The concept of dysplastic nevus (DN) is somewhat controversial. While DN is not a proven precursor of cutaneous melanoma, several studies suggest that it may be a risk factor. The management of DN is also a topic of some debate. There is no consensus on the optimal approach (observation or re-excision) when a nevus with moderate dysplasia has been excised and the margins are affected. A survey conducted in North America found that 48% of those surveyed would re-excise the lesion. In 2015, the North American Pigmented Lesion Subcommittee suggested that observation may be a reasonable option, although the evidence to support this recommendation was limited.1
Recently, Kim et al2 published the results of a retrospective multicenter study that examined the development of melanoma in 438 patients with excised nevi with moderate dysplasia and compromised margins (467 lesions). Of these, 50.4% had undergone previous biopsies of dysplastic nevi, 33.2% had a history of melanoma, and 23.8% (83 of 349 patients) had a family history of melanoma. The biopsy methods used were shave (46.4%), punch (45.3%), and elliptical (7.7%) excision. Dysplasia was independently assessed by an expert. During a mean follow-up period of 6.9 years (range, 3–21.3 y), none of the participants developed melanoma at the site of the excised DN. However, 22.8% developed a primary melanoma at a different site. Of these, 3 patients had metastatic melanoma (2 with invasive melanoma prior to biopsy). Comparison of those that developed a subsequent cutaneous melanoma with those that did not identified the following risk factors: older age (mean age of 49.7 vs 45.9 years; P = 0.04); history of previous melanoma (49% vs 9.9%; P < 0.001); and a previously biopsied DN (33.5% vs 13.2%; P < 0.001). No association was observed for sex or family history of melanoma. Multivariate regression analysis revealed that a history of melanoma (odds ratio [OR], 11.74; 95%CI, 5.71–24.15; P < 0.001) and previous (histologically confirmed) DN (OR, 2.55; 95%CI, 1.23–5.28; P = 0.01) were independently associated with the development of melanoma at a site other than that of the DN biopsy, even after adjusting for age, sex, and family history of melanoma.
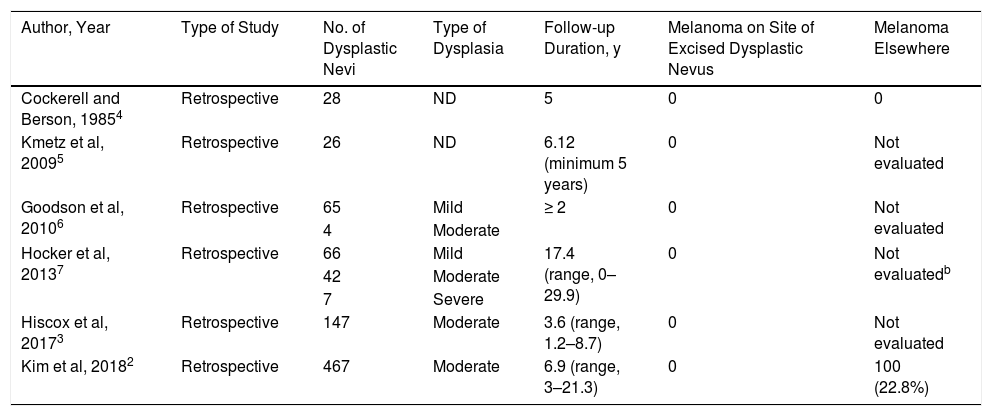
The results of the study by Kim et al, the largest cohort described to date, are consistent with the findings of previous publications (Table 1),3 suggesting that observation is a reasonable option in these cases and supporting the hypothesis that DN is not a precursor lesion of melanoma, but an important risk marker. It should be noted that around 70% of cutaneous melanomas develop de novo and not on a pre-existing nevus.
Summary of Studies on the Follow-up of Excised Dysplastic Nevi with Affected Margins
| Author, Year | Type of Study | No. of Dysplastic Nevi | Type of Dysplasia | Follow-up Duration, y | Melanoma on Site of Excised Dysplastic Nevus | Melanoma Elsewhere |
|---|---|---|---|---|---|---|
| Cockerell and Berson, 19854 | Retrospective | 28 | ND | 5 | 0 | 0 |
| Kmetz et al, 20095 | Retrospective | 26 | ND | 6.12 (minimum 5 years) | 0 | Not evaluated |
| Goodson et al, 20106 | Retrospective | 65 | Mild | ≥ 2 | 0 | Not evaluated |
| 4 | Moderate | |||||
| Hocker et al, 20137 | Retrospective | 66 | Mild | 17.4 (range, 0–29.9) | 0 | Not evaluatedb |
| 42 | Moderate | |||||
| 7 | Severe | |||||
| Hiscox et al, 20173 | Retrospective | 147 | Moderate | 3.6 (range, 1.2–8.7) | 0 | Not evaluated |
| Kim et al, 20182 | Retrospective | 467 | Moderate | 6.9 (range, 3–21.3) | 0 | 100 (22.8%) |
Abbreviation: ND, not described.
aStudies based exclusively on the follow-up of nevi with severe dysplasia are not included in this table.
In patients with nevi with moderate dysplasia and affected margins after excision, clinical observation may be a valid option. Patients with a previous history of melanoma or 2 DNs (one of which shows moderate dysplasia) should be considered at high risk and followed closely.
Please cite this article as: Morgado-Carrasco D, Feola H, Fustà-Novell X, Martinez N. FR-Nevus con displasia moderada extirpados con márgenes quirúrgicos afectados. ¿Se deben reextirpar? Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2019.01.028