A 71-year-old man presented with a lesion on the first toe of the right foot that had appeared 4 months earlier.
Physical ExaminationPhysical examination revealed a firm tumor (largest diameter approximately 2cm) that was located on the lateral and plantar aspects of the first toe of the right foot and caused no discoloration of the overlying skin (Fig. 1).
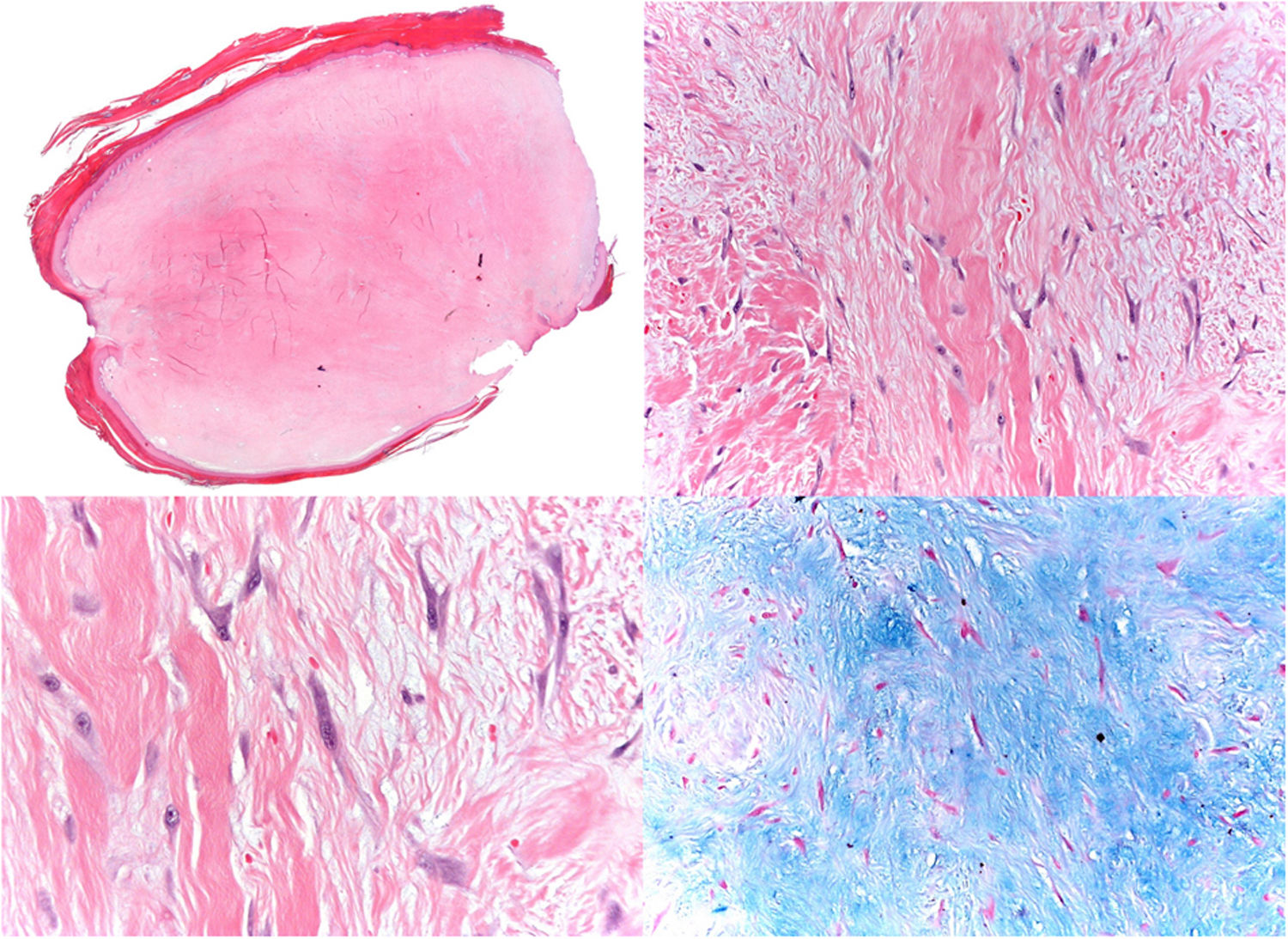
HistopathologyHistopathology showed a well-defined lesion consisting of nonatypical stellate and fusiform fibroblasts and myofibroblasts on a background of thick, dense collagen, with myxoid areas and sparse capillaries that were neither atypical nor prominent (Fig. 2). These cells were positive for vimentin, focally positive for smooth muscle actin, and negative for CD34, desmin, S100, β-catenin, AE1/AE3, and epithelial membrane antigen (EMA). Ki67 immunostaining revealed a cell proliferation index of 1%.
Additional TestsMagnetic resonance imaging (MRI) was requested, and showed a hypointense nodular lesion with smooth and slightly lobulated borders located in the subcutaneous fatty tissue at the level of the distal phalanx. A fat plane was evident between the lesion and adjacent osteotendinous structures.
No enhancement was observed after contrast administration.
What Is Your Diagnosis?
DiagnosisDesmoplastic fibroblastoma.
Clinical Course and TreatmentThe lesion was completely excised, and there was no evidence of recurrence after 18 months of follow-up.
CommentDesmoplastic fibroblastoma, also known as collagenous fibroma, is a benign soft-tissue tumor that was first described by Evans in 1995.1 The largest series (63 patients) was published by Miettinen in 1998.2
Incidence of this rare entity is higher in men than women, and the median age at diagnosis is 50 years.2 It usually manifests as a well-defined, rounded painless mass that grows slowly, although our patient’s tumor was fast-growing. Although typically small, this tumor can reach sizes of over 20cm. It is usually located on the upper limbs, lower limbs, and trunk, although intraoral,3 genital,4 and intrathoracic5 presentations have been described.
Desmoplastic fibroblastoma originates predominantly in subcutaneous or intramuscular cell tissue and, in rare cases, in bone.
Histologically, it is characterized by low cellularity and the presence of medium-sized fibroblasts on a fibromyxoid background with abundant collagen. The fibroblasts have a reactive appearance, with normochromic nuclei, visible nucleoli, and amphophilic cytoplasm. The borders are well defined, although interdigitation with fat or muscle tissue may be observed. Immunohistochemistry shows diffuse labeling for vimentin, focal positivity for actin, desmin, cytokeratin, and S-100, and negative staining for β-catenin, EMA, and CD34.
The chromosomal translocations t(2,11) and t(11,17), which affect 11q12, have been detected in this tumor. The FOSL1 gene is located nearby (at 11q13.1) and the FOSL1 protein is overexpressed, as evidenced by strong diffuse nuclear immunoreactivity for FOSL1 on immunohistochemistry. This immunoreactivity is useful to differentiate desmoplastic fibroblastoma from other diseases such as tendon sheath fibroma, although unfortunately this technique is currently not routinely available.6
The differential diagnosis includes benign and malignant fibrous tumors and reactive processes, the most common of which are nodular fasciitis, extra-abdominal fibromatosis, tendon sheath fibroma, neurofibroma, calcifying fibrous tumor, desmoid tumor, and low-grade fibromyxoid sarcoma.
Treatment consists of complete removal of the lesion, and the incidence of recurrence is low.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alcántara-González J, Carolina Pérez González Y, Rodríguez-Lopez T. Tumor de rápido crecimiento en el primer dedo del pie derecho. Actas Dermosifiliogr. 2021;112:167–168.