Scombroid poisoning is a common cause of food poisoning worldwide. It is caused by ingestion of oily fish contaminated with bacteria that trigger the formation of high concentrations of histamine. Scombroid poisoning manifests mainly as a skin complaint (flushing that spreads downward and/or an erythematous urticarial rash affecting the face and upper trunk). Although the clinical course is usually self-limiting and benign, vascular compromise, bronchospasm, and arrhythmias have been described. It is important to establish a differential diagnosis that includes conditions such as fish allergy. Oral antihistamines are the mainstay of treatment. Scombroid poisoning is best prevented by refrigerating fish properly. The practical review of scombroid poisoning provided here is intended for dermatologists.
La escombroidosis es una causa frecuente de intoxicación alimentaria a nivel mundial que se debe a la ingesta de pescado azul contaminado con bacterias que inducen la formación de grandes cantidades de histamina. Clínicamente se manifiesta sobre todo a nivel cutáneo, en forma de flushing descendente y/o rash eritemato-urticariforme facial y en el tronco superior. Aunque habitualmente tiene un curso autolimitado y benigno, pueden existir casos de compromiso vascular, broncoespasmo y arritmias. Es importante hacer un correcto diagnóstico diferencial, entre otros con la alergia al pescado. El tratamiento se basa en la administración de antihistamínicos orales. Lo más importante es su prevención mediante una correcta refrigeración del pescado. Este trabajo es una revisión práctica de la escombroidosis orientada para su uso por el dermatólogo.
Scombroid poisoning, also known as histamine fish poisoning, is a histamine toxicity syndrome first described in the United Kingdom in 1799.1 It is a common cause of food poisoning worldwide and is triggered by the ingestion of contaminated oily fish. Although the true incidence of scombroid poisoning is unknown in Spain, this country would be considered a risk area because of its high levels of fish consumption. The condition typically presents with skin manifestations in the form of flushing and/or a urticarial rash.
Patients with scombroid poisoning typically seek medical attention for their symptoms in primary care centers or emergency departments, although because the condition is mild and self-limiting, it is probably safe to assume that a considerable proportion of patients do not visit a doctor. Accordingly, and also because scombroid poisoning is frequently confused with a food allergy, many cases are not reported and it is probably underdiagnosed.2 The aim of this article is to provide a practical overview of scombroid poisoning and to guide dermatologists in its diagnosis and treatment, as it is not unusual for us to be called on to evaluate the skin lesions seen with this syndrome.
EpidemiologyScombroid poisoning exists around the world. Its incidence is unknown, and reported rates vary enormously from one area to the next depending on fish consumption habits. An estimated annual incidence of between 2 and 5 cases per 1 million inhabitants has been reported for Denmark, New Zealand, France, and Finland, while rates for Hawaii have been as high as 31 cases per 1 million inhabitants a year.3 The largest numbers of cases have been reported in Japan, the United Kingdom, the United States, and Australia.4 In the United States and Europe, scombroid poisoning accounts for up to 40% of all food poisoning outbreaks.3
Scombroid poisoning typically affects groups of diners who have eaten contaminated oily fish. It has traditionally been linked to the consumption of fish from the Scombroidae and Scomberesocidae family, such as tuna fish (responsible for over 80% of cases), mackerel, and bonito. Cases, however, have also been linked to other types of fish, such as anchovies, greater amberjack fish, swordfish, herring, sardines, salmon, trout, and even dolphin and Swiss cheese.3
PathogenesisScombroid, or histamine fish, poisoning, is caused by the ingestion of poorly conserved fish, i.e., fish that has generally been stored at a temperature of above 4°C. These conditions favor the growth of different bacteria, triggering the conversion of histidine (present in the meat of oily fish) to histamine by bacterial enzymes,3,4 namely histidine decarboxylase. The conversion takes place in a matter of hours, such that fish stored at 20°C can accumulate toxic levels of histamine in just 2hours. Levels of over 50mg of histamine per 100g of fish are necessary to trigger the clinical manifestations of scombroid poisoning.4 (Histamine levels in fresh fish are less than 0.01mg/100 g.) The most commonly implicated bacterial agent is Escherichia coli, although there have been cases attributed to bacteria from the species Vibrio, Proteus, Serratia, Enterobacter, Klebsiella, Clostridium, Salmonella, and Shigella. Histamine poisoning generally affects fresh fish rather than canned fish,5 as the latter is typically subject to more quality controls and cans generally contain different specimens of fish, meaning that the toxic effect of a single contaminated specimen would be minimized. Although the canning process can destroy the bacteria, it cannot destroy histamine that has already formed.
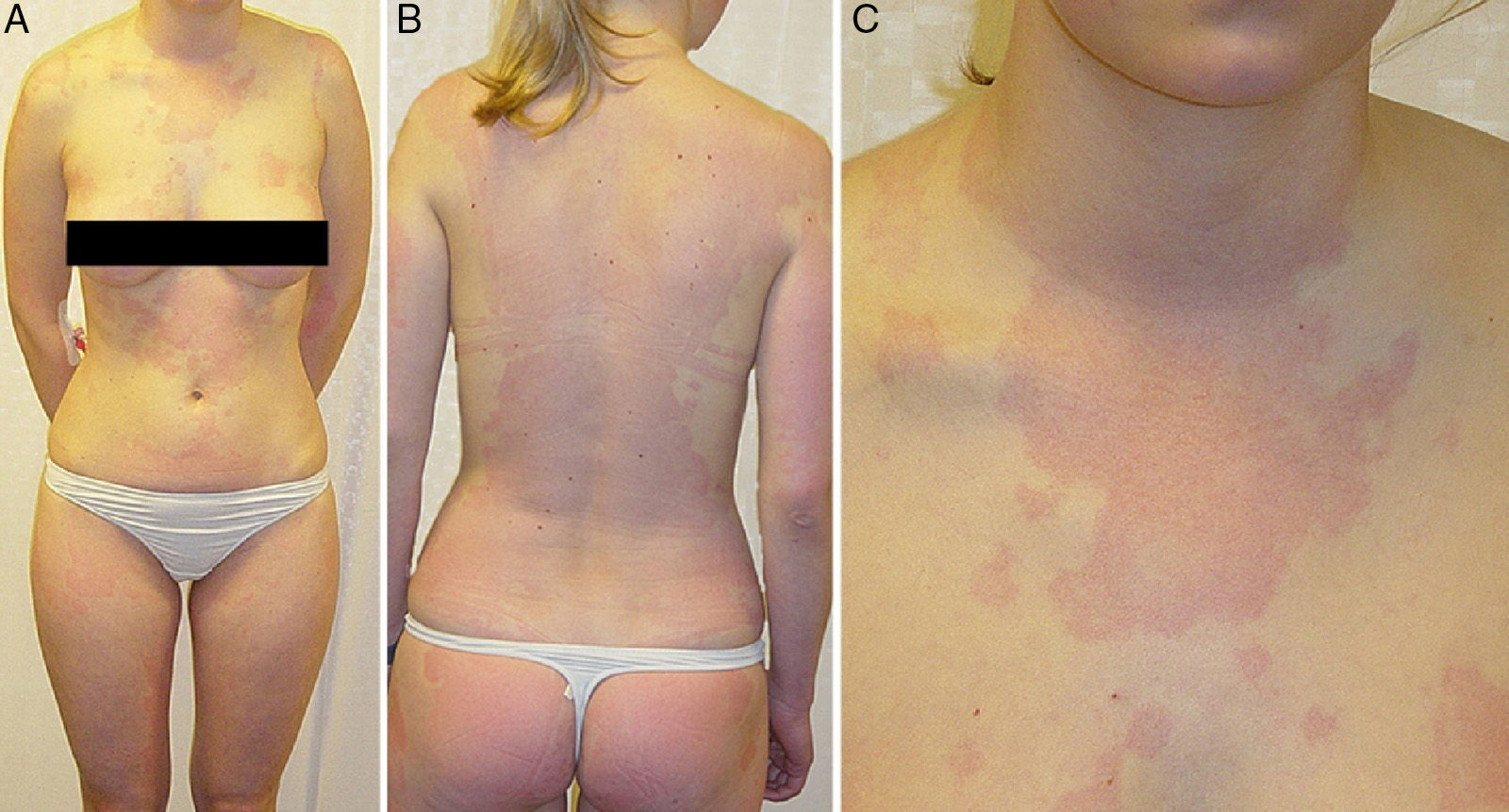
Clinical PresentationThe clinical manifestations of scombroid poisoning appear within minutes to hours of eating contaminated fish and are the result of histamine poisoning. Histamine is an endogenous amine with numerous biological effects,6 including vasodilation, an immediate allergic response following activation of H1 receptors, and neurotransmission due to the activation of H3 receptors. The amount of histamine required to produce manifestations varies from one person to the next. Scombroid poisoning symptoms tend to be mild and typically start with a burning or tingling sensation on the tongue, accompanied or not by a peppery and/or metallic taste. This is gradually followed by flushing in the head and neck area, with a considerable burning sensation, and a downward-spreading erythematous urticarial rash on the face and upper trunk7 (Fig. 1). Other common symptoms are a burning sensation, pruritus, and swelling around the mouth. Gastrointestinal symptoms are also common and include stomach cramps, nausea, vomiting, and diarrhea. A throbbing headache and palpitations are other hallmark symptoms. Because of the similarity with allergic reaction symptoms, scombroid poisoning is frequently mistaken for immunoglobulin E (IgE)–mediated fish allergy. Although rare, there have been reports of hypotension with distributive shock, bronchospasm, respiratory distress, and cardiac arrhythmias; these complications tend to occur in patients with an underlying condition (e.g., asthma or heart disease),8–10 explaining why some authors have described scombroid poisoning as a dermatologic emergency.11
Symptoms typically disappear within 12 to 48hours without treatment and leave no short-term or long-term sequelae. Patients under treatment with isoniazid or monoamine oxidase inhibitors (MAOIs) are more vulnerable to histamine fish poisoning4 and develop more severe and lasting symptoms, as these drugs inhibit the metabolism of histamine. Patients under treatment with antihistamines, by contrast, are somewhat protected against scombroid poisoning as these block the effect of histamine.
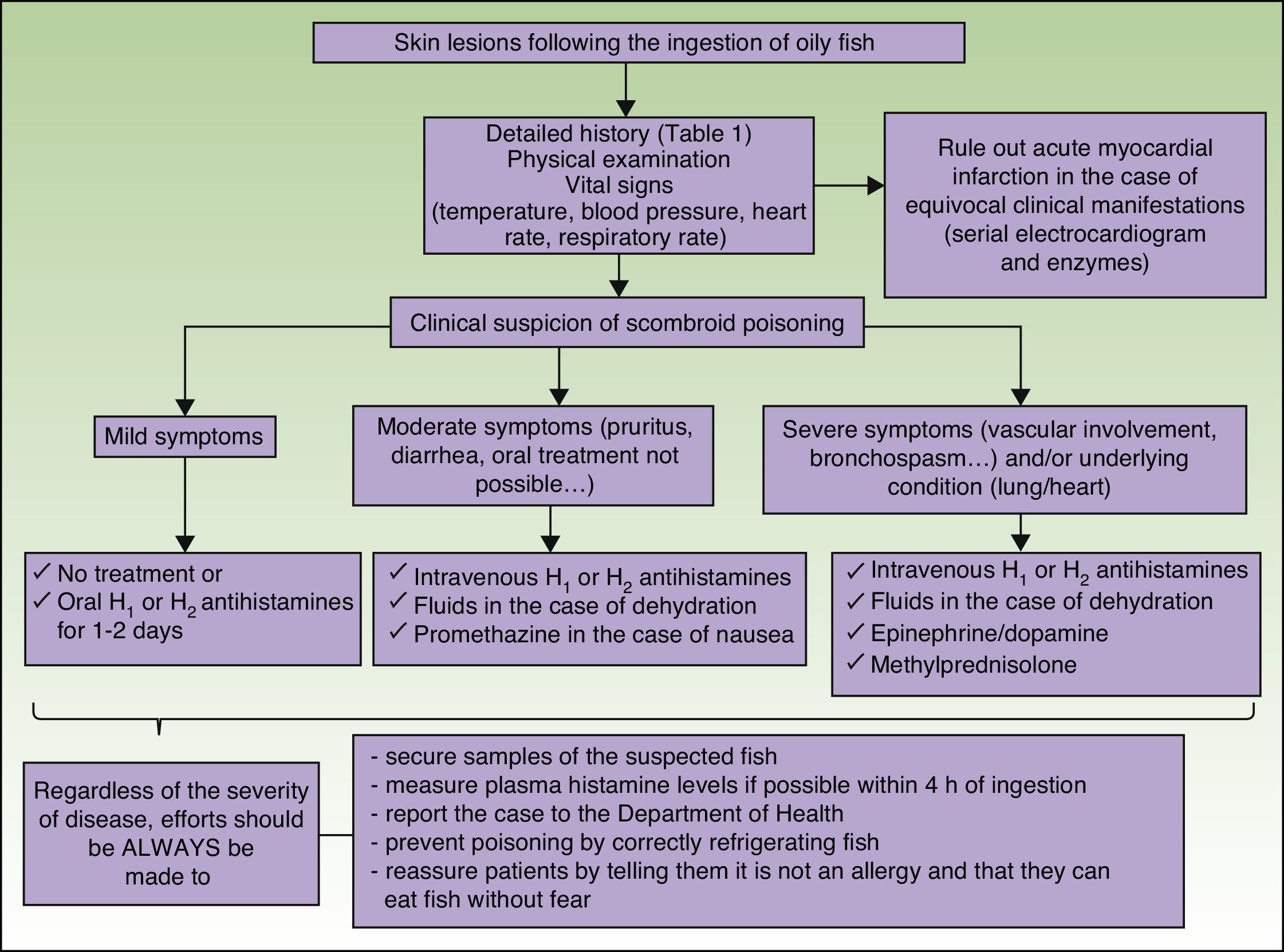
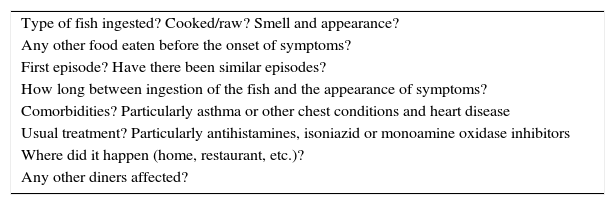
DiagnosisThere are no specific diagnostic tests for scombroid poisoning in humans. The condition is generally diagnosed on clinical grounds and a recent history of fish ingestion.12 A thorough history is thus very important for the correct diagnosis of scombroid poisoning (Table 1). The following findings can also help to raise suspicion:
- 1.
Onset of symptoms within 1 hour of eating scombroid fish
- 2.
Histamine-mediated symptoms, such as flushing, rash, headache, diarrhea, etc.
- 3.
Epidemiological data: similar symptoms in other diners
- 4.
Rapid resolution of symptoms following the administration of antihistamines
Questions to Ask When Faced With a Suspected Case of Scombroid Poisoning.
| Type of fish ingested? Cooked/raw? Smell and appearance? |
| Any other food eaten before the onset of symptoms? |
| First episode? Have there been similar episodes? |
| How long between ingestion of the fish and the appearance of symptoms? |
| Comorbidities? Particularly asthma or other chest conditions and heart disease |
| Usual treatment? Particularly antihistamines, isoniazid or monoamine oxidase inhibitors |
| Where did it happen (home, restaurant, etc.)? |
| Any other diners affected? |
Once scombroid poisoning is suspected, a definitive diagnosis can be established by measuring histamine levels in the fish implicated in the episode. Levels of over 50mg per 100g of fish are considered toxic.4 In Europe, histamine levels must not exceed 10mg per 100g. Levels are determined by sending samples of the suspect fish to the laboratory, accompanied, where appropriate, by other products from the same lot. It is important to ensure that the samples are shipped in a frozen state to prevent the formation of histamine during shipment. Furthermore, because histamine levels can vary enormously from one part of the fish to another, different sections should be sent.
It is also useful to measure plasma histamine levels in the patient13; a 2- to 4-fold increase above normal is suggestive of poisoning. This test must be performed within 24hours, as levels return to normal after this time. High plasma histamine levels within the first 4hours have been proposed as a specific finding for scombroid poisoning.
Differential DiagnosisThe following conditions should be contemplated in the differential diagnosis3:
Allergic reaction to fish. This is the most common condition with which scombroid poisoning is confused. De novo fish allergy is rare in adults, with a prevalence of just 0.6%.14 However, the absence of known allergies, similar symptoms in other diners, and, where possible, the detection of toxic histamine levels in fish, all help to establish a diagnosis of scombroid poisoning. If the suspicion of an allergic reaction persists, specific IgE levels should be measured or the patient referred to an allergologist.
Acute myocardial infarction. This condition is distinguishable from scombroid poisoning in that its main manifestation is intense, oppressive chest pain, accompanied by symptoms such as profuse sweating, dizziness, nausea, vomiting, etc. Serial electrocardiograms and normal cardiac markers help to rule out infarction.
Staphylococcal food poisoning. Unlike scombroid food poisoning, staphylococcal food poisoning is generally characterized by fever and does not cause flushing or rash.
Given the benign nature of scombroid poisoning and its tendency to spontaneously resolve, many patients do not require treatment. In the case of mild symptoms (flushing, burning, rash, or swelling around the mouth), the only effective treatment is the prompt administration of oral antihistamines for 1 to 2 days.4 H1 antihistamines, including cetirizine, are preferable as they are nonsedating. They can be combined with an H2 antihistamine, such as cimetidine, famotidine, or ranitidine.4 With this treatment, symptoms should resolve within 6 to 8hours. It is unnecessary to prolong treatment for longer than 2 days, as this is the time it takes for the toxin to be completely absorbed or eliminated and consequently for the clinical manifestations to disappear.
Intravenous antihistamines can be administered to patients with very bothersome symptoms or patients who do not tolerate oral antihistamines. The drugs of choice in such cases are diphenhydramine, famotidine, and ranitidine.4
Patients who experience hypertension or dehydration should be administered fluids, and vomiting can be treated with intravenous promethazine. The use of epinephrine or other vasoconstrictors should be considered in patients with severe symptoms, although these situations are extremely rare (Fig. 2).
Corticosteroids15 and epinephrine are not indicated in mild cases, as their action is independent of the pathogenesis of scombroid poisoning. In other words, they do not reduce histamine levels and as such are ineffective.
The prophylactic use of antihistamines is not justified either,4 although it could be indicated in a patient about to eat fish who is being treated with isoniazid and/or MAOIs and has had a prior episode of scombroid poisoning.
It is important to educate patients on the origin of the condition and remind them that it is not a fish allergy and they can therefore eat fish without fear of a reaction.16
PrognosisScombroid poisoning is generally a benign, self-limiting condition. However, because there have been reports of distributive shock, bronchospasm, and cardiac arrhythmias, early diagnosis and treatment is important. There has just been 1 reported death due to scombroid poisoning worldwide.17
PreventionThe most important consideration is that scombroid poisoning can be prevented by rapidly refrigerating fish for consumption. Fish should be ideally be stored at a temperature of 0°C or less to prevent both the growth of bacteria and the activation of histidine decarboxylase. It is important to recall that while cooking or freezing contaminated fish can destroy the bacteria, it will not destroy the toxin, which is stable in heat and cold.
Finally, outbreaks of scombroid poisoning should always be reported to the health department to prevent other cases.
ConclusionsScombroid poisoning is a common cause of fish poisoning and is very probably underdiagnosed. It typically presents with cutaneous lesions and is treated with oral antihistamines for 1 to 2 days. Complications are rare. Prevention is unquestionably the best “cure”, as once histamine has formed, reactions cannot be prevented by cooking, freezing, or canning. Familiarity with this condition among dermatologists will help to prevent confusion with allergic reactions to fish. As scombroid poisoning presents with skin lesions, it is likely that at some point in our career, we will be called on by the emergency department to evaluate a case of scombroid poisoning.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Guergué-Díaz de Cerio O, Barrutia-Borque A, Gardeazabal-García J. Escombroidosis: abordaje práctico. Actas Dermosifiliogr. 2016;107:567–571.