnification ×5). B, Positive staining for smooth muscle actin (hematoxylin-eosin, original magnification ×100; inset, further magnification ×5).
Cutaneous leiomyomas are rare, benign tumors. They are classified into 3 categories according to the muscle fibers from which they originate: piloleiomyoma, originating from the smooth muscle fibers of the arrector pili muscle; angioleiomyoma, originating from the tunica media of the blood vessels; and dartoic or genital leiomyoma, originating from the smooth muscles of the scrotum, vulva, nipple, or areola. Genital leiomyomas are the least common type and those located on the nipple or areola are extremely rare.1–4 Leiomyomas of the nipple and areola, first described in 1854 by Virchow, present as small, solitary nodular lesions covered with healthy skin that can exceptionally cause nipple retraction and spread to the underlying breast tissue.4 The lesions are usually asymptomatic but in rare cases can cause pain spontaneously or in response to stimuli such as cold, pressure, or emotional stress.
Histologically, they are poorly defined, unencapsulated skin tumors composed of bundles of spindle cells with abundant eosinophilic cytoplasm and elongated nuclei with blunt ends, arranged in an interwoven pattern. The epidermis is usually unaffected because it is separated from the tumors by a free zone of dermis; cellular mitosis and atypia are rare.2 Leiomyomas are positive for vimentin, desmin, and smooth muscle actin.
Differential diagnosis with the following diseases should be considered: Paget disease, fibroma, adenoma of the nipple, lymphadenosis benigna cutis, leiomyosarcoma of the areola, erosive adenomatosis of the nipple, and myoid hamartoma.2
Several treatment modalities are used. In cases involving pain it can be useful to use calcium channel blockers or α–blockers, which inhibit contraction of muscle fibers. Isolated cases have been treated with cryotherapy, nitroglycerin, hyoscine hydrobromide, lidocaine, and analgesics.5 In addition to medical treatment, surgical excision is also an option. However, surgery is sometimes contraindicated because of patient factors or because the lesions, as in our patient, are located in areas that require a good cosmetic result. CO2 laser removal has been used to treat cutaneous leiomyoma with good results,5 but to date no cases of genital leiomyoma treated with this modality have been reported. CO2 laser emits light in the infrared spectrum at a wavelength of 10 600nm, which is absorbed by water. The laser vaporizes the skin and causes coagulative necrosis in the remaining dermis. CO2 laser treatment is advantageous mainly because the procedure is rapid and enables precise selection of tissue. The technique is safe, as tissue damage is specific, with highly localized destruction, minimal damage to surrounding tissue, and minimal bleeding because it promotes coagulation. An alternative to the CO2 laser is the erbium-doped yttrium aluminum garnet (Er:YAG) laser, which emits light in the infrared spectrum at a wavelength of 2900nm and can vaporize the skin at a lower penetration depth than the CO2 laser. The Er:YAG laser produces little thermal damage to the underlying tissue because of its high water absorption coefficient. However, this effective absorption limits the transmission of heat to the deep layers, where it may be insufficient to promote coagulation and prevent bleeding during surgery.
In conclusion, we have presented a case of a rare disease in which CO2 laser treatment provided very satisfactory cosmetic results. We believe that this technique can be considered a good option in cases in which surgery is not possible or is contraindicated.
Please cite this article as: López V, López I, Alcacer J, Ricart JM. Buenos resultados tras tratamiento con láser CO2 de leiomioma en el pezón. Actas Dermosifiliogr. 2013;104:928–930.