Psoriasis is a chronic skin condition that affects approximately 1–3% of the world's population and is known to decrease patients’ quality of life. However, it is yet to be ascertained whether the specific location of psoriatic lesions on the body influences one's quality of life.
MethodsA systematic review was conducted with a search of MEDLINE, EMBASE, and Web of Science databases. Only non-case report and non-review studies with explicitly stated body regions affected by psoriasis were included in the review.
FindingsPsoriatic patches and plaques in different areas of the body were not found to influence patients’ quality of life to differing extents.
ConclusionsWhile the body of evidence is limited and presents unstandardized results, the results of this review point to the fact that all psoriatic patches and plaques decrease patients’ quality of life, with neither one region doing so to a significantly greater extent than another.
La psoriasis es una afección crónica de la piel que afecta aproximadamente el 1-3% de la población mundial con gran impacto negativo en la calidad de vida de los pacientes. Sin embargo, aún no se ha determinado en qué medida la ubicación específica en el cuerpo de las lesiones psoriasis influye en la calidad de vida.
MétodoSe realizó una revisión sistemática con una búsqueda en las bases de datos Medline, Embase y Web of Science. En la revisión se descartaron los artículos referidos a casos clínicos y revisiones, incluyéndose solo aquellos en los que se indicó de forma explícita la evaluación por regiones corporales afectadas por psoriasis.
ResultadosNo pudo identificarse una relación entre la presencia de placas de psoriasis en diferentes áreas del cuerpo y la calidad de vida de los pacientes.
ConclusionesSi bien la evidencia es limitada y presenta resultados no estandarizados, los resultados de esta revisión permiten sugerir que la presencia de placas de psoriasis disminuyen la calidad de vida de los pacientes, sin diferencias en función de la región afectada.
Psoriasis vulgaris is a chronic immune-mediated systemic inflammatory disease that affects 1–3% of the world's population.1 It is often associated with scaly papules, patches, and plaques that may appear anywhere on the body.2 While it is known that psoriasis negatively affects the quality of life of patients, little is known about the relationship between the region(s) of the body affected by psoriasis and the quality of life.3 This systematic review strives to ascertain whether the body region affected with psoriasis can predict one's quality of life. It is hypothesized that psoriatic areas that are more visible or sensitive (face, neck, genitals) will be associated with a lower quality of life compared to psoriatic areas that are less visible, such as thighs or trunk.
MethodsA literature search using the MEDLINE, EMBASE, and Web of Science literature database was conducted using the terms (“psoriasis” AND (face OR facial OR scalp OR ear OR cheek* OR lips OR lip OR earlobe* OR forehead OR eyelid* OR nose OR chin OR jaw OR neck OR Shoulder* OR chest OR breast* OR underarm* OR axilla OR axillae OR arm OR forearm* OR elbow* OR wrist* OR hand* OR finger* OR nail* OR abdomen OR stomach OR hip OR hips OR back OR trunk OR buttock* OR leg OR legs OR thigh* OR knee* OR kneecap* OR ankle* OR shin* OR calf* OR calves OR toe OR toes OR plantar OR foot OR feet OR limb* OR Genital* OR vulv* OR labia* OR groin OR vagina* OR folds OR penile OR penis OR scrotum OR pubis OR “inverse psoriasis”) AND (“Dermatology Life Quality Index” OR “DLQI” OR “Skindex 29” OR “Skindex 17” OR “Dermatology Quality of life Scale” OR “DQOLS” OR “Psoriasis Disability Index” OR “PDI” OR “Impact of Psoriasis Questionnaire” OR “IPSO” OR “Psoriasis Index of Quality of Life” OR “quality of life scale” OR “QOLS” OR “PSORIQoL” OR “SF36” OR “EQ5D” OR MQOL OR “McGill Quality of Life scale” OR HRQOL OR “Health-related quality of life” OR WHOQOL-BREF OR “Global Quality of Life Scale” OR GQOL) AND adult).
Articles identified for inclusion met the following criteria: there was mention of the specific body part(s) affected by psoriasis; the quality of life of psoriasis patients was reported; the articles were published prior to February 14, 2021. Studies were excluded if patients’ quality of life scores accounted for more than one location of psoriasis on the body, for instance, if the patients had multiple areas of the body affected by psoriasis and their quality of life score reflected all of those areas. Additionally, articles were excluded if the studies were conference proceedings, if they did not mention where on the body patients experienced psoriasis, if they were reviews or meta-analyses, and if they were case reports.
Quality of life scalesDespite having a search strategy that accounted for a wide array of quality of life scales, the most common one reported in the included studies were the DLQI.4–6
The Dermatology Life Quality Index (DLQI) is a 10-item questionnaire used to evaluate quality of life impact and disability associated with skin disease. This questionnaire deals with many aspects of one's life, including the impact of skin disease on symptoms, one's self-perception, activities, relationships, and treatment. Patients indicate how much their skin disease affects their life for each item, with possible answers being: “very much,” “a lot,” “a little,” and “not at all.” Each response is scored on a scale from 0 to 3 and summed to get a total score out of a maximum 30 points. Thus, a higher DLQI score indicates a greater impairment of one's quality of life.
ResultsA total of 663 relevant citations were identified from the literature search (Fig. 1).7 Of these, 251 were excluded based on the title and abstract, and 301 were selected for further examination. A total of 50 articles were included in this review.8-57 See Table 1 (Supplementary material) for a summary of the included studies.
Given that studies used different quality of life scales, it was not possible to compile and average results from all studies. Hence, we compiled results from studies which used the same quality of life scale. For instance, studies whose results were based on DLQI were included with similar studies, and studies whose results were based on EQ-5D were similarly grouped together.
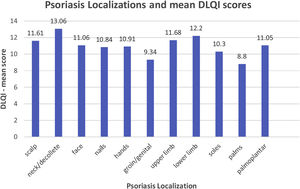
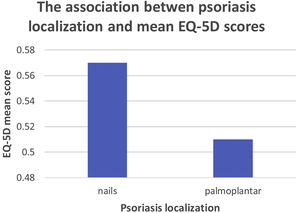
For graphical representation and statistical analysis, every psoriatic body region had to correspond to at least two studies to be included in the analysis, so as to prevent one study's results biasing the analysis. Keeping this methodology in mind, the most commonly-reported quality of life scale was the DLQI, followed by the EQ-5D, as shown in Figs. 2 and 3.
For other quality of life scales, such as Modified Finlay-Kahn questionnaire or the PDI, there were insufficient studies for compilation into a graphical format and for statistical analysis. Nevertheless, these studies’ results are reported in Table 1, Supplementary material.
At first glance, Fig. 2 appears to demonstrate that psoriasis localization on the neck/décolleté is associated with a higher DLQI score (decreased quality of life) compared to psoriasis localized to the palms, for instance. To deduce whether the differences in the quality of life between the psoriatic body regions are truly significant, the One-way ANOVA test was used. The ANOVA test results pointed to the fact that the mean DLQI scores between all of the body regions affected by psoriasis are not significantly different.
To deduce whether the results in Fig. 3 are significantly different, a T-test was used. The result of the T-test pointed to the fact that the mean EQ-5D scores of nail and palmoplantar psoriasis are also not significantly different.
DiscussionWhile it was hypothesized that more visible and/or sensitive psoriatic areas such as the face, neck, and genitals would be associated with a significantly impaired quality of life compared to less visible and/or sensitive ones, this was not the case. In fact, there was not one region of the body affected by psoriasis which was associated with a significantly worsened quality of life compared to another region. This review specifically analyzed the baseline quality of life scores of patients with various psoriatic body region involvements rather than the improvement of quality of life due to a treatment. This was done to avoid confounding the results.
The results of the study could have been affected by the limitations of the systematic review. For one, certain studies reported the quality of life associated with the involvement of specific body regions, rather than associated with those body regions in isolation. This made it difficult to deduce to what extent the impairment in quality of life was to the specific psoriatic region alone. Furthermore, studies included in this review used different quality of life scales, making it difficult to compare the results across the studies and to pool the studies’ results for analysis. This greatly reduced the maximum possible number of studies used in the analyses and hence may have biased the results. Thus, future studies are encouraged to report multiple scales if possible, especially accounting for the more conventionally-used scales. Furthermore, the inherent limitation of quality of life scales is that they may be subjective. A methodological limitation of this review was that data abstraction and review was completed by only one reviewer, thereby limiting the inter-rater reliability of study screening. Finally, this review is limited by the fact that the included studies were both observational studies and controlled trials, meaning there were varying degrees of variable and bias control. However, without this methodological limitation, the body of evidence would be insufficient to lend itself to a statistical analysis, meaning that this was a necessary limitation.
Some of the strengths of this study include the fact there was a broad search conducted, with a thorough review of studies, as well as the use of multiple databases for the search. Additionally, the statistical analysis allows for more robust conclusions to be reached.
Future studies are encouraged to be performed with a greater sample size, with each patient experiencing only one localization of psoriasis (for instance, on the scalp alone) in order to truly delineate whether there is a relationship between the body region affected by psoriasis and the quality of life. Additionally, future studies should use more common quality of life scales, such as DLQI, in order to allow for better comparison among studies. Lastly, further research can also explore to what extent treatment improves the quality of life in specific body regions and whether certain body regions’ associated quality of life improves significantly more compared to other regions affected by psoriasis. Further research may also benefit from including more parameters, such as skin area affected by psoriasis and the corresponding quality of life scores, to determine whether larger areas of skin also play a role in affecting the patients’ quality of life. Perhaps the area of skin affected by psoriasis is another confounding variable in the relationship between psoriatic sites and quality of life.
ConclusionsTo the best of our knowledge, this systematic review is the first to use worldwide data in an attempt to deduce whether specific psoriatic areas of the body affect patients’ quality of life to differing extents. The results of this review point to the fact that all psoriatic involvement arguably decrease a patient's quality of life, with neither one region doing so to a significantly greater extent than another.
Despite not arriving at the predetermined hypotheses, the results of this review are still useful in shedding light on the fact that patients with psoriasis have a decreased quality of life no matter where they have skin involvement. This can help inform importance of additional care for patients with psoriasis, including anticipation of a decreased quality of life and proactive management, such as referral for psychotherapy or patient support groups.
This review can also help patients to appreciate that no one region affected by psoriasis is predicts a significantly “better” or “worse” quality of life than another; all psoriatic regions predict a decreased quality of life.
Conflict of interestDr. Vender has received.
- •
Grants/Research Support: Abbvie, Amgen, Bausch Health, Centocor, Dermira, Dermavant, Galderma, GSK, Leo, Lilly, Takeda, Novartis, Merck, Pfizer, Regeneron, UCB.
- •
Participated in Speakers Bureau and received Honoraria: Abbvie, Amgen, Janssen, Galderma, GSK, Leo, Lilly, Merck, Novartis, Pfizer, Bausch-Health, Actelion, Celgene, Cipher, UCB.
- •
Has received Consulting Fees: Abbvie, Amgen, BMS, Janssen, Galderma, GSK, Leo, Lilly, Merck, Novartis, Palladin, Pfizer, Bausch-Health, Actelion, Celgene, Cipher, UCB.