A 12-year-old girl with no relevant past history presented with a lesion on the lateral portion of the right eyebrow that had appeared 2 months earlier. The patient had no history of trauma. She reported occasional pain and an increase in the size of the lesion, followed by stabilization.
Physical ExaminationPhysical examination revealed an ill-defined oval-shaped subcutaneous growth measuring 2cm in diameter, with a firm elastic consistency, adherent to the deeper tissues, with no alterations of the underlying skin (Figure 1).
Additional TestsRadiographs of the face, orbit, superior orbital fissure, and skull were normal. Soft-tissue ultrasound revealed a solid, rounded growth with some small vessels in the subcutaneous cellular tissue (Figure 2).
Clinical Course and TreatmentThe lesion was completely excised, and after 8 months of follow-up there were no signs of local recurrence and no other lesions had appeared.
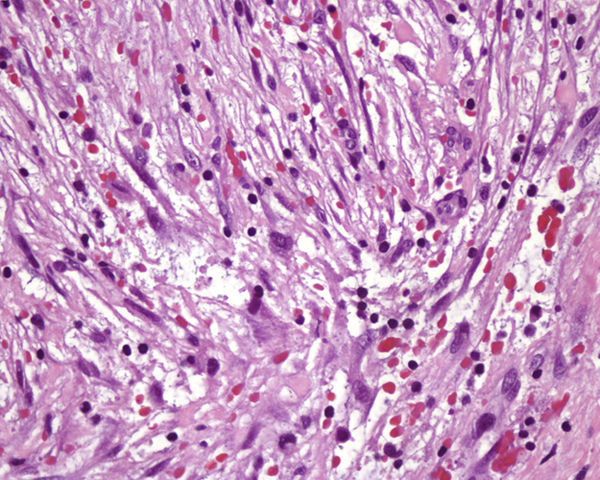
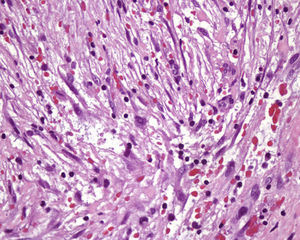
HistopathologyHistologic examination revealed a localized growth in the subcutaneous cellular tissue formed by a proliferation of multipolar spindle-shaped fibroblasts and myofibroblasts with vesicular nuclei and prominent nucleoli, arranged in a non-specific pattern in a myxoid stroma with extravasated blood cells and fibrous areas with hyalinized collagen (Figure 3, hematoxylin-eosin, original magnification×400).
What Is Your Diagnosis?
DiagnosisNodular fasciitis (NF).
CommentNF was first described by Konwaler et al. in 1954 as “subcutaneous pseudosarcomatous fibromatosis (fasciitis).”1 It is a fast-growing proliferative lesion that mainly affects the subcutaneous cellular tissue, fascia, and muscle, although a rare dermal variant also exists.2 The etiology and pathogenesis of NF remain uncertain, although it is considered to be a reactive, benign, self-limiting process2–4 related, in isolated cases, to infectious processes or trauma.2 It usually appears in white men3 in the third or fourth decades of life2; only 10% of cases are found in children anywhere from several months to 18 years of age, with the average age falling between 8 and 14 years, depending on the case series.3–5 The most common site of NF lesions is the extremities and trunk, followed by the head and neck, the most frequent site during childhood,4,5 although reports of NF in children are rare.3,5 NF usually presents as a single asymptomatic lesion. Clinically, NF is characterized by a firm nodule, either fixed or mobile, that is generally less than 3cm in diameter, skin-colored or erythematous, sometimes painful, and without palpable lymph nodes.1,3,4
NF is diagnosed histopathologically. Presurgical imaging studies help to better define the lesion and rule out other possible diagnoses.4
Histologic examination shows a proliferation of fibroblasts and myofibroblasts with an increase in mitotic activity and loose myxoid stroma,2,3 with increased vascularization, extravasated erythrocytes, chronic inflammatory infiltrate2,4 and occasional osteoclastic giant cells. Price et al. were the first to classify NF in 3 histologic subtypes: myxoid or reactive (type i, the most common type), cellular (type ii), and fibrous (type iii). It has been suggested that these subtypes may not be independent but rather that they represent the progression of NF over time.2 Immunohistochemical studies are positive for muscle-specific actin, smooth muscle actin, calponin, and vimentin and negative for desmin, cytokeratin, h-caldesmon, smooth muscle myosin, S100 protein, and CD34.3,5,6 As in other mesenchymal tumors, cytogenetic studies have revealed rearrangements of the USP6 locus related to high mitotic activity.4
The clinical differential diagnosis includes benign lesions such as dermoid or epidermoid cysts, pilomatricoma, lipoma, and postoperative or posttraumatic nodules, as well as malignant tumors1–5 such as fibrosarcoma, malignant peripheral nerve sheath tumor, undifferentiated pleomorphic sarcoma, and dermatofibrosarcoma protuberans.
Despite its reactive character and the possibility of spontaneous remission, surgical excision appears to be the most reasonable form of management, especially in children.5 Recurrences are rare and require that the diagnosis be reconsidered.2–5
Please cite this article as: García-Montero PP. Tumoración subcutánea en la cola de la ceja derecha. Actas Dermosifiliogr. 2017;108:253–254.