Reticulate acropigmentation of Kitamura (RAPK) is an uncommon genodermatosis that is classed as a congenital reticulate pigmentary disorder. It is characterized by acral lentiginous pigmentation and mainly affects Japanese individuals. Nevus of Ito is a congenital dermal melanocytosis that is congenital and affects the deltoid and acromioclavicular region, more commonly in Asian women.
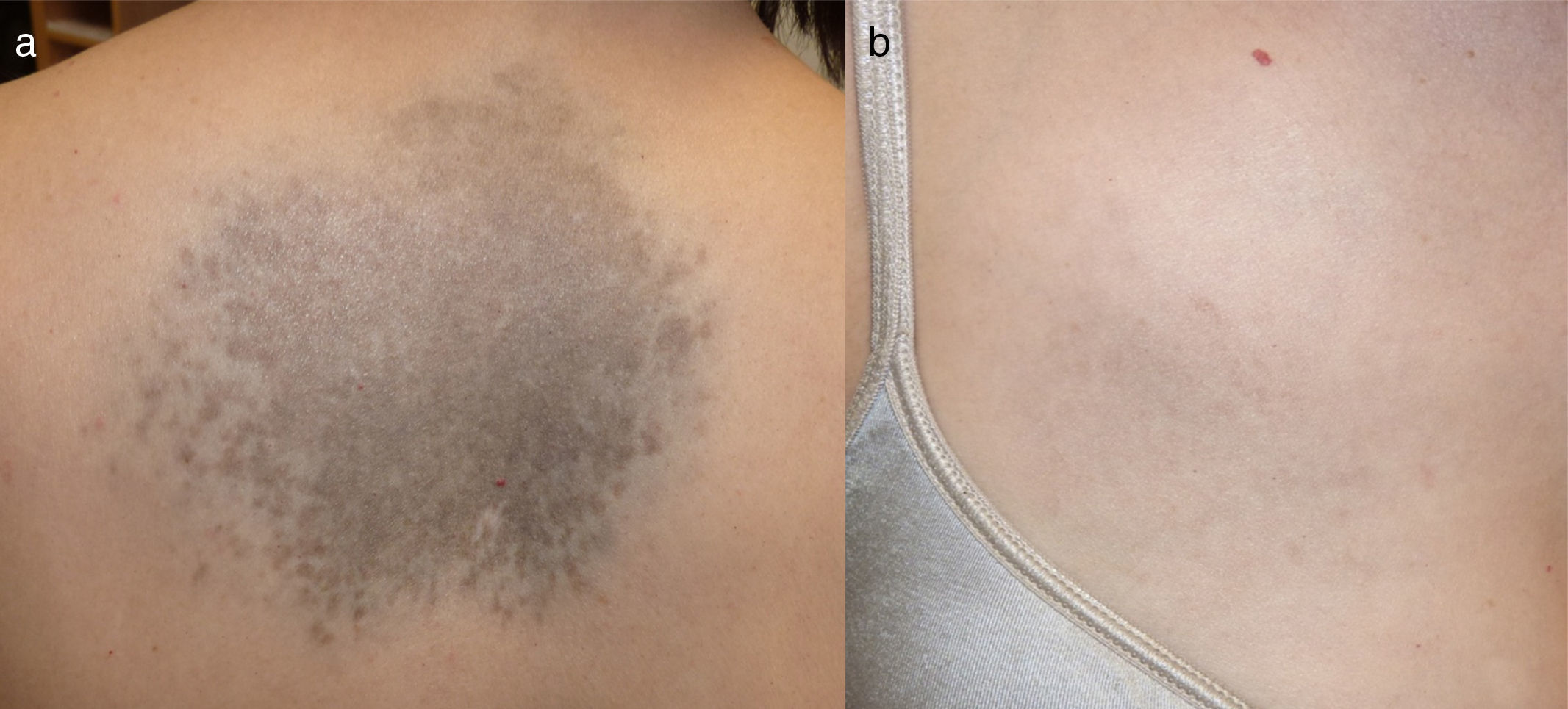
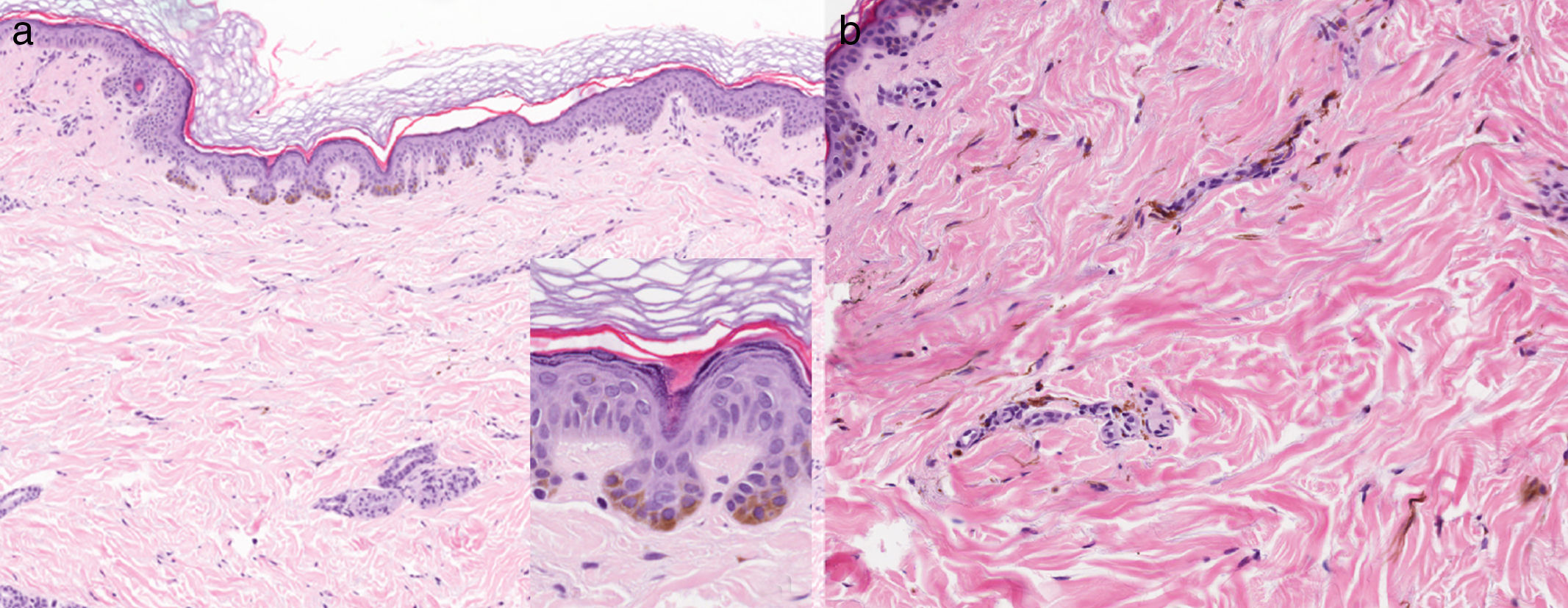
We report the case of a 47-year-old woman (phototype III) with no clinical history of interest who consulted for progressively slow-growing asymptomatic darkening of the skin on the dorsum of the hands and on the face that began during adolescence. She reported that her mother had similar pigmentation on the hands, although other family members did not (2 maternal aunts, 2 siblings, 3 children). She also had a stable congenital lesion on her back and right hemithorax. Examination revealed symmetrical lentiginous pigmentation on the dorsum of the hands, the anterior aspect of the wrists, the eyelids, and the area around the lips, together with palmoplantar pits and interrupted palmar creases (Fig. 1). A blue-grayish plaque was observed on her back and right hemithorax and arm (Fig. 2). Analysis of a biopsy specimen from the hand revealed lentiginous epidermal hyperplasia with hyperpigmented bulbous projections of the epidermal rete ridges; in the case of the dorsum, it revealed dendritic melanocytes in the dermis (Fig. 3). These findings led us to diagnose the patient's condition as RAPK and nevus of Ito.
A, Findings from a biopsy specimen taken from the wrist. Note the lentiginous epidermal hyperplasia with hyperpigmented bulbous projections of the epidermal rete ridges and increased basal melanocytes (hematoxylin-eosin [H-E], original magnification ×10; detail (inset), original magnification ×40). B, Findings from a biopsy specimen taken from the back. Notice the dendritic melanocytes in the reticular and papillary dermis and hyperpigmentation of the basal layer of the epidermis (H-E, original magnification ×20).
Reticulate pigmentary disorders comprise a group of congenital and acquired conditions with reticulate or freckle-type hyperpigmentation and occasional hypopigmentation. There is some confusion in the literature with respect to definitions and terminology. Hereditary forms are unusual and have variable inheritance patterns, although they are generally autosomal dominant, with possible associated abnormalities. They include dyskeratosis congenita, Dowling-Degos disease, RAPK, Haber syndrome, reticulate acropigmentation of Dohi, Naegeli-Franceschetti-Jadassohn syndrome, X-linked reticulate pigmentary disorder, and dyschromatosis universalis hereditaria. In the acquired forms, the lesions are usually larger and include confluent and reticulate papillomatosis (Gougerot-Carteaud), prurigo pigmentosa, lichen planus pigmentosus, Riehl melanosis, erythema ab igne, cutis marmorata, livedo reticularis, and postinflammatory pigmentation.1
RAPK is an uncommon disorder, with approximately 130 reported cases.2–7 While more common in Japan, it can be found throughout the world. The inheritance pattern is autosomal dominant, although nonhereditary cases occur sporadically. It first appears during the first or second decade of life, with reticulate or freckle-like hyperpigmented macules that measure 1 to 5mm. The lesions are initially atrophic and are found on the dorsum of the hands and feet and can extend proximally with progressive darkening aggravated by exposure to sunlight. They rarely affect the face and are accompanied by palmoplantar pits and interrupted palmar creases, and there have been isolated reports of localized alopecia and absence of the distal phalanges of the toes. Dermoscopy shows the pigmentation to have a fine network of nonspecific reticulate brown pigment and the palmoplantar pits to have brown spots.2 Histopathology reveals atrophy of the epidermis, elongation, and increased melanin on the interpapillary ridges, with scarce perivascular lymphocytic infiltrate, and an increased number of DOPA-positive basal melanocytes.4
There is some debate over whether RAPK, Dowling-Degos disease, Haber syndrome, and reticulate acropigmentation of Dohi are variants of the same disease, since their clinical and histologic characteristics overlap to some extent, mainly in Dowling-Degos disease and RAPK. The exception is Galli-Galli disease, in which suprabasal acantholysis can be observed.3,4 Dowling-Degos disease is autosomal dominant, more commonly affects adult women, and manifests with reticulate pigmentation and brown hyperkeratotic papules mainly on flexures and the trunk. It may be accompanied by comedones on the face and neck, perioral pitting, and facial scars, and even epidermal cysts, suppurative hidradenitis, seborrheic keratosis, pilonidal cysts, and tumors such as keratoacanthoma and squamous cell carcinoma. Histologically, it is similar to RAPK, although with more pronounced follicular involvement. Recent genetic studies indicate that they are different disorders, although this issue remains unresolved. In Dowling-Degos disease, there have been reports of mutations in the keratin 5 gene (KRT5) and, subsequently, in the protein O-fucosyltransferase 1 gene (POFUT1) and protein O-glucosyltransferase 1 protein gene (POGLUT1), which overlaps clinically with RAPK.8 In 2013, several mutations were detected in the ADAM10 gene in Japanese families with RAPK,5 and, more recently, in other cases.6,7ADAM10 codes for a disintegrin and metalloprotease, a member of the a disintegrin and metalloprotease family, which has numerous biologic functions and is expressed in the human epidermis, melanoma cells, and keratinocytes. In mice, its mutation is associated with freckle-like pigmentation.5
Furthermore, dermal melanocytosis comprises a group of benign congenital and—less frequently—acquired disorders characterized by the presence of dendritic melanocytes in the dermis. They are more common in Asian and African women and are unusual in white individuals. They comprise nevus of Ota, nevus of Ito, Mongolian spots, and dermal melanocytic hamartoma. Dermal melanocytosis rarely becomes malignant, with barely 4 cases of nevus of Ito.9 Moreover, a case of Dowling-Degos disease and metastatic amelanotic melanoma has been reported.10 To date, RAPK has not been reported to occur alongside other melanocytic disorders. There is no proof that RAPK and nevus of Ito are related, since, although both are pigmentation disorders, they are different. Thus, in dermal melanocytosis there is a proliferation of dermal melanocytes, whereas in RAPK, electron microscopy reveals an increase in the number of melanosomes in lesional melanocytes and keratinocytes.6 The ADAM10 mutation has not been studied to date in dermal melanocytosis.
We present a case of RAPK and nevus of Ito in a white woman. This association has not previously been reported. Both conditions are more common in Asian individuals.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to Dr. Juan Luis Santiago Sánchez-Mateos for his help in this study.
Please cite this article as: García-Arpa M. Acropigmentación reticulada de Kitamura y nevus de Ito. Actas Dermosifiliogr. 2017;108:675–677.




![A, Findings from a biopsy specimen taken from the wrist. Note the lentiginous epidermal hyperplasia with hyperpigmented bulbous projections of the epidermal rete ridges and increased basal melanocytes (hematoxylin-eosin [H-E], original magnification ×10; detail (inset), original magnification ×40). B, Findings from a biopsy specimen taken from the back. Notice the dendritic melanocytes in the reticular and papillary dermis and hyperpigmentation of the basal layer of the epidermis (H-E, original magnification ×20). A, Findings from a biopsy specimen taken from the wrist. Note the lentiginous epidermal hyperplasia with hyperpigmented bulbous projections of the epidermal rete ridges and increased basal melanocytes (hematoxylin-eosin [H-E], original magnification ×10; detail (inset), original magnification ×40). B, Findings from a biopsy specimen taken from the back. Notice the dendritic melanocytes in the reticular and papillary dermis and hyperpigmentation of the basal layer of the epidermis (H-E, original magnification ×20).](https://static.elsevier.es/multimedia/15782190/0000010800000007/v2_201708291348/S1578219017302159/v2_201708291348/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



