The patient was a 76-year-old woman with no personal history of interest who consulted for a nodular lesion measuring 2cm on her right buttock. The lesion had first appeared 1 year previously, had gradually increased in size, and was accompanied by an adjacent satellite nodule. Both lesions were firm in consistency with an infiltrated subcutaneous base (Fig. 1).
DiagnosisPrimary cutaneous marginal zone B-cell lymphoma.
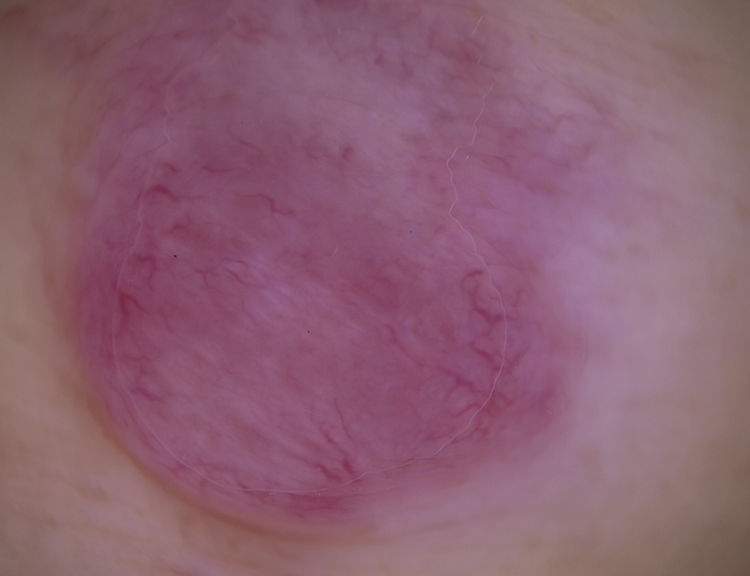
CommentDermoscopy revealed a homogeneous salmon-pink nodule with poorly focused prominent linear-irregular vessels distributed mainly on the periphery (Fig. 2). Poorly defined whitish structures were visible in the center of the lesion. There was no desquamation, pigmented base, or ulceration.
Suspicion of cutaneous lymphoma, cutaneous metastasis, amelanotic melanoma, or soft tissue sarcoma prompted us to remove the lesion. Histology revealed a diffuse nodular lymphocytic infiltrate separated from a preserved epidermis by a Grenz zone. Immunohistochemistry revealed positive results for CD20, CD79a, Bcl2, and κ light chain restriction. Together with clonal rearrangement of the IGH gene in polymerase chain reaction, these findings confirmed the diagnosis of cutaneous marginal zone B-cell lymphoma. The absence of findings in the extension study confirmed the mainly cutaneous origin.
Cutaneous lymphomas comprise a heterogeneous group of malignant neoplasms with very diverse clinical and histopathological manifestations.1,2 Therefore, diagnosis is usually complicated, and the lesion may go undetected in the initial phases, even for clinical experts.3 While diagnosis must be confirmed by biopsy and immunohistochemistry, some recent studies indicate that dermoscopy is a useful tool in the initial suspected diagnosis.3–5
In 2018, Geller et al.3 reported on the dermoscopic features of a series of 58 cutaneous B-cell lymphomas. The most frequent findings were a homogeneous salmon-pink color (79.3%) and prominent blood vessels (77.6%) that were of serpentine (linear-irregular) morphology (67.2%). The salmon pink color is thought to be associated with the lymphocytic infiltration and increased vascular flow, whereas the prominent blood vessels are associated with the angiogenesis that accompanies the neoplasm. It is noteworthy that in this study we did not record significant differences in dermoscopy findings between the various B-cell lymphoma histologic subtypes (follicle-center, marginal zone, and diffuse large B-cell) or depending on the anatomic location.
The most common clinical differential diagnosis in this series was with basal cell carcinoma (in up to 17.4% of cases), squamous cell carcinoma, dermatofibrosarcoma protuberans, cutaneous metastasis, melanoma, cysts, and arthropod bite. Strikingly, agreement between the 2 observing dermoscopy experts was relatively low for the 17 histologically confirmed cases, thus demonstrating the low specificity of these findings.3
In conclusion, we believe that the presence of homogeneous salmon-pink areas and prominent linear-irregular blood vessels in pink nodules should lead us to consider cutaneous lymphoma as a possible diagnosis, although these findings are not completely confirmatory.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez-Lomba E, Lozano-Masdemont B, Avilés-Izquierdo JA. Nódulo rosado de lento crecimiento en glúteo Eczema y urticaria en Portugal. 2019;110:763–764.