Psoriasis is a chronic inflammatory disease associated with an increased risk of ischemic coronary artery disease (CAD) in some populations. We aimed to determine the association between these 2 diseases in our geographic area.
Material and methodWe performed a cross-sectional study of patient records between 2005 and 2012 in the database (Abucacis, Datamart) that contains all medical case histories in the province of Castellón, Spain. Patients diagnosed with psoriasis were compared with a control group of patients diagnosed with melanocytic nevus. The prevalence of CAD and the presence or absence of the main cardiovascular risk factors were analyzed in each group.
ResultsA total of 9181 patients with psoriasis and 21925 with melanocytic nevus were studied. Univariate logistic regression analysis showed that CAD was significantly associated with psoriasis, age (in years), sex, hypertension, diabetes mellitus, dyslipidemia, and obesity (P<.05). On adjustment for age, sex, and the other cardiovascular risk factors, multivariate regression analysis established that psoriasis was independently associated with CAD (P<.029).
ConclusionOur findings in a large sample of patients in a Mediterranean area support the hypothesis that patients in this population have an increased risk of ischemic CAD.
La psoriasis es una enfermedad inflamatoria crónica que se ha asociado a un aumento de riesgo de enfermedad arterial coronaria isquémica (EACI) en algunas poblaciones. El objetivo de nuestro estudio fue determinar la asociación entre psoriasis y EACI en nuestro medio.
Material y métodoSe realizó un estudio transversal en la provincia de Castellón con datos procedentes del sistema de información asistencial Abucasis (Datamart) desde el año 2005 hasta el 2012. Se seleccionó a los pacientes con psoriasis y como grupo control a los pacientes con nevus melanocítico. Se estudió la prevalencia de EACI en ambos grupos estratificando por los principales factores de riesgo cardiovascular.
ResultadosSe estudiaron 9.181 pacientes con psoriasis y 21.925 con nevus melanocítico. En el análisis de regresión logística univariante la EACI se asoció significativamente a las variables psoriasis, edad (en años), sexo, hipertensión, diabetes mellitus, dislipidemia y obesidad (p<0,05). En el análisis de regresión logística multivariante, tras ajustar por edad, sexo y el resto de los factores de riesgo cardiovascular, se establece una relación independiente entre la presencia de EACI y psoriasis (p<0,029).
ConclusiónNuestros resultados apoyan la existencia de mayor riesgo de EACI en pacientes con psoriasis en una población amplia del área mediterránea.
Psoriasis is a chronic inflammatory disease that affects 2-3% of the adult population. Its pathophysiology is characterized by immune responses mediated by type 1 and type 17 helper T lymphocytes and synthesis of various cytokines that produce inflammation of the skin and joints. Other inflammatory markers, such as C-reactive protein, are also increased at the systemic level.1 Proinflammatory mediators are involved in the onset of acute ischemic coronary artery disease (CAD), as in other chronic inflammatory diseases, such as rheumatoid arthritis or lupus erythematosus.2 The European Guidelines on cardiovascular disease prevention recently included psoriasis as a risk factor for ischemic heart disease.3
Although an association between psoriasis and acute ischemic CAD has been found in various populations,4 data for patients in the Mediterranean area are lacking, and differential characteristics for cardiovascular risk in this population have not been investigated. We designed a cross-sectional study to evaluate the association between psoriasis and risk of ischemic CAD in the province of Castellón, Spain.
The control population comprised patients with benign skin disease not caused by inflammatory processes, such as melanocytic nevus. The presence of nevus in all age groups and the absence of an association with inflammation enabled us to use these patients as a control group.
The objective of the study was to determine the prevalence of ischemic CAD in patients with psoriasis in our geographic area and to compare it with the prevalence of ischemic CAD in patients with melanocytic nevus.
Material and MethodsStudy DesignWe performed a cross-sectional study on the population of the province of Castellón using 2 groups: patients with psoriasis and patients with melanocytic nevus. Within these groups, we studied the prevalence of acute ischemic CAD depending on the corresponding diagnosis.
Datamart is the database that includes the electronic clinical history (Abucasis) for patients receiving health care in the Autonomous Community of Valencia. This database has been used in Castellón by attending physicians (both specialists and primary care physicians) since 2005. It is used by all dermatologists in Castellón. Diseases were semiautomatically coded according to the International Classification of Diseases, Ninth Revision (ICD-9) by assigning diagnoses to the patients’ clinical histories. Diagnoses must be assigned and coded before treatment can be prescribed; therefore, almost all clinicians involved in patient care enter and code the diagnoses of the diseases they treat.
The province of Castellón has 604 564 inhabitants who are attended by professionals from the health districts of Vinaroz, General de Castellón, and La Plana. The population is distributed in small population centers; the largest city has fewer than 200 000 inhabitants.5
Our inclusion criteria were age over 20 years and psoriasis or melanocytic nevus according to the codes specified in the Datamart database. We selected the ICD-9 codes for psoriasis (696), acute myocardial infarction (410, 411, and 412), angor pectoris (413),6 and melanocytic nevus-benign neoplasm of skin (216 and 448.1), which were named benign skin tumor.
The study groups were adjusted for age and sex, and the main cardiovascular risk factors in the clinical history with the corresponding ICE-9 diagnosis (sex, presence or absence of dyslipidemia, diabetes mellitus, hypertension, obesity, and smoking) were collected to verify or reject an independent association between ischemic CAD and psoriasis. Smoking is only coded in the clinical history when the patient requests cessation treatment.
The study was approved by the Ethics Committee of Hospital La Plana.
Statistical AnalysisThe differences in age between the groups were analyzed using the t test for independent samples: quantitative variables were assumed to be normally distributed because of the large sample size.
The remaining comparisons were qualitative and were analyzed using contingency tables, the chi-squared test or Pearson test in the case of large samples, and the Fisher exact test or maximum likelihood method when the samples were considered less extensive and depending on whether 2 or more groups were compared.
Statistical significance was set at P<.05.
Factors associated with ischemic CAD were assessed by constructing a binary logistic regression model in 2 steps:
- 1.
First, the univariate models were analyzed. The dependent variable was always ischemic CAD (yes vs no). The remaining variables were independent, and the odds ratio and corresponding 95% confidence interval (CI) were shown in all cases.
- 2.
Second, variables with a significance of P<.2 in the univariate analysis (to study possible multiplicative effect values among the independent variables) were used to construct a forward stepwise model in which the entry significance level was P<.1 and the exit significance level was P>.15.
Patients who simultaneously presented both main study diagnoses (psoriasis and benign skin tumor) were excluded from the analysis.
All the analyses were performed using SPSS, version 19.0 (IBM Corp).
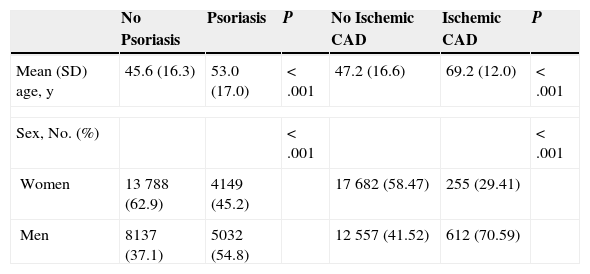
ResultsIschemic Coronary Heart Disease in Patients With Psoriasis and in Patients With Benign Skin TumorWe excluded 525 patients with a simultaneous diagnosis of benign skin tumor and psoriasis. Valid data were obtained for analysis from 31 106 patients. Of these, 9181 (29.5%) had psoriasis, and the remainder had benign skin tumor. There were 13 169 men (42.3%) and 17 937 women (57.7%). The mean (SD) age of the study participants was 47.9 (16.9) years; in patients without psoriasis, mean age was 45.6 (16.3) years, and in those with psoriasis, it was 53.0 (17.0) years (P<.001). Among patients without psoriasis, 62.89% were women and 37.11% were men. In the psoriasis group, 45.19% were women and 54.81% were men. The mean (SD) age of patients with ischemic CAD was 69.2 (12.0) years compared with 47.2 (16.6) years in patients without ischemic CAD (P<.001). Women accounted for 58.47% of patients without ischemic CAD and men 41.52%; women accounted for 29.41% of patients with ischemic CAD and men 70.59% (Table 1). Therefore, we adjusted the model for age and sex in order to analyze the association between psoriasis and ischemic CAD.
Sex and Age According to Psoriasis and Ischemic CAD.
| No Psoriasis | Psoriasis | P | No Ischemic CAD | Ischemic CAD | P | |
|---|---|---|---|---|---|---|
| Mean (SD) age, y | 45.6 (16.3) | 53.0 (17.0) | <.001 | 47.2(16.6) | 69.2(12.0) | <.001 |
| Sex, No. (%) | <.001 | <.001 | ||||
| Women | 13 788 (62.9) | 4149 (45.2) | 17 682 (58.47) | 255 (29.41) | ||
| Men | 8137 (37.1) | 5032 (54.8) | 12 557 (41.52) | 612 (70.59) | ||
Abbreviation: CAD, coronary artery disease.
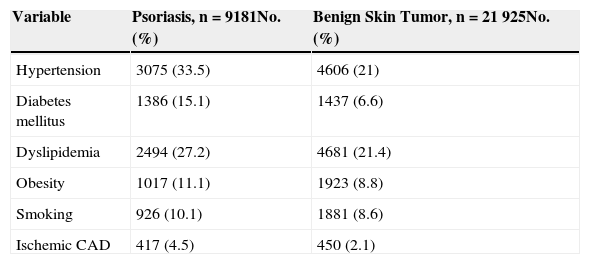
Table 2 shows the distribution of risk factors for ischemic CAD in the psoriasis group and control group (benign skin tumor). The frequency of hypertension, diabetes mellitus, dyslipidemia, obesity, and smoking was greater in patients with psoriasis.
Frequency of Risk Factors for Ischemic CAD in the Study Population.
| Variable | Psoriasis, n=9181No. (%) | Benign Skin Tumor, n=21 925No. (%) |
|---|---|---|
| Hypertension | 3075 (33.5) | 4606 (21) |
| Diabetes mellitus | 1386 (15.1) | 1437 (6.6) |
| Dyslipidemia | 2494 (27.2) | 4681 (21.4) |
| Obesity | 1017 (11.1) | 1923 (8.8) |
| Smoking | 926 (10.1) | 1881 (8.6) |
| Ischemic CAD | 417 (4.5) | 450 (2.1) |
Abbreviation: CAD, coronary artery disease.
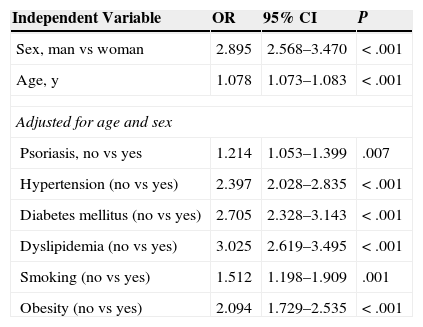
In the univariate logistic regression analysis adjusted for age and sex with ischemic CAD (no vs yes) as the dependent variable and psoriasis, age (in years), sex, and presence of hypertension, diabetes mellitus, dyslipidemia, obesity, and smoking as independent variables, we found a significant association for all the variables (Table 3).
Logistic Regression Analysis With Total Ischemic CAD in Psoriasis Compared With Benign Skin Tumora
| Independent Variable | OR | 95% CI | P |
|---|---|---|---|
| Sex, man vs woman | 2.895 | 2.568–3.470 | <.001 |
| Age, y | 1.078 | 1.073–1.083 | <.001 |
| Adjusted for age and sex | |||
| Psoriasis, no vs yes | 1.214 | 1.053–1.399 | .007 |
| Hypertension (no vs yes) | 2.397 | 2.028–2.835 | <.001 |
| Diabetes mellitus (no vs yes) | 2.705 | 2.328–3.143 | <.001 |
| Dyslipidemia (no vs yes) | 3.025 | 2.619–3.495 | <.001 |
| Smoking (no vs yes) | 1.512 | 1.198–1.909 | .001 |
| Obesity (no vs yes) | 2.094 | 1.729–2.535 | <.001 |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; OR, odds ratio.
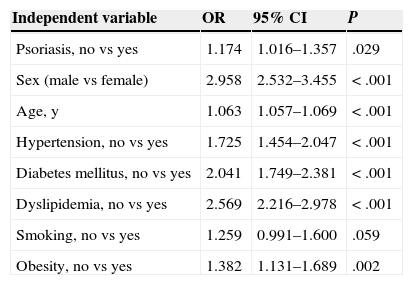
In the multivariate logistic regression analysis, we detected an independent association between the presence of ischemic CAD and psoriasis (P<.029) adjusted for age, sex, and the other risk factors. The presence of psoriasis increases the possibility of ischemic CAD 1.17 times (95% CI, 1.02-1.36). This independent association was also observed for the remaining variables known to be risk factors for ischemic CAD (smoking, hypertension, diabetes mellitus, and dyslipidemia), except smoking (P=.059) (Table 4).
Multivariate Logistic Regression Analysis with Ischemic CAD in Patients With Psoriasis Compared With Patients Without Psoriasis.
| Independent variable | OR | 95% CI | P |
|---|---|---|---|
| Psoriasis, no vs yes | 1.174 | 1.016–1.357 | .029 |
| Sex (male vs female) | 2.958 | 2.532–3.455 | <.001 |
| Age, y | 1.063 | 1.057–1.069 | <.001 |
| Hypertension, no vs yes | 1.725 | 1.454–2.047 | <.001 |
| Diabetes mellitus, no vs yes | 2.041 | 1.749–2.381 | <.001 |
| Dyslipidemia, no vs yes | 2.569 | 2.216–2.978 | <.001 |
| Smoking, no vs yes | 1.259 | 0.991–1.600 | .059 |
| Obesity, no vs yes | 1.382 | 1.131–1.689 | .002 |
Abbreviations: CAD, ischemic coronary artery disease; CI, confidence interval; OR, odds ratio.
The Hosmer-Lemeshow test of goodness of fit was performed with the residuals to determine whether the model was robust to changes in the values of the variables. The significance value of P=.258 obtained indicates that our model was reliable and robust.
DiscussionSeveral studies have investigated the association between psoriasis and cardiovascular disease based on inflammatory mechanisms that are common to both diseases. The results of the studies are very different, and an association was found between the diseases in some7–10 but not in others.2,11 In their review of the association between psoriasis and cardiovascular disease, Dauden et al.4 examined 15 studies from the last decade in the United Kingdom, Germany, United States, Taiwan, and Israel. These studies revealed a greater risk among patients with psoriasis.4 Studies that evaluate cardiovascular risk cannot be directly extrapolated from one European country to another. Significant differences have been found in the incidence of ischemic CAD between European countries; therefore, it has been proposed that cardiovascular risk should be evaluated taking into account the relevant geographic area.12,13 In Spain, the various studies on psoriasis and cardiovascular risk were performed among hospital patients; therefore, no results are available for the general population.14
A meta-analysis of published studies revealed an association between psoriasis and cardiovascular disease, as well as between psoriasis and other cardiovascular risk factors. However, these associations disappear in studies from population databases.14 Unlike other studies,14,15 ours is not subject to bias stemming from the selection of hospital patients only, since it includes both hospital patients and outpatients seen by dermatologists and cardiologists or family physicians; therefore, it includes mild, moderate, and severe psoriasis in the same proportion as in the general population. This is possible because of the characteristics of our health system, which provides almost universal care. The age- and sex-adjusted multivariate analysis showed that psoriasis is an independent cardiovascular risk factor. The presence of an association between ischemic CAD and any type of psoriasis (whether extensive or not) confirms psoriasis as an independent cardiovascular risk factor, although this does not rule out the possibility that risk could increase with severity. Given that 2% to 3% of the Spanish population have psoriasis (80% mild and 20% moderate to severe),16 the number of patients potentially exposed to this risk factor is high. According to European guidelines on cardiovascular disease prevention,3 this observation would support prevention of cardiovascular disease from an early age, and more so in persons with risk factors such as psoriasis. Other unanswered questions requiring different types of study include whether a patient with psoriasis could benefit from primary prevention with drugs to treat ischemic CAD or whether more aggressive treatment of psoriasis would reduce cardiovascular risk.
An association between psoriasis and other cardiovascular risk factors such as hypertension, diabetes mellitus, dyslipidemia, and obesity has been reported in several countries.7,8,10,16 In our setting, where the presence of cardiovascular risk factors is greater in psoriatic patients, the fact that the population traditionally follows a Mediterranean diet, lives in small towns, enjoys universal health care, and is scarcely affected by the disadvantages typical of an urban lifestyle (eg, type of diet, frequent use of cars) leads us to ask, as did Gelfland et al.,10 whether psoriasis and ischemic CAD are not only associated with inflammation, but whether they are also the product of factors such as stress, a sedentary lifestyle, or low control of cardiovascular risks. Parodi et al.17 recently carried out a study in a Mediterranean population in Italy in which they found an association between psoriasis and other cardiovascular risk factors, although the study sample did comprise hospital patients. Population studies are necessary to determine whether psoriasis is associated with other cardiovascular risk factors.
The lack of an association between ischemic CAD and smoking in the present study is due to coding bias. Until recently, smoking was only routinely coded in the database when patients requested help with cessation. Although smoking is now recorded and coded at the primary care visit, our data were collected before this change was made.
The present study could be limited by the fact that diagnostic error cannot be ruled out during coding; however, we feel this possibility is minimal owing to the size of our database. Coding of ischemic heart disease is usually best recorded in the clinical history taken by the family physician because of its implications for prognosis and treatment. Furthermore, ours is a population-based, cross-sectional study with the methodological limitations inherent to its design, namely, it is not possible to establish the time sequence between ischemic CAD and psoriasis, and what we call risk factors could also be factors associated with more chronic disease or greater survival. Similarly, we do not distinguish between degrees of psoriasis. The diagnosis of psoriasis was taken as categorical, since we were interested in considering psoriasis as a risk factor. We excluded cases with concomitant diagnoses of psoriasis and nevus to differentiate clearly between the control group and the study group. We felt that the minimum bias this could cause was less important than the potential confusion of including it in the study.
Our results point to an increased risk of ischemic CAD in patients with psoriasis in the Mediterranean area. Further studies would be necessary to determine whether treatment of psoriasis or primary prevention based on drug therapy would reduce this risk.
Ethical DisclosuresProtection of persons and animalsThe authors declare that this research did not involve experiments performed on humans or animals.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mahiques-Santos L, Soriano-Navarro C.J, Perez-Pastor G, Tomas-Cabedo G, Pitarch-Bort G, Valcuende-Cavero F. Psoriasis y enfermedad arterial coronaria isquémica. Actas Dermosifiliogr. 2015;106:112–116.