Skin lesions are a common reason for consulting a primary care physician. Current legislation in Spain states that purely aesthetic skin problems that do not pose a health problem are not to be treated within the National Health Service. The aim of this study was to estimate the proportion of referrals from primary care physicians to dermatologists that were for cystic lesions or benign tumors and could potentially have been avoided.
Material and methodsWe consulted cases registered in the DIADERM study dataset, which is representative of dermatology practice in Spain, and collected the main diagnoses given on referring patients from primary care. A referral diagnosis was classified as potentially avoidable if it corresponded to one of the primary care discharge diagnoses listed in a consensus paper of the Andalusian section of the Spanish Academy of Dermatology and Venereology (AEDV).
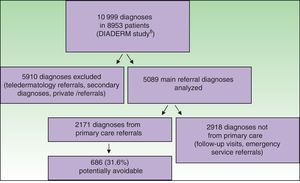
ResultsWe collected 2171 main reasons for first-visit referrals to dermatologists; 686 of them (31.6%) were for cystic lesions or benign tumors and classified as potentially avoidable. In 478 cases (22%) the patients were discharged on the first visit. The most frequent diagnoses in such cases were seborrheic keratosis (9.3%) and melanocytic nevus (8.6%).
ConclusionsNearly a third of referrals from primary care to a dermatologist were for cystic lesions and benign tumors and could have been avoided. A clearer understanding of our caseload can be useful for improving planning, training, and health care system management.
Las lesiones cutáneas constituyen un motivo de consulta frecuente en Atención Primaria (AP). Aquellas que no supongan un problema de salud, sino una cuestión estética, no deben ser tratadas en el Sistema Nacional de Salud, según la legislación vigente. El objetivo de este trabajo es estimar qué porcentaje de derivaciones remitidas desde AP a Dermatología por lesiones quísticas o tumores benignos corresponde a lesiones que podríamos considerar potencialmente evitables.
Material y métodoUtilizamos los diagnósticos principales de los pacientes derivados de AP, recogidos en el estudio representativo nacional DIADERM. Cada uno de los diagnósticos derivados fue clasificado como potencialmente evitable si se correspondía con alguno de los diagnósticos con criterio de alta desde AP, establecidos en el documento de consenso propuesto por la sección territorial andaluza de la Academia Española de Dermatología y Venereología.
ResultadosSe recogieron datos de 2.171 motivos principales de consulta derivados de AP como primeras consultas. De estos, 686 (31,6%) son diagnósticos que podrían corresponderse con derivaciones potencialmente evitables por lesiones quísticas o tumorales benignas. Un 22% (478) del total de las consultas fueron dadas de alta en la primera visita. Los diagnósticos más frecuentes entre estos fueron las queratosis seborreicas (9,3%) y los nevus melanocíticos (8,6%).
ConclusionesLa proporción de derivaciones potencialmente evitables a Dermatología desde AP por lesiones quísticas y tumorales benignas supone casi un tercio de las consultas. El conocimiento de la realidad asistencial de nuestro entorno puede ser útil para mejorar la planificación, la formación y la gestión sanitaria.
The prevalence of skin lesions is high in the general population, and they have come to figure among the main reasons for consulting primary care physicians.1,2 Many of these lesions are benign, having no impact on the individual's health, and care is usually sought for purely aesthetic reasons.3 Spanish Royal Decree 1030/2006 of September 15 excludes procedures and treatments that have only cosmetic outcomes from the list of services covered by the public National Health Service (NHS).4 Dermatology-related visits for minor lesions nevertheless accounted for up to 25% of primary care consultations in one Spanish study.3 The primary care family practitioner currently provides the first line of care in the NHS and is the one who decides whether to refer a patient to a dermatologist or not.5,6 The Andalusian section of the Spanish Academy of Dermatology and Venereology (AEDV), working with the Spanish Society for Quality in Health Care (SECA), recently published a consensus paper recommending a care process for persons with cystic lesions or benign tumors.7
The present study aimed to estimate the percentage of primary care referrals to dermatologists for cystic lesions or benign tumors that might be avoided. The results should provide real data for assessing the magnitude of the problem nationwide and for drafting health care policies.
Material and MethodsData were taken from the AEDV's DIADERM study of 2016,8 which surveyed a representative sample of dermatologists practicing in Spain. The 2224 members of the AEDV in November 2014 were stratified according to geographic area and sampled randomly so that the respondents would represent dermatologists across the country. The surveyed dermatologists reported all diagnoses made over a period of 6 days (3 days during cold weather and 3 days during hot weather). An expert coded the diagnoses according to version 10 of the International Classification of Diseases. Each patient visit was associated with a single principal diagnosis.
We extracted the diagnoses that were the main reason for a referral to dermatology by a primary care physician in the NHS. Teledermatology consultations were excluded.
A referral was classified as potentially avoidable if the diagnosis was one of those that could have been discharged from primary care, as established by the 2016 consensus paper of the Andalusian section of the AEDV (Table 1).7 Such cases can be discharged from primary care provided malignancy is not suspected and there is no doubt about the diagnosis, no functional impact, and no history of resistance to treatment in the case of viral infections. Referrals were not classified as potentially avoidable if they met appropriate referral criteria, such as would be the case for an atypical nevus.
Criteria for Discharge From Primary Care Without Referral to Dermatology and Criteria for Treatment by a Dermatologist
| Diagnosis | Discharge From Primary Care | National Health Service Dermatologist Can Treat |
|---|---|---|
| Melanocytic nevus | Common melanocytic nevus not meeting ABCDE criteria | Diagnosis is in doubt, malignancy is suspected |
| Seborrheic keratosis | Clinically typical seborrheic keratosis | Diagnosis is in doubt, malignancy is suspected |
| Dermatofibroma | Clinically typical dermatofibroma | Diagnosis is in doubt, malignancy is suspected |
| Acrochordon | Clinically typical acrochordons with no indication for surgery (ie, not large lesions or those in locations that objectively cause functional problems, such as the perianal area or the groin) | Diagnosis is in doubt, malignancy is suspected |
| Vascular lesion | Ruby points, venous lakes, spider veins | Diagnosis is in doubt, malignancy is suspected, neonatal lesions, pyogenic granuloma, angiokeratoma |
| Cyst | Small, asymptomatic epidermal cyst with no functional impact | Diagnosis is in doubt, malignancy is suspected |
| Lipoma | Firm diagnosis, no suspicion of malignancy, small lesions with no functional impact | Diagnosis is in doubt, malignancy is suspected, neonatal lesions, pyogenic granuloma, angiokeratoma |
| Common or plantar wart, molluscum contagiosum | Asymptomatic common warts or molluscum not resistant to initial treatment | Diagnosis is in doubt, resistance to treatment, functional impact |
| Onychocryptosis (ingrown nail) | After effective treatment (confirmed by clinical inspection and pathologic examination) | Recurrence after surgical removal, uncertain diagnosis |
| Milium cyst | Firm diagnosis, no suspicion of a neoplastic process | Diagnosis is in doubt, malignancy is suspected |
| Sebaceous hyperplasia | Firm diagnosis, no suspicion of a neoplastic process | Diagnosis is in doubt, malignancy is suspected |
| Fibrous papule | Firm diagnosis, no suspicion of a neoplastic process | Diagnosis is in doubt, malignancy is suspected |
| Syringoma | Firm diagnosis, no suspicion of a neoplastic process | Diagnosis is in doubt, malignancy is suspected |
| Xanthoma | Firm diagnosis, no suspicion of a neoplastic process | Diagnosis is in doubt, malignancy is suspected |
Abbreviation: ABCDE, asymmetry, border irregularity, color that is not uniform, diameter > 6mm, evolving size or shape or color.
a Source: Moreno-Ramírez et al.7
A record of the primary care physician's justification for the referral was not available. An indirect indicator of a referral's appropriateness was the decision taken by the dermatologist during the first visit. We assumed that patients who were discharged on the first dermatology visit underwent no dermatologic procedure; if the dermatologist had intervened, there would have been an order for pathology and/or follow-up observation of a scar. The patients with a main diagnosis included in the consensus paper's list and who were discharged by the dermatologist after the first visit might have been referred because of a primary care physician's reasonable doubt that was resolved by the dermatologist; alternatively, their cases might consitute potentially avoidable referrals. On the other hand, if the dermatologist did not discharge the patient, the referral might also have represented either an appropriate one or poor use of resources by the dermatologist.
The DIADERM study8 was classified as observational non-postauthorization research by the Spanish Agency of Medicines and Healthcare Products (AEMP) and approved by the research ethics committee of the province of Granada on October 8, 2014.
Descriptive statistics (absolute frequency and percentage) were compiled and the χ2 test was used to compare qualitative variables using Stata statistical software (version 14.2, Statacorp, Texas, USA).
ResultsThe DIADERM dataset included 10999 diagnosed cases in 8953 patients. Once we had excluded the teledermatolgy cases, the secondary reasons for consulting a physician, and the cases registered by physicians outside the NHS, there were 5089 diagnoses registered as the main reasons patients consulted a physician available for analysis. Of these, 2171 (42%) were first registered from a primary care clinic of the NHS (Fig. 1). The 2918 remaining diagnoses were excluded because they involved follow-up visits, emergency visits, or referrals from other specialists.
Six hundred eighty-six of the 2171 cases (31.6%) were classified as potentially avoidable referrals; 478 of them (22%) were discharged after the first specialist visit (Table 1). The percentage of cases discharged by the dermatologist on the first visit was significantly higher in the group of 686 potentially avoidable referrals than in the others (69.7% vs 39.1%, respectively; P<.001, χ2 test). The percentages of potentially avoidable referrals (Table 2) were similar in all the geographic areas of Spain (P=.74, χ2 test).
Absolute and Relative Frequency of Initial Primary Care Referrals and Dermatology Discharges for Diagnoses Listed in the Andalusian Consensus Statement7
| Diagnosis | Potentially Avoidable Referrals, n (%)a | Cases Discharged After a First Dermatology Visit, n | Cases Discharged After a First Dermatology Visit, % of Totala | First-visit Dermatology Discharges, % of Main Referral Diagnosisb |
|---|---|---|---|---|
| Seborrheic keratosis | 201 (9.3) | 180 | 8.3 | 89.6 |
| Melanocytic nevus | 187 (8.6) | 118 | 5.4 | 63.1 |
| Common or plantar wart, molluscum contagiosum | 135 (6.2) | 85 | 3.9 | 63 |
| Acrochordons | 52 (2.4) | 39 | 1.8 | 75 |
| Cyst | 45 (2.1) | 10 | 0.5 | 22.2 |
| Vascular lesion | 25 (1.2) | 18 | 0.8 | 72 |
| Dermatofibroma | 13 (0.6) | 8 | 0.4 | 61.5 |
| Onychocryptosis (ingrown nail) | 12 (0.6) | 8 | 0.4 | 66.7 |
| Lipoma | 7 (0.3) | 4 | 0.2 | 57.1 |
| Fibrous papule | 3 (0.1) | 3 | 0.1 | 100 |
| Xanthoma | 3 (0.1) | 2 | 0.1 | 66.7 |
| Sebaceous hyperplasia | 2 (0.1) | 2 | 0.1 | 100 |
| Milium cyst | 1 (0.05) | 1 | 0.05 | 100 |
| Syringoma | 0 (0) | 0 | 0 | 0 |
| Total | 686 (31.6) | 478 | 22 | 69.7 |
The largest group was made up of potentially avoidable referrals for seborrheic keratosis, which accounted for 201 visits (9.3%). Seborrheic keratosis was also the discharge diagnosis reached most often by dermatologists, who recorded it after 180 out of the 201 first visits (89.6%) that named this condition as the main reason for consulting the specialist. Referrals for melanocytic nevi and the group of lesions comprised of common or plantar warts or molluscum contagiosum infections accounted for 8.6% and 6.2% of the referrals, respectively. However, the percentages of first-visit discharges by dermatologists were somewhat lower for these 2 referral diagnoses, at 63% in both cases (118 out of 187 and 85 out of 135 referrals, respectively).
DiscussionThis study found that approximately 32% of referrals from primary care to dermatology in the Spanish NHS concerned the conditions included in the Andalusian consensus paper on cystic lesions or benign tumors7 and might therefore be classified as avoidable referrals in the absence of diagnostic doubt or functional impact. Seborrheic keratosis, melanocytic nevus, the group comprising common or plantar warts and molluscum contagiosum, and acrochordons and cysts account for 28.6% of the skin conditions referred from primary care to dermatology. As expected, a significantly higher proportion of visits for these conditions were discharged by the dermatologist after the first visit, suggesting that they may have been potentially avoidable. Such referrals for minor skin problems consume human and material resources but provide scant added value in terms of the population's health and may even violate current legislation.5
The consensus statement of the Andalusian section of the AEDV7 and the model for the practice of dermatology issued by the department of health of the government of Catalonia (Departament de Salut, Generalitat de Catalunya)9 are examples of efforts intended to increase the ability of primary care physicians to resolve benign lesions and skin conditions that are not complex in order to improve efficiency.
The percentage of dermatology referrals from primary care that our study identified as potentially avoidable was similar to the percentage of requests for treatment for aesthetic purposes in a study by Macaya-Pascual et al3 in an outpatient clinic of the NHS in L’Hospitalet de Llobregat, near Barcelona. Similarly, a study by Lowell et al2 reported that 29.4% of referrals to a dermatologist were for benign tumors.
Avoidable referrals in large numbers put pressure on the routine practice of dermatology, taking time that could be dedicated to other skin diseases that have greater impact on health.5 According to the previously cited study by Macaya-Pascual et al,3 the diagnosis and treatment of these conditions in a single dermatology practice in a Spanish outpatient clinic that attends 7500 visits each year would cost some €317000 per year. This figure points to a need for strategies to make the system more efficient nationwide by applying consensus-based recommendations, such as are outlined in the Andalusian statement,7 and by improving contact with primary care physicians through teledermatology.10 This approach, which is already in place in many centers, offers an effective way to manage communication between care levels and would probably help to reduce the number of potentially avoidable referrals.11
Our study's main strength is that it is based on the DIADERM registry, which reflects a stratified random selection of cases from dermatologists working in all the territories where members of the AEDV practice.8 The information, therefore, is a representative reflection of dermatology practice throughout Spain.
An important limitation of the study is that we have no information about the circumstances justifying the primary care physicians’ referrals, which would be appropriate in the presence of diagnostic doubt or functional impact. Therefore we can only speculate on the maximum impact of applying the recommendations of the Andalusian consensus statement.7 Cases discharged because they were resolved during the first visit to the dermatologist may have involved either avoidable referrals or appropriate ones (because of the primary care physicians’ doubts). Cases in which the dermatologist scheduled a second visit or a surgical procedure might also have been either appropriate or inappropriate use of resources. Thus, it is possible that the proportion of truly avoidable referrals, according to the definitions of the consensus statement,7 might be as low as 0% or as high as 31.6% of first visits to the dermatologist. More likely, however, the real percentage lies between the extremes. Another limitation derives from our study's focus on cystic lesions and benign tumors (including common warts, molluscum contagiosum, and onychogryphosis as listed by the Andalusian recommendations7). If a similar model were applied to all the reasons for referral, including infectious and inflammatory conditions, the potential impact could be greater. Finally, although the Andalusian section of the AEDV's consensus statement was drafted with the collaboration of the SECA and knowledgeable, clinically experienced dermatologists, it must be admitted that neither primary care physicians nor patients were consulted. Nonetheless, administrators of public agencies, who are charged with representing patients’ needs, did participate. In any case, we believe that future consensus statements should involve both the aforementioned stakeholders in the care process.12
In conclusion, this is the first study to analyze potentially avoidable referrals for cystic lesions and benign tumors from primary care to dermatology throughout Spain. The findings show that these referrals account for a high proportion of the dermatology caseload and that the most common diagnoses are seborrheic keratosis, melanocytic nevus, and the group comprising warts and molluscum contagiosum. We have provided information that can be useful for health care planning and training to optimize available resources as well as for designing future studies. Conclusions should take into consideration the limitations discussed above, the real possibilities of the health care situation of Spain, and the need for continuity between primary and specialist care.
FundingThe DIADERM study, which is supported by the Healthy Skin Foundation of the Spanish Academy of Dermatology and Venereology (AEDV), received funding from Novartis. This pharmaceutical laboratory, however, did not participate in gathering or analyzing data, interpreting results, or drafting the final report.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The DIADERM project was made possible thanks to the collaboration of regional coordinators and local participants.
Coordinators and participants: Section coordinators: Agustín Buendía, Pablo Fernández-Crehuet, Husein Husein-ElAhmed, Jesús Vega, Agustín Viera, José Manuel Carrascosa, Marta Ferrán, Enrique Gómez, Lucía Ascanio, Ignacio García Doval, Salvador Arias-Santiago, and Yolanda Gilaberte.
Participants: Juan A. Sánchez, Amalia Serrano, Rosa Castillo, Ramón Fernandez, José Armario, Carolina Lluc Cantalejo, Cristina Albarrán, María Cruz Martín, Juan Antonio Martín, Román Barabash, Lara Pérez, Manuel Salamanca, Carlos Hernández, José Francisco Millán, Inmaculada Ruiz, Susana Armesto, Marta González, Valia Beteta, Concepción Cuadrado de Valles, Pilar Cristóbal, María Magdalena Roth, Juan Garcias, Ricardo Fernández de Misa, Estela García, María del Pino Rivero, José Suárez, Birgit Farthmann, Alba Álvarez, Irene García, Caridad Elena Morales, María Cristina Zemba, Trinidad Repiso, Carmen Sastre, María Ubals, Alejandro Fernández, Urbà González, Ramón Grimalt, Sara Gómez, Ingrid López, Franco Antonio Gemigniani, María José Izquierdo, Fernando Alfageme, Nuria Barrientos, Laura María Pericet, Santiago Vidal, Celia Camarero, Pablo Lázaro, Cristina García, María Pilar de Pablo, Pedro Herranz, Natalia del Olmo, María Castellanos, Natalia Jiménez, Sonsoles Aboín, Isabel Aldanondo, Adriana Juanes, Dulce María Arranz, Olga González, Luis Casas, Juan José Vázquez, Carmen Peña, José Luis Cubero, Carlos Feal, María Eugenia Mayo, Nicolás Iglesias, Rafael Rojo, Elfidia Aniz, Sabrina Kindem, Nerea Barrado, Marisa Tirado, Ester Quecedo, Isabel Hernández, Antonio Sahuquillo, Rebeca Bella, Ramón García, Anaid Calle, Francesc Messeguer, Alberto Alfaro, Luisa Casanova, Libe Aspe, María Pilar Moreno, Izaskun Trébol, Gonzalo Serrano, Víctor Manuel Alcalde, Patricia García, and Carmen Coscojuela.
Please cite this article as: González-Cruz C, Descalzo MÁ, Arias-Santiago S, Molina-Leyva A, Gilaberte Y, Fernández-Crehuet P, et al. Análisis de la proporción de derivaciones potencialmente evitables desde Atención Primaria a Dermatología por lesiones quísticas o tumorales benignas en España. Datos del estudio DIADERM. Actas Dermosifiliogr. 2019;110:659–665.