In 2008, Giuseppe Fabrizi et al.1 were the first to describe a subgroup of lesions with distinct histopathologic characteristics among all the melanocytic nevi excised for clinical regression; these lesions were given the name of sclerosing nevus with pseudomelanomatous features (SNPF).
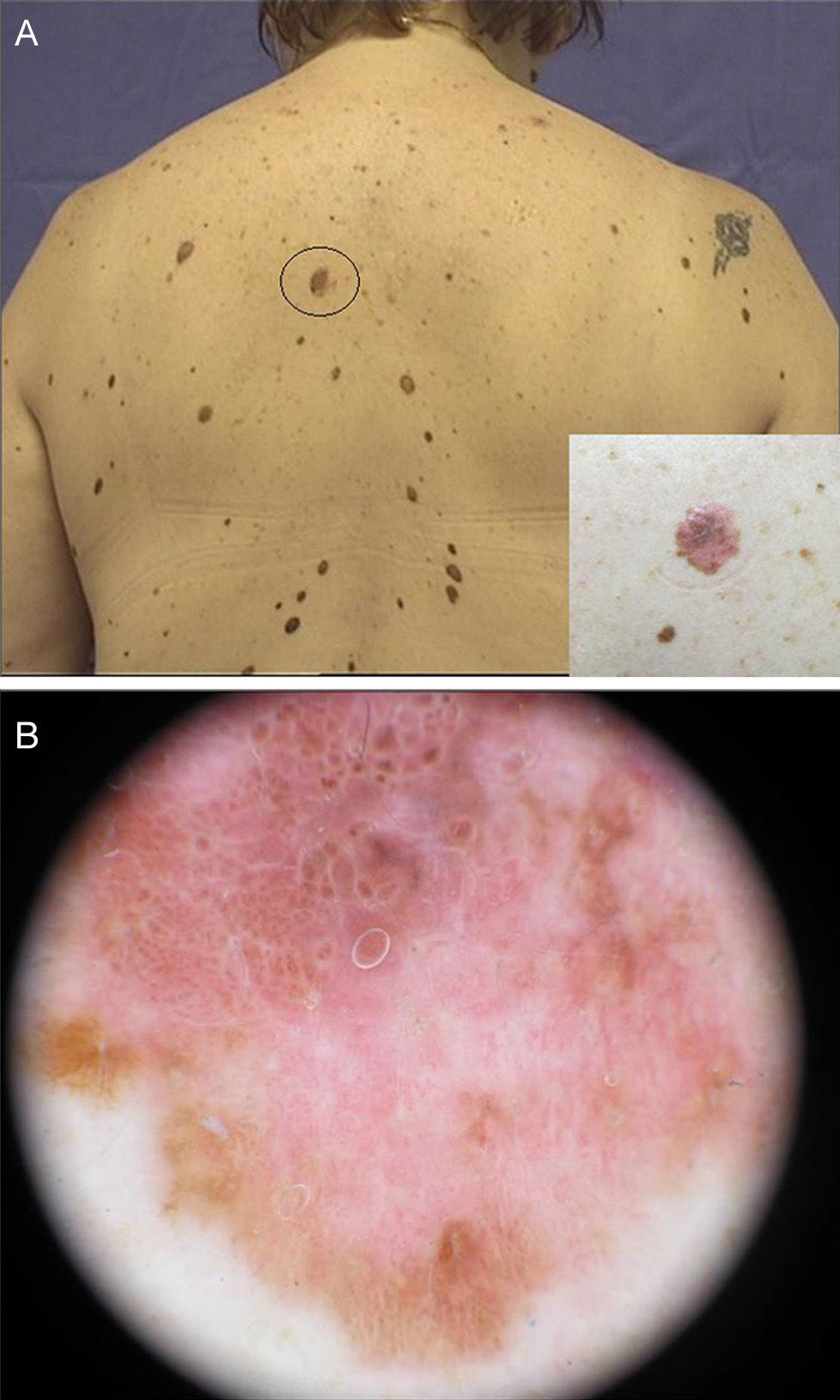
We present the case of a 44-year-old woman who was seen for persistent pruritus in the area of a nevus on her back. The variegate maculopapular lesion measured approximately 1cm in diameter and had irregular borders. On dermoscopy, an atypical globular pattern and a negative network were observed, with red, white, and occasional bluish areas (Fig. 1).
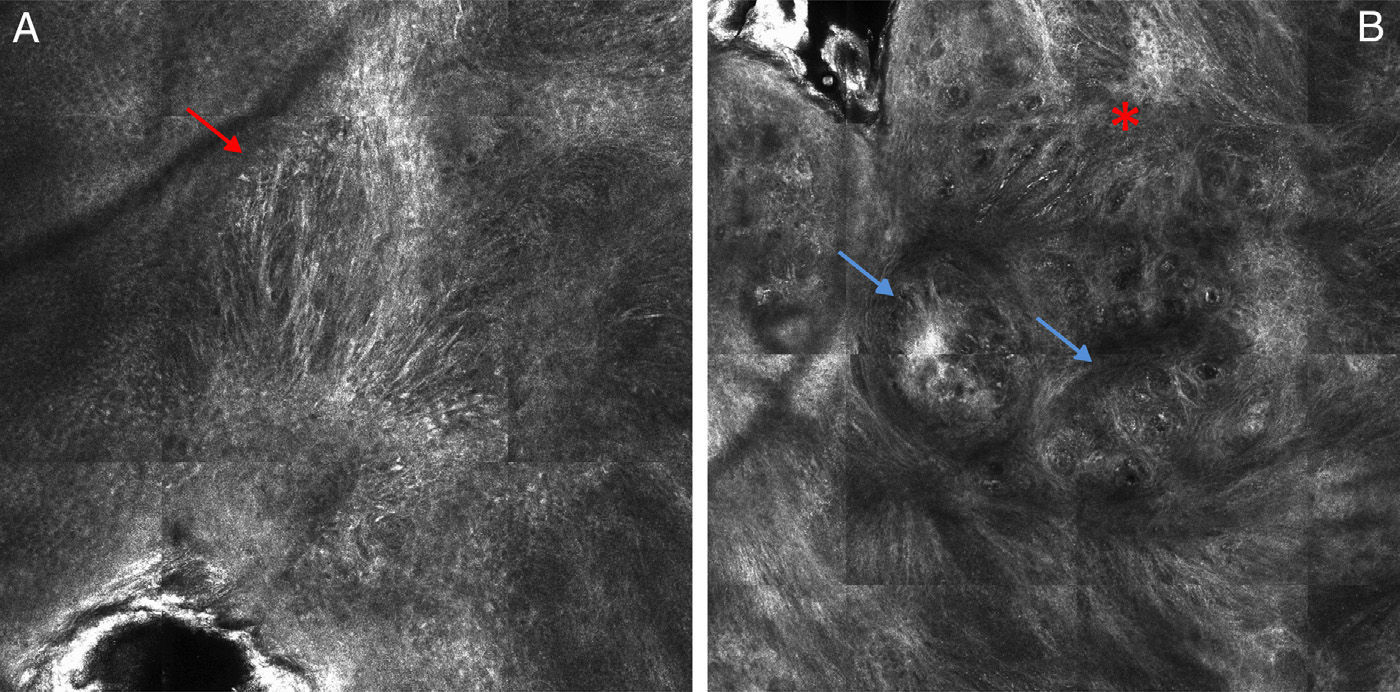
The lesion was evaluated using reflectance confocal microscopy (RCM), which showed marked destructuring of the epidermis, with irregularly shaped keratinocytes instead of the typical honeycomb or cobbled appearance, the presence of pagetoid cells with a multifocal distribution and dendritic morphology, a loss of bright rings, the absence of a defined pattern at the dermoepidermal junction, the presence of atypical cells forming junctional and dermal nests, and a dense inflammatory infiltrate with fibrosis and abundant melanophages (Fig. 2). With a suspected diagnosis of melanoma, the lesion was excised.
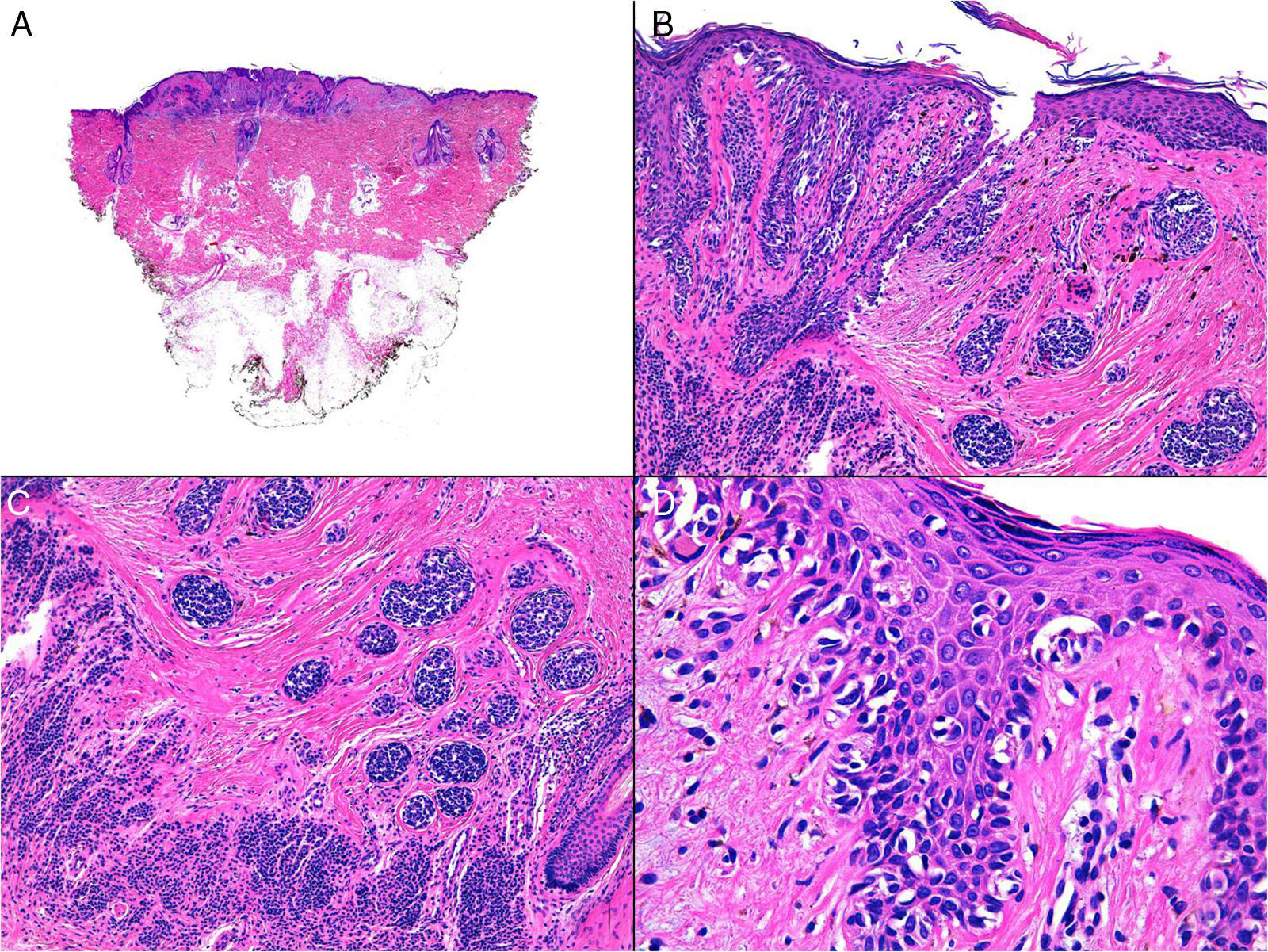
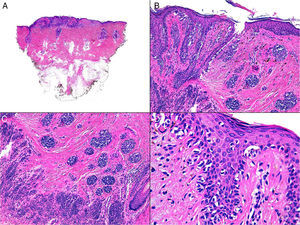
Histopathology revealed an atypical proliferation of melanocytes at the dermoepidermal junction, with occasional pagetoid spread in the epidermis, an area of scar tissue, melanocytic nests with a morphology similar to that described at the dermoepidermal junction, and a residual nevus with a congenital pattern, both peripherally and deep to the scar tissue. The cells were not frankly atypical and, after detailed examination, no mitotic figures were identified (Fig. 3). The proliferation index was very low and was limited practically to the junctional component. The cells of the irregular nests and of the residual nevus component expressed Melan-A and p16, with a loss of expression of HMB-45 in the dermal component. The lesion did not reach the borders of resection. This histologic image was consistent with a sclerosing nevus with pseudomelanomatous features. With this diagnosis, no additional treatment was performed, and the patient remains on follow-up.
Histology. A, Lesion with a 3-zone pattern. Hematoxylin and eosin (H&E), low-power view. B and C, Proliferation of atypical melanocytes at the dermoepidermal junction with an area of scarring, nests of atypical melanocytes, and a congenital-type residual nevus both peripheral and deep to the scar. H&E, original magnification×100. D, Scattered areas of pagetoid spread of melanocytic cells in other areas of the epidermis. H&E, original magnification×400.
SNPF, a recently described clinical and pathologic entity, is also known as nevus with florid fibroplasia.2 It is considered to mimic melanoma both clinically and histologically.3 Etiologically, this lesion appears to be a benign melanocytic nevus that becomes involved in a process of fibrosis combined with a pseudomelanomatous proliferation. It typically arises in young individuals, mainly on the back, particularly in the area of the scapula. This site is thought to be affected because of almost imperceptible microtrauma or inflammatory changes in the region, such as the chronic friction of clothing, sunburn, seborrheic eczema, or acne. However, other authors consider that this type of fibrosis may be something intrinsic to the maturation process of a dysplastic nevus.2
Dermoscopically it is characterized by signs of regression, affecting 10% to 50% of the lesion, in the form of white and blue scars, and an absence of other specific signs of melanoma.4
RCM is a noninvasive technique with a resolution very similar to conventional histology. It provides horizontal images and can be considered an intermediate diagnostic method between dermoscopy and histopathology, frequently avoiding unnecessary surgical excisions. However, the presence of cellular atypia on RCM study in these cases means that a diagnosis of melanoma cannot be ruled out. As is to be expected, abundant melanophages and collagen bundles are also observed.5
Histologically there are 3 zones: an atypical proliferation of melanocytes at the dermoepidermal junction, with lentiginous hyperplasia, and confluent junctional nests with occasional pagetoid spread; a significant area of dermal sclerosis that contains irregular nests of atypical melanocytes; and a congenital-type residual nevus adjacent to the deep surface of the scar.1 The low level of cellular atypia and the absence of mitoses, cell necrosis, or spreading dermal nodules differentiates this lesion from regressing melanoma. In addition, SNPF usually has an “ordered” pattern of fibrosis, with homogeneous bundles of parallel eosinophilic collagen fibers closely related to the epidermis. In contrast, a regressing melanoma is characterized by fibrosis that is often paler (perhaps because of edema), formed of more irregular collagen bundles, and the presence of melanophages. The diagnostic criteria of Fabrizi et al. probably make it possible to differentiate SNPF from a regressing melanoma. However, atypia in the junctional region associated with pagetoid spread makes diagnosis of this entity a question of the quantitative presence of morphological criteria, and a degree of interobserver variability between pathologists should therefore be expected.3
Taking into account the benign biological behavior of this entity, some authors consider that a more conservative approach could be warranted in melanocytic lesions showing regression on the convex area of the back.4 Those authors propose observation. However, other authors recommend surgical excision, as SNPF mimics melanoma clinically, dermoscopically, and on RCM.5 Only histology can give us the definitive diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Floristán Muruzábal U, Pinedo Moraleda FJ, Gamo Villegas R, López Estebaranz JL. Nevus esclerosante con rasgos seudomelanomatosos. Actas Dermosifiliogr. 2016;107:691–694.