A 52-year-old male farmer with a history of generalized plaque psoriasis and psoriatic arthritis was being treated with etanercept 50mg once weekly for 3 years with a good response. He presented to our department with painful erythematous nodular lesions on the right forearm (Fig. 1A) and in the left periorbital region (Fig. 1B). The lesions had appeared 10 days earlier, following a rabbit bite on the forearm. There were no associated systemic symptoms or fever.
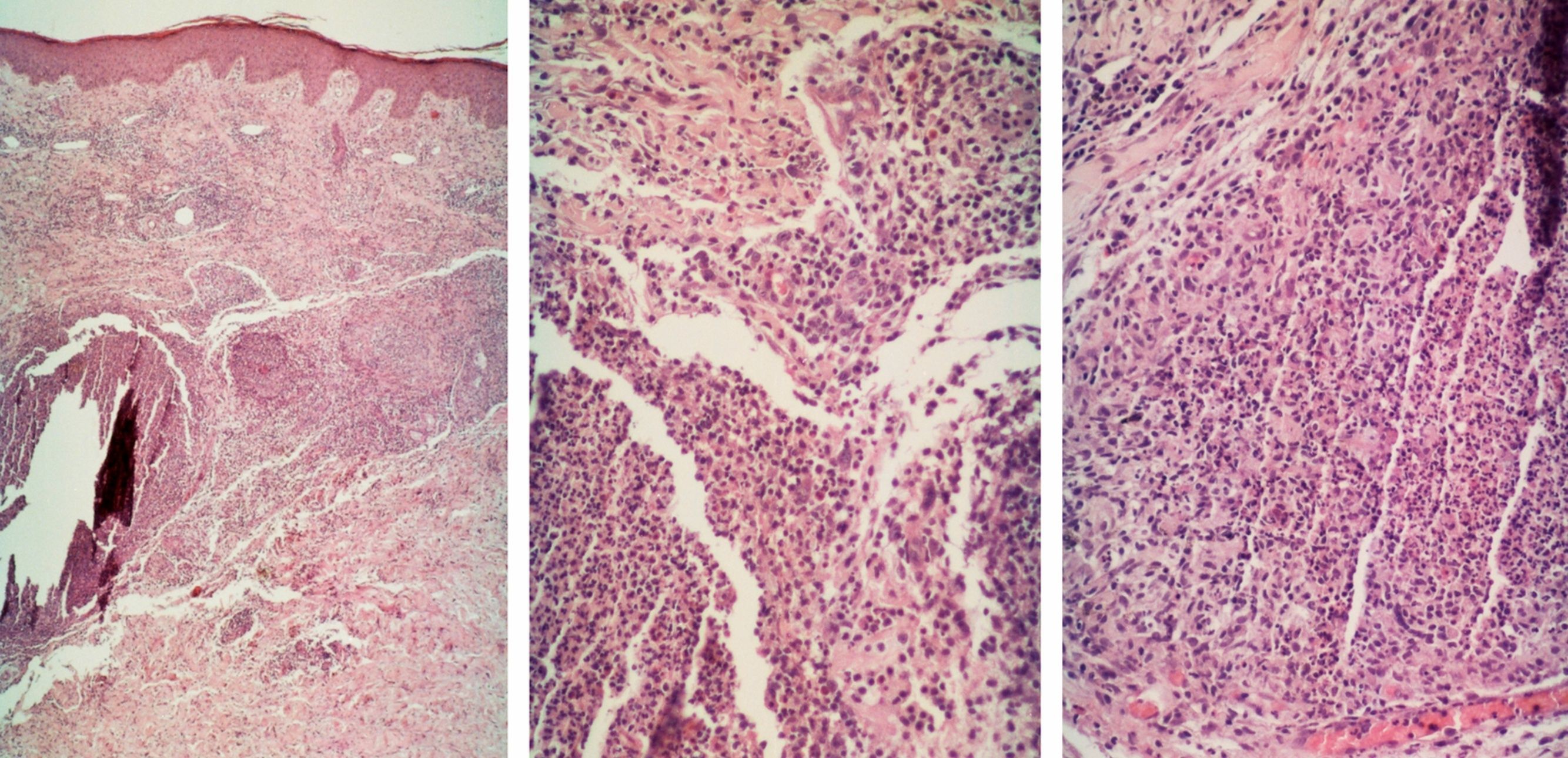
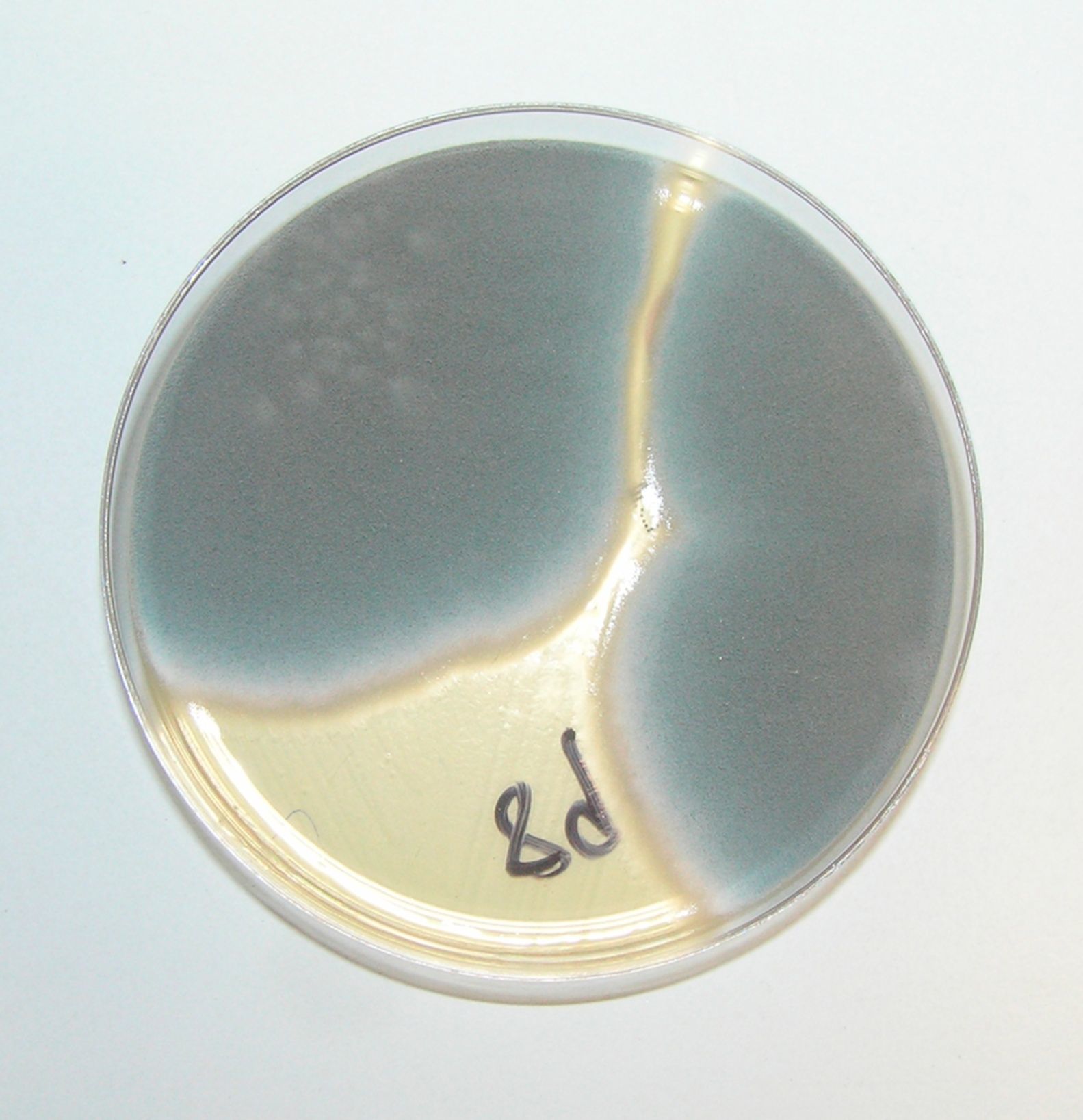
A cutaneous biopsy was performed, and as we suspected a fungal infection, the patient was started on itraconazole 100mg twice daily and etanercept was withdrawn. The biopsy showed an inflammatory infiltrate consisting primarily of polymorphonuclear cells forming abscess-like areas (Fig. 2). Periodic acid-Schiff (PAS) and Grocott-Gomori methenamine-silver staining did not reveal any fungi, but skin culture on solid Sabouraud medium with gentamicin and chloramphenicol (25°C) revealed Aspergillus fumigatus (Fig. 3). The potassium hydroxide (KOH 10%) test did not show hyphae in the microbiological sample and the polymerase chain reaction (PCR) for fungal DNA in the skin was negative. Blood tests and the chest X-ray were normal.
The lesions resolved completely with 4 weeks of treatment with itraconazole. One week after the end of treatment, the patient restarted etanercept and developed no further lesions.
Aspergillus species are ubiquitous and infection occurs most commonly in immunosuppressed individuals,1–3 like our patient; indeed, after Candida species, these fungi are the most frequent opportunistic pathogens in this group of patients.1,2 Cutaneous aspergillosis is normally a manifestation of disseminated disease, which typically begins as a pulmonary infection.1 Primary cutaneous aspergillosis is rare but it can occur, especially in the case of skin injury,4 such as that caused by a rabbit bite.
The skin manifestations of cutaneous aspergillosis are non-specific but are usually characterized by erythematous to violaceous indurated nodules progressing to ulcers with a central eschar.1 In our case, an early diagnosis prevented this progression.
The erythematous nodules on the forearm of our patient were distributed in a sporotrichoid (lymphocutaneous) pattern, which is seen more often in sporotrichosis and atypical mycobacterial infections (particularly due to Mycobacterium marinum) than in aspergillosis. Other unusual agents associated with the sporotrichoid pattern are Nocardia species, pyogenic bacteria (Staphylococcus aureus, Streptococcus pyogenes), and Pseudallescheria boydii. Noninfectious causes of this pattern include lymphoma, Langerhans cell histiocytosis, and in-transit metastases. Additionally, perineural spread of leprosy can mimic a lymphocutaneous pattern.5
The patient also had periorbital lesions, which probably resulted from self-inoculation, with the forearm being the most likely portal of entry.
A diagnosis of aspergillosis is supported by the presence of septated hyphae with acute-angle branching under microscopic examination with special fungal stains (PAS, Grocott),1,4 but it must be confirmed by culture.4 In disseminated disease, which was not the case in our patient, the serum galactomannan antigen detection test is useful to establish an early diagnosis.6 PCR-based testing, which was negative in our case, has yet to be standardized and validated for this purpose.6
There are no treatment guidelines for primary cutaneous aspergillosis as there are for disseminated disease,6 but reported cases have been successfully treated with amphotericin B, itraconazole, or voriconazole, with or without surgical ressection.2–4,7 Cutaneous aspergillosis may respond better to treatment than other forms of aspergillosis because it is recognized early, hence allowing rapid institution of treatment,3 as occurred in our case.
Our patient was immunosuppressed due to treatment with etanercept. There are no published data about primary cutaneous aspergillosis in patients treated with tumor necrosis factor-α (TNF-α) blockers but disseminated aspergillosis accounts for 23% of invasive fungal infections in these patients.8 TNF-α appears to have an important role in host defenses against A. fumigatus, enhancing leukocyte recruitment9 and phagocytosis.10 Furthermore, TNF-α blockade has been seen to increase mortality in animal models infected with Aspergillus.9 TNF-α blockade appears to increase susceptibility to fungal infections via the following mechanisms: decreased production of interferon-γ with decreased cellular immune response, decreased toll-like receptor 4 expression with diminished fungal recognition ability, and decreased granuloma formation and phagocytosis.11
To the best of our knowledge, this is the first report of primary cutaneous aspergillosis in a patient with psoriasis treated with a TNF-α blocker. Our case shows the need to monitor patients treated with these blockers and to retain a high index of suspicion of infections, in particular those caused by fungi. Finally, it demonstrates how a patient recently treated with etanercept responded well to anti-fungal therapy.
The work should be attributed to: Department of Dermatology and Venereology, Centro Hospitalar de São João EPE, Porto, Portugal.