A healthy 27-year-old heterosexual man visited the emergency department with diffuse edema in the buttocks, fever, and poor overall condition, which had appeared a week earlier. The patient had also presented in the previous year with cellulitis in the same location on up to 12 occasions and had received antibiotic treatment on multiple occasions for this reason. The patient stated that he had no past history of trauma and had not undergone topical or intramuscular treatment in that region.
Examination revealed tense, erythematous plaques (between 5 and 10cm in diameter) that were hot to the touch, and nodules in the gluteal and sacral region, showing marked asymmetry between the 2 buttocks (Fig. 1). Palpation also revealed swollen lymph glands measuring approximately between 1 and 2.5cm. Blood tests revealed leukocytosis with neutrophilia and raised C-reactive protein (CRP) levels (13.65mg/dL). Despite attempts to puncture the nodules, it was not possible to obtain material for study. The patient was admitted to the infectious disease unit and empirical intravenous antibiotic treatment was instated with ceftriaxone and clindamycin.
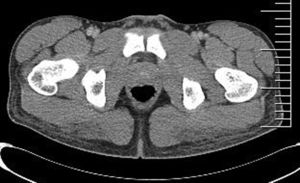
A pelvic CT scan revealed diffuse bilateral thickening in the superficial and deep soft tissue, which corresponded to radiologic signs of cellulitis and fasciitis. Both gluteus maximus muscles showed hypodense areas measuring approximately 6×2×5cm, and signs of myositis (Fig. 2). Two skin biopsies were performed, 1 of which was sent for histopathology study (Fig. 3) and the other for microbiology culture.
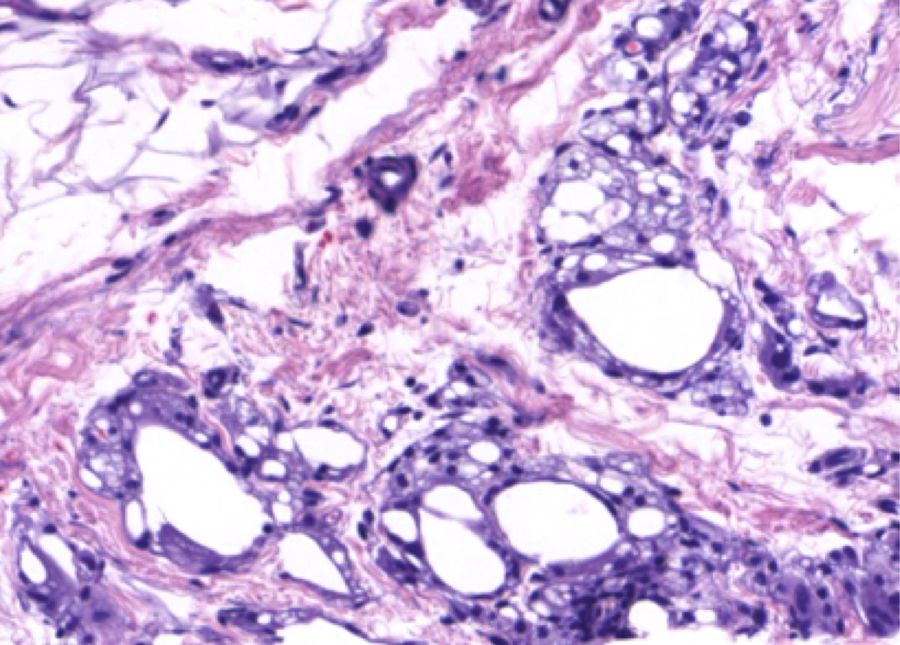
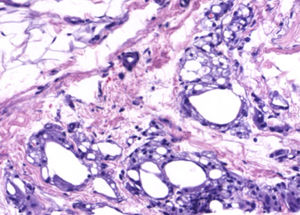
What is your diagnosis?Diagnosis and DiscussionThe microbiology culture was negative. Histology revealed multiple empty cystic areas in the dermis and hypodermis, surrounded by an inflammatory histiocyte infiltrate. The study also revealed abundant foam cells and multinucleate giant cells (Fig. 3).
When questioned again, the patient admitted that he had undergone injections with mineral oil 2 years earlier in the buttocks on up to 30 occasions, for esthetic purposes. A year later, he began to present the symptoms described above. In light of this information, foreign body granuloma was diagnosed and treatment with 40mg per day of prednisone was prescribed; a complete clinical response was achieved. The patient was then discharged with a descending dose of prednisone over 2 weeks. Because he continued to present intermittent episodes, minocycline was prescribed at a dosage of 100mg per day, with no clinical improvement. Alopurinol was later prescribed but was poorly tolerated by the patient and it was therefore decided to change to 400mg per day of hydroxychloroquine; however, the episodes persisted. The patient has since been undergoing intermittent pulse corticosteroid therapy with prednisone and has remained asymptomatic.
The popularity of injectable fillers has increased markedly in recent decades. The materials used include a wide variety of nonauthorized products.1,2 Mineral oil (petrolatum) has been used for cosmetic purposes to perform injections of permanent dermal filler. This filler has even been used to increase muscle volume3 and penis size.2,4 The cosmetic results immediately after injections of petrolatum tend to be satisfactory; however, the long-term complications are disastrous. For this reason, petrolatum is not currently considered legal for use as a filler. Furthermore, it is not generally administered by medical personnel and is most frequently self-injected.3,4
The adverse effects of injections of fillers include arterial occlusion, tissue necrosis, embolism, infections, hypersensitivity reactions, migration of the injected material, and even death.5 The formation of sclerosing lipogranuloma or paraffinoma, a granulomatous reaction associated with intense fibrosis, is a frequent complication secondary to injection of mineral oil.2,4 Histology often shows a “Swiss cheese” image, owing to cystic spaces that replace the normal subcutaneous cell tissue.5
Complications following the injection of liquid chemical products will present in a period of time that may vary from months to years.1 Adverse effects, such as infection and ulceration, are often seen within 18.5 months after the paraffin injections.6 With regard to treatment, complete surgical excision is the best option for preventing recurrence3; however, complete excision is often not possible. Macrolides and tetracyclines have been shown to produce good results where infection is suspected, partly owing to their anti-inflammatory action.5 Oral or intralesional corticosteroids can be used to reduce granulomatous immune reactions.1,5 Other therapeutic alternatives include tacrolimus, etanercept, and alopurinol.1
Although most medical professionals no longer inject unauthorized products, unqualified personnel continue to expose themselves and third parties to severe complications. It is therefore very important to take this entity into consideration as a possible diagnosis, as most patients will be reluctant to admit to having undergone these procedures. It should also be remembered that the adverse effects caused by injecting this material may appear after a long period of latency.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morgado-Carrasco D, Giavedoni P, Mascaró JM. Celulitis glútea de repetición en un varón joven. Actas Dermosifiliogr. 2020;111:63–64.