Necrobiosis lipoidica is a granulomatous disease of unknown origin that typically gives rise to multiple lesions on the anterior aspect of both lower legs. The histopathologic abnormalities are mainly observed in the mid and deep dermis. The alterations tend to extend into the subcutaneous cellular tissue along the adipose tissue septa, giving rise to a predominantly septal panniculitis.1,2
High-frequency skin ultrasound has been shown to be a useful additional test for the diagnosis and differentiation of inflammatory diseases that affect the dermis and subcutaneous cellular tissue.3
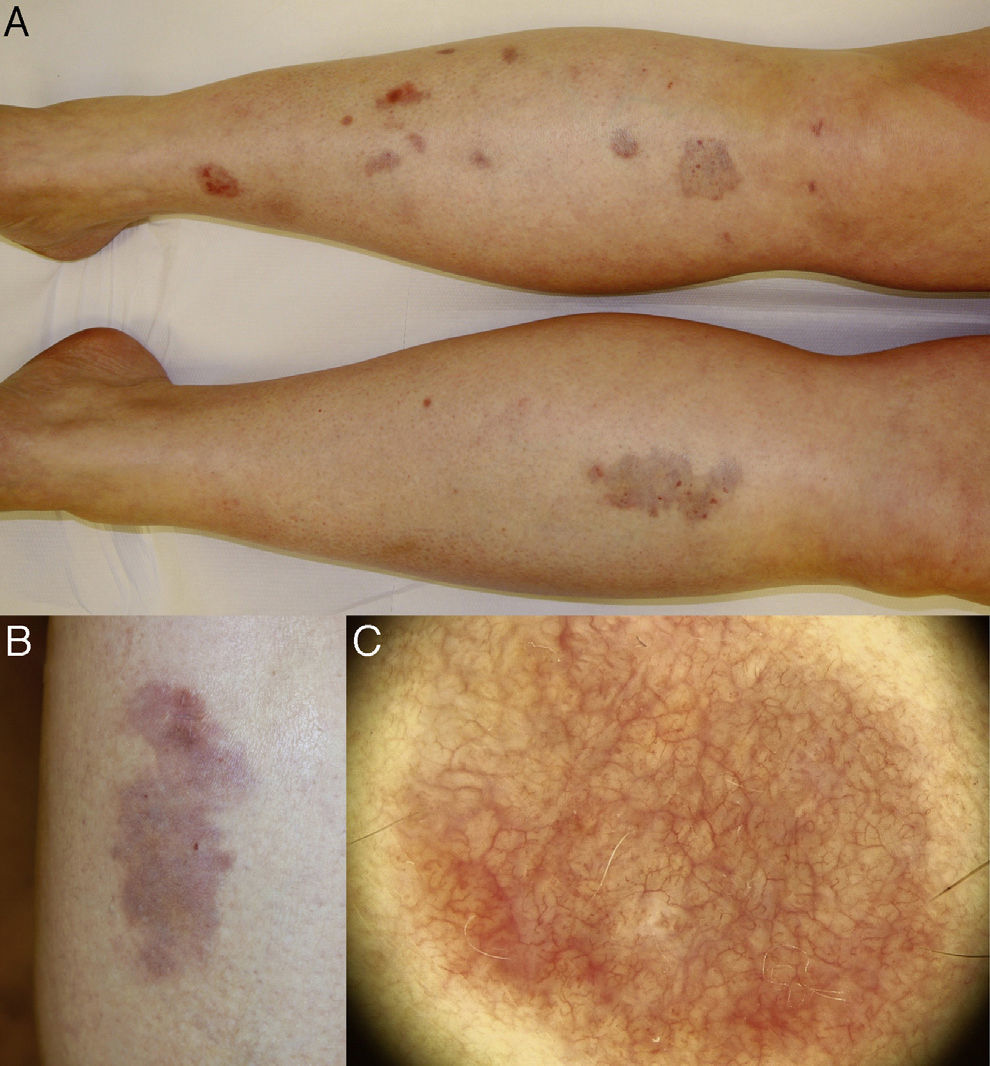
Case DescriptionOur patient was a 40-year-old woman with a history of systemic lupus erythematosus, with lupus nephritis diagnosed in 1997 (currently asymptomatic and not on treatment) and nonspecific colitis diagnosed in 2010 (on treatment with sulfasalazine). She was seen for asymptomatic lesions on the lower legs. The alterations had started 2 years earlier as a single lesion on the anterior aspect of left lower leg and had later affected the right lower limb. Dermoscopic study of 1 of the lesions (FotoFinder Medicam 800HD, FotoFinder Systems GmbH, Bad Birnbach, Germany) revealed a dense network of branching anastomosing vessels on a yellow-orange background (Fig. 1).
A, Well-defined, round and oval plaques affecting the anterior aspect of both lower legs. B, Detail of an isolated erythematous lesion, with orange, yellowish, brownish, and whitish areas; superficial atrophy and numerous telangiectasias can be observed. C, Dermoscopic image showing a dense network of branching anastomosing vessels on a yellow-orange background with whitish areas.
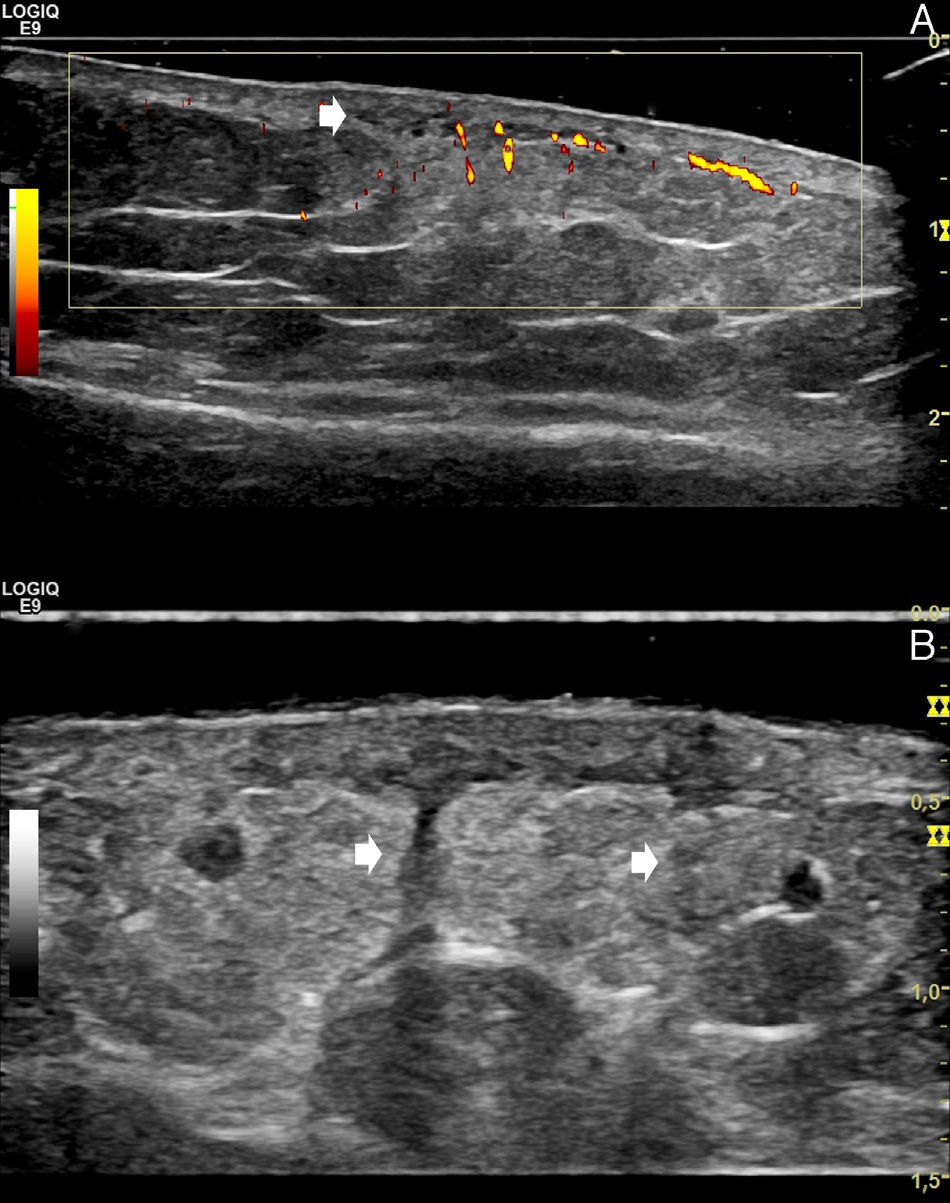
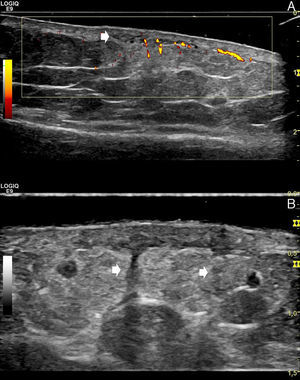
Ultrasound was performed using the LOGIQ E9 XDclear device (General Electric Health Systems, Milwaukee, United States) with 2 linear transducers with maximum frequencies of 15 and 18MHz. Hypoechoic areas were observed in the mid and deep dermis, with evidence of increased blood flow on color power Doppler. Compared with healthy perilesional skin, the dermohypodermal interface was blurred as a result of a diffuse increase in echogenicity of the subcutaneous cellular tissue (Fig. 2A). At greater depth, vertical hypoechoic bands were seen to penetrate deeply into the fat (Fig. 2B).
A, Power Doppler ultrasound (linear 15MHz transducer; longitudinal axis, left leg): hypoechoic areas in the mid and deep dermis (arrow), with blurring of the dermohypodermal junction and a diffusely increased echogenicity of the underlying superficial hypodermal adipose tissue. Power Doppler shows increased dermal and superficial hypodermal flow. The image allows us to compare the affected area (right side of the image) with healthy perilesional skin (left side of the image). B, Gray-scale ultrasound (linear 18MHz transducer; longitudinal axis, left leg). The hypoechoic vertical bands correspond to thickened septa (arrows).
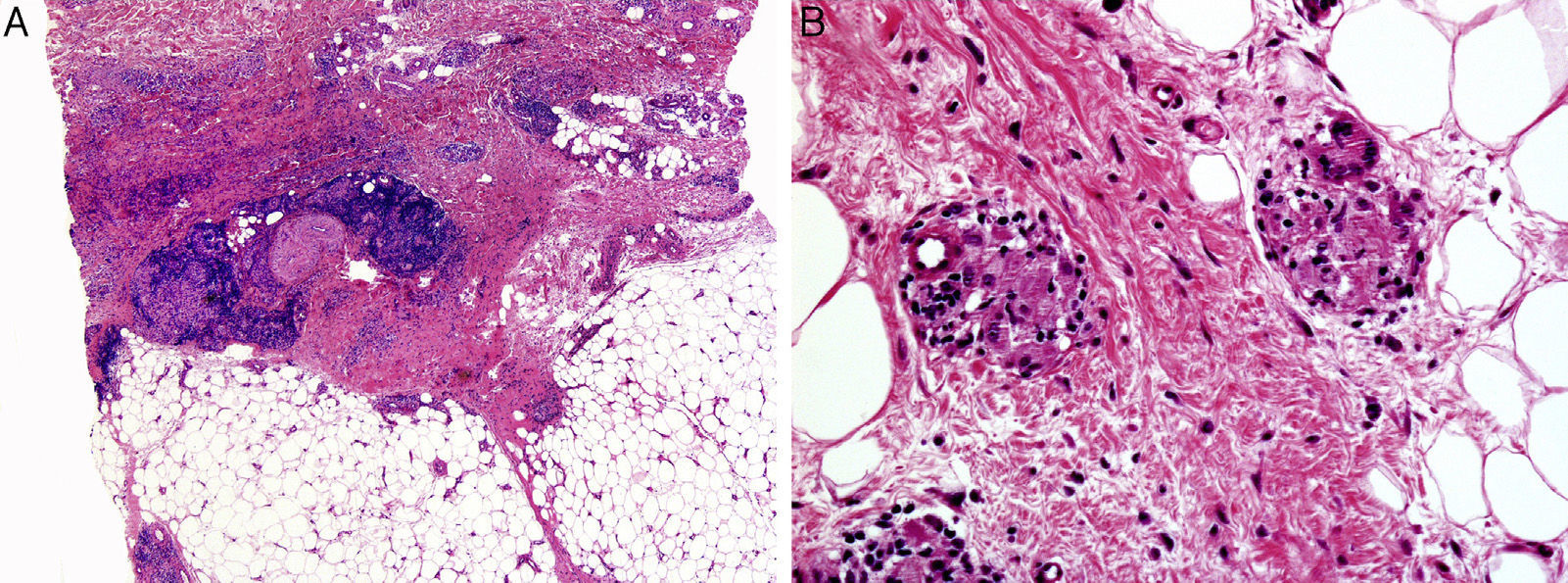
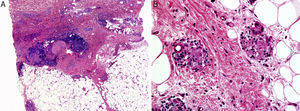
Histopathology revealed areas of degenerated collagen surrounded by palisaded histiocytes and a lymphocytic and plasma-cell infiltrate that mainly affected the mid and deep dermis (Fig. 3A). The inflammatory changes extended into the subcutaneous cellular tissue, with foci of degenerated collagen surrounded by histiocytes in the connective tissue septa of the hypodermis, forming granulomas of vaguely sarcoid appearance (Fig. 3B).
A, Predominant involvement of the mid and deep dermis, with areas of degenerated collagen surrounded by palisaded histiocytes and a lymphocytic and plasma-cell infiltrate. B, The inflammatory changes extend into the subcutaneous cellular tissue, with foci of degenerated collagen surrounded by histiocytes in the connective tissue septa, forming granulomas of vaguely sarcoid appearance.
A diagnosis of sarcoidal necrobiosis lipoidica was made and blood tests were requested, including measurement of blood glucose, thyroid hormones, and antithyroid antibodies, which were normal or negative. Treatment was started with topical corticosteroids.
DiscussionThis case illustrates the usefulness of high-frequency ultrasound to guide the diagnosis in suspected necrobiosis lipoidica. The technique enables us to locate foci of inflammation in the mid and deep dermis, and to demonstrate the presence of panniculitis with edema and thickening of the septa in the subcutaneous cellular tissue. Dermal inflammation is seen as hypoechoic areas that usually have increased blood flow on color Doppler or power Doppler (slow flow). The inflammatory findings in the subcutaneous cellular tissue vary depending on whether involvement is predominantly lobular, septal, or mixed. Lobular involvement produces a diffuse increase in echogenicity of the adipose tissue; septal involvement produces a typically hypoechoic noncompressible thickening of the septa, seen as hypoechoic perilobular bands. In mixed panniculitis, the 2 patterns coexist.3 In our patient, we also observed the characteristic loss of sharpness of the dermohypodermal junction, which we believe to be due to the simultaneous inflammatory involvement of the deep reticular dermis and the hypodermis.
Dermoscopy in our patient was characteristic. The lesions presented hairpin vessels on a yellowish-orange background with whitish areas. Branching vascular structures are formed of anastomosing vessels of a similar size. The presence of comma vessels has also been described as an early manifestation of the disease.4 A pigmented pseudonetwork and a brown-colored background due to melanocyte stimulation are sometimes observed.5
The case presented occurred in a nondiabetic patient with a diagnosis of systemic lupus erythematosus and nonspecific colitis. The association of necrobiosis lipoidica and diabetes mellitus is well known, but the proportion of patients who present both diseases varies between the different studies (11% to 65%).6–8 Necrobiosis lipoidica has also been reported in healthy individuals and in patients with other autoimmune and inflammatory diseases, including inflammatory bowel disease.8
Finally, the finding on histopathology of sarcoid granulomas in the dermis and in the adipose tissue septa was interesting. These structures, formed of groups of giant and epithelioid cells in areas of degenerated collagen, are an uncommon feature that defines what has been called the sarcoid variant of necrobiosis lipoidica.9,10
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Gavín J, Comba Pérez-Pérez L, Requena L, Wortsman X. Necrobiosis lipoídica sarcoidea en paciente no diabético. Utilidad de la ecografía cutánea. Actas Dermosifiliogr. 2016;107:525–527.